Choosing between frozen embryo transfer and fresh transfer is a big decision. It affects your chances of getting pregnant and your overall experience. Research shows that the best choice depends on your age, how well you respond to fertility meds, and your personal situation.
IVF is a detailed process that includes many steps, from the first visit to the embryo transfer. Knowing the differences between these treatments is key for those looking into fertility options. We’ll dive into the specifics of both, their advantages, and their downsides.
Key Takeaways
- IVF is a broader procedure that encompasses egg retrieval, laboratory fertilization, and embryo development.
- Frozen embryo transfer refers to transferring previously frozen embryos into the uterus.
- The choice between frozen embryo transfer and fresh transfer depends on individual circumstances.
- Recent research reveals that the best option depends on age and response to fertility medications.
- Understanding the differences between these fertility treatments is key for successful fertility outcomes.
The Evolution of Fertility Treatments
Fertility treatments have made huge strides, giving hope to those facing infertility. In vitro fertilization (IVF) is a key success in this area. It has changed how we approach fertility issues.
At least 12 million babies have been born thanks to IVF and other ARTs. This shows how these technologies are helping more people have children.
Growing Prevalence of Assisted Reproductive Technologies
ARTs, led by IVF, are becoming more common. Studies show that success rates depend on factors like age and how well the ovaries respond.
- Increased Accessibility: Better technology and more clinics mean more people can try these treatments.
- Improved Success Rates: New techniques and protocols are making ART more effective.
- Growing Acceptance: Society is becoming more open to ART, reducing the stigma.
Common Reasons People Seek Fertility Treatments
People seek fertility treatments for many reasons. These include:
- Female Infertility Factors: Problems like ovulation issues, endometriosis, and blocked tubes.
- Male Infertility Factors: Issues like low sperm count, poor sperm movement, and other male problems.
- Unexplained Infertility: Cases where the reason for infertility is unknown.
- Age-Related Fertility Decline: Women over 35 facing fertility issues due to age.
Knowing these reasons helps tailor treatments for better success. This includes cases of late implantation successful pregnancy.
What Is In Vitro Fertilization (IVF)?
In vitro fertilization (IVF) is a complex medical process that has changed how we treat infertility. It involves several steps like ovarian stimulation, egg retrieval, fertilization, and embryo culture. These steps aim to help achieve a successful pregnancy.
The Complete IVF Process Explained
The IVF process starts with ovarian stimulation. This is when medications are used to make the ovaries produce many eggs. Then, a minor surgical procedure called egg retrieval is done to collect these eggs.
After that, the eggs are fertilized with sperm in a lab. The resulting embryos are then grown for 3-5 days.
Key steps in the IVF process include:
- Ovarian stimulation
- Egg retrieval
- Fertilization
- Embryo culture
- Embryo transfer
Understanding the IVF process is key, as it can be emotionally and physically tough. People going through IVF may feel a mix of emotions, from hope to anxiety, while waiting to see if it works.
Who Is IVF Recommended For?
IVF is suggested for those facing fertility challenges like blocked fallopian tubes, low sperm count, endometriosis, and unexplained infertility. It’s usually considered after other treatments have failed.
It’s also an option for those who have had issues with late implantation in past treatments. Late implantation can be a worry, but knowing its causes and how it affects IVF success is important.
Typical Timeline for an IVF Cycle
An IVF cycle usually takes about 4-6 weeks. This includes time for ovarian stimulation, egg retrieval, fertilization, embryo culture, