Last Updated on November 4, 2025 by mcelik
Shoulder injuries are common, hitting athletes and active people hard. A shoulder dislocation is one of the worst, where the humerus pops out of its socket. It’s painful and can leave you wondering how to fix it.Learn how to fix shoulder dislocation safely, including medical and at-home recovery steps.
But, there are ways to fix a shoulder dislocation. Knowing what causes it, its symptoms, and how to treat it can help. This knowledge can help you get your shoulder working right again and prevent future problems.
The shoulder joint is the most mobile in the human body. This makes it prone to dislocations. A shoulder dislocation happens when the humerus moves out of its socket. This can be due to trauma, sports injuries, or falls.
There are different types of shoulder dislocations. Anterior dislocations are the most common. They often result from falls onto an outstretched hand or direct blows to the shoulder. Posterior dislocations are less common and can be caused by seizures or electric shock.

Shoulder dislocations can be caused by traumatic injuries. This includes injuries from sports or car accidents. Falls onto the shoulder or outstretched hand can also lead to dislocation. Conditions like ligament laxity or muscle imbalances can also increase the risk.
Some factors can increase the risk of shoulder dislocations. These include a history of previous dislocations and participation in contact sports. Younger people are also at higher risk due to their activity levels and bone density.
Medical experts say, “Understanding the causes and risk factors of shoulder dislocations is key for prevention and treatment.” Proper diagnosis and treatment can help prevent future dislocations.
Knowing the signs of a dislocated shoulder is key. Look for visual clues, pain patterns, and how well you can move. If you notice these signs, get medical help right away.
A dislocated shoulder is easy to spot. It looks different, maybe even droops. You’ll also see swelling and bruising around the shoulder.
Pain is a big clue. It’s often very sharp and feels like your shoulder is unstable. You might also feel numbness or tingling from nerve damage.
A dislocated shoulder makes moving your arm hard. You might struggle to move it outward or lift it up. To avoid more pain, you might need to keep your arm in a cast.
| Signs/Symptoms | Description |
| Visible Deformity | The shoulder appears out of place or droops. |
| Pain | Intensified pain, often with feelings of instability. |
| Mobility Issues | Difficulty moving the arm, specially outward or above the head. |

When a shoulder dislocation happens, acting fast is key. It helps prevent more harm and eases pain. The steps you take first can greatly affect how well you recover.
Right after a shoulder dislocation, it’s important to keep the arm in place. Use a sling to hold the arm up and keep it from moving. This helps avoid more injury.
Using ice is a good way to lessen pain and swelling. Wrap the ice in a cloth to protect your skin. Apply it for 15-20 minutes, then take a break.
Managing pain well is very important after a shoulder dislocation. You can use pain relievers or anti-inflammatory drugs as needed. Rest and ice also help with pain.
Always follow the right dosage for any medicine. If the pain is too much or you’re worried about the injury, talk to a doctor.
It’s important to know when to get emergency care for a dislocated shoulder. A dislocated shoulder can cause serious problems if not treated right away.
Some symptoms mean you need to go to the emergency room right away. Look out for severe pain, numbness or tingling in your arm or hand. Also, if moving your shoulder or arm is hard, get help fast.
Not getting medical help for a dislocated shoulder can cause big problems. You might get nerve damage, have trouble moving, or keep getting dislocations. You could also face chronic pain and long-term disability.
When you get to the emergency room, doctors will check how bad the dislocation is. They might do a reduction to fix the shoulder. Then, they’ll use immobilization to help it heal. They’ll also make sure you’re not in too much pain.
Fixing a shoulder dislocation needs careful and precise steps. It’s very important to get medical help right away. This helps avoid more serious problems.
Closed reduction is a non-surgical way to fix the shoulder. A doctor carefully moves the humerus back into place. There are different methods, like the Stimson technique and the external rotation method.
The doctor picks the best method based on the patient’s situation and the dislocation type.
Sedation is used to make the process less painful. The level of sedation can range from conscious sedation to deeper levels. The choice depends on the patient’s health, the dislocation’s severity, and the doctor’s opinion.
After fixing the shoulder, a detailed check is done. This ensures the joint is correctly aligned and checks for nerve or blood vessel damage. The check might include X-rays or other tests.
This assessment confirms the procedure’s success and plans the next steps. This could include how to keep the shoulder stable and rehabilitation.
The success of fixing a shoulder dislocation depends on many things. These include how quickly and accurately the procedure is done, and the quality of care after. Good medical steps can greatly lower the risk of problems and improve patient outcomes.
After a shoulder dislocation, many wonder if they should care for it at home or see a doctor. The choice between home care and professional treatment depends on several things. These include the dislocation’s severity, any complications, and the person’s health.
Mild shoulder dislocations might be treated at home. This includes rest, ice, and over-the-counter pain relief. But, it’s important to know when you need a doctor’s help.
Home care strategies include:
Home care is good for mild cases, but it has limits. Without professional help, dislocations can cause nerve damage, chronic instability, and more dislocations.
“It’s essential to seek medical attention if you experience severe pain, numbness, or difficulty moving your shoulder after a dislocation.”
For severe dislocations, fractures, nerve injuries, or if dislocations keep happening, see a doctor. A healthcare professional can diagnose, reduce the dislocation, and suggest rehab.
| Criteria | Home Care | Professional Treatment |
| Severity of Dislocation | Mild | Moderate to Severe |
| Associated Injuries | No associated injuries | Fractures, nerve injuries |
| Recurrence | First-time dislocation | Recurrent dislocations |
In conclusion, home care might work for mild dislocations, but often, you need a doctor. It’s key to talk to a healthcare professional to find the right treatment.
Understanding the severity of shoulder dislocations is key. Imaging helps find the right treatment. It’s all about getting the right diagnosis.
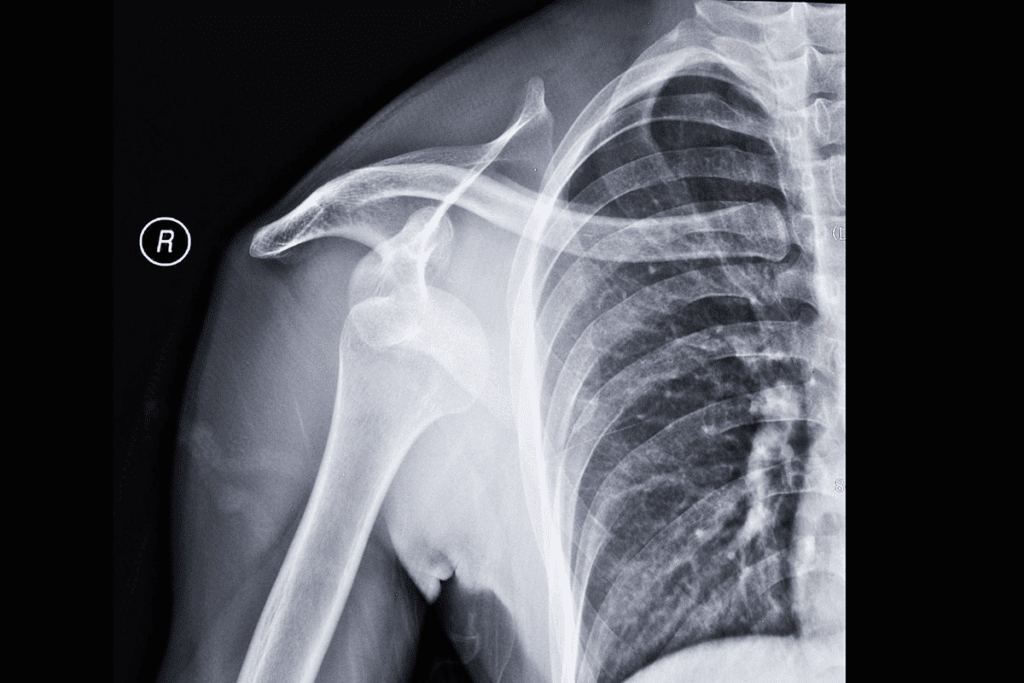
X-rays are often the first choice for shoulder dislocations. They check the humerus’s position and look for fractures. An X-ray can confirm the dislocation and spot complications early.
Magnetic Resonance Imaging (MRI) shows soft tissues like ligaments and tendons. MRI for shoulder dislocation is great for checking the rotator cuff and soft tissue injuries.
Computed Tomography (CT) scans give detailed views of cross-sections. They’re good for complex fractures or when MRI isn’t possible. CT scans for shoulder dislocation help see bony injuries and plan surgery.
| Imaging Technique | Primary Use | Benefits |
| X-ray | Initial assessment of dislocation and fractures | Quick, widely available, and cost-effective |
| MRI | Evaluation of soft tissue injuries | Detailed images of ligaments, tendons, and other soft tissues |
| CT Scan | Assessment of complex fractures and bony injuries | Provides detailed cross-sectional images |
In conclusion, X-rays, MRI, and CT scans are vital for diagnosing and treating shoulder dislocations. Each has its own use and benefits. Together, they help create a complete treatment plan.
After a shoulder dislocation reduction, it’s key to immobilize the shoulder. This helps the injured tissues heal right and lowers the chance of more injuries.
A sling and swath are common for immobilizing the shoulder. A sling holds the arm up, and a swath wraps around the body. This keeps the arm close to the chest, reducing shoulder joint movement.
The time needed for immobilization varies. It depends on how bad the dislocation is and the person’s health. Usually, it lasts from a few days to weeks. Always follow your doctor’s advice to avoid stiffness and help healing.
When it’s time to move again, start slow. Begin with easy exercises to get your range of motion back. Then, move on to strengthening exercises. A physical therapist can make a plan just for you to safely get back to doing things you love.
Here’s what to do to gradually move back to normal:
Managing pain well is key when recovering from a shoulder dislocation. It lets patients do the exercises they need to get better. This helps them heal faster.
For really bad pain, doctors might give stronger meds. These can be opioids or other narcotics. But, they should be used carefully because they can lead to addiction. Always take them exactly as your doctor says.
For milder pain, over-the-counter (OTC) pain relievers like ibuprofen or acetaminophen work well. They help with pain and also cut down on swelling. This is great for shoulder dislocation pain.
There are ways to manage pain without meds too. Physical therapy, using ice or heat, and relaxation methods help. Gentle exercises keep the shoulder moving and less stiff. Ice or heat can ease pain and swelling. Deep breathing or meditation can also help by lowering stress.
Using these methods together can help manage pain well after a shoulder dislocation. It’s important to talk to doctors to find the right plan for you.
Starting rehabilitation early can greatly help those with shoulder dislocations. The main goal is to get the shoulder working right again, lessen pain, and stop future dislocations.
Pendulum exercises are a top pick for early rehab. To do a pendulum exercise, lean forward and let your affected arm hang straight down. Swing your arm in small circles, first clockwise and then counterclockwise. Passive range of motion exercises mean having someone else move your shoulder for you, without you using your muscles.
Isometric strengthening means tightening the muscles around the shoulder without moving it. This helps build strength and stability. For example, you can do isometric shoulder flexion by standing with your affected side against a wall and pushing gently against it.
How fast you move on with rehab depends on how well you’re recovering and how bad the dislocation was. Usually, people can go from gentle pendulum exercises to more active strengthening in 2-6 weeks.
After a shoulder dislocation, advanced rehab is key to getting strength back and avoiding future injuries. These plans help patients get their shoulder fully working again.
Resistance training is vital in shoulder rehab. It makes the muscles around the shoulder stronger, which helps keep it stable. Resistance bands and light weights are often used.
A study in a Journal showed how effective resistance training is. It said progressive overload is key to keep improving muscle strength.
| Exercise | Sets | Reps |
| Resistance Band External Rotations | 3 | 12 |
| Light Weight Shoulder Press | 3 | 10 |
| Scapular Squeezes | 3 | 15 |
The rotator cuff is essential for shoulder stability. Exercises that target these muscles are vital to prevent dislocations. Internal and external rotations are important.
“Strengthening the rotator cuff is not just about preventing injuries; it’s about restoring function and improving the overall quality of life for individuals with shoulder instability.”
A good rotator cuff strengthening program can greatly improve shoulder stability and function. It’s important to start with easy exercises and gradually get harder as the patient gets stronger.
Adding functional movement patterns to rehab helps patients move like normal again. This includes throwing, lifting, and overhead movements that we do every day and in sports.
Functional training not only increases range of motion but also boosts strength and coordination for complex movements. It’s a key step to getting back to normal activities and preventing future shoulder problems.
Surgery might be needed for people with recurring shoulder dislocations or serious instability. Many dislocations can be treated without surgery. But, some need a more serious approach to fix the shoulder and stop future dislocations.
Surgery is usually for those with:
These problems can make daily life hard. Surgery aims to fix these issues and make the shoulder joint more stable.
Several surgeries can treat shoulder dislocations, including:
These surgeries can be done arthroscopically or openly, based on the case and the doctor’s advice.
Recovery from shoulder surgery has several steps:
Recovery can take months. During this time, patients are watched for progress and any issues. A good rehab plan is key for the best results.
Recovering from a shoulder dislocation takes time and understanding. The journey is divided into several phases, each with its own goals and expectations.
In the first few days to weeks, the main focus is on pain management and keeping the shoulder stable. Patients often wear a sling to ease discomfort.
Once the pain starts to lessen, usually in 2-6 weeks, the healing journey begins. This phase involves gradual mobilization and strengthening exercises. These help restore shoulder movement and stability.
The long-term goals, reached in 3-6 months, aim for regaining full strength and function. Patients are encouraged to join advanced rehabilitation protocols. This includes sports-specific training if needed.
Knowing the recovery timeline and milestones is key to a successful rehab. By sticking to a structured plan, individuals can reach their best outcomes and lower the chance of future dislocations.
To stop shoulder dislocations from happening again, we need to do a few things. We must strengthen our muscles, use the right techniques when we’re active, and make some lifestyle changes. These steps can really help keep our shoulders safe and healthy.
Having a good strengthening program is key to avoiding shoulder dislocations. We need to focus on exercises that strengthen the muscles around the shoulder. Rotator cuff strengthening exercises are great because they help keep the shoulder stable and prevent dislocations.
It’s important to use the right technique when we’re being active. We should learn and practice the correct way to move. This helps avoid putting too much strain on our shoulders.
| Activity | Proper Technique |
| Throwing | Step behind the body and use the leg for power |
| Lifting | Keep the object close to the body and lift with the legs |
| Falling | Try to roll with the fall to distribute the impact |
Changing our lifestyle can also help prevent shoulder dislocations. We should keep a healthy weight, not smoke, and eat well to support our muscles and bones.
By making these changes, we can make our shoulders stronger and improve our overall health.
Getting the right treatment is key to recovering from a shoulder dislocation. A good plan includes rest, managing pain, and physical therapy. This helps your shoulder work better and lowers the chance of it happening again.
If your symptoms don’t get better or get worse, see a doctor. Healing from a shoulder dislocation takes time. Be patient.
To keep your shoulder healthy, do strengthening exercises. Also, use the right techniques in sports and make changes in your daily life to avoid injuries. Taking care of your shoulder means you can move freely and easily.
The best method is using a sling and swath. It keeps the shoulder stable and reduces pain.
Recovery time varies. It can take weeks to months, depending on the injury’s severity.
Signs include severe pain, limited mobility, swelling, and a visible deformity.
Minor dislocations might heal with rest and immobilization. But severe cases need medical help for proper healing.
A dislocation is when the bone is completely out of the socket. A subluxation is when it’s only partially out.
Diagnosis involves a physical exam, medical history, and imaging tests like X-rays or MRI.
Not getting medical help can cause nerve damage, chronic instability, and more dislocations.
Yes, physical therapy can improve stability and reduce the risk of future dislocations.
Surgery can provide long-term stability, reduce future dislocation risks, and improve function.
Manage pain with prescription meds, over-the-counter options, ice, and rest.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!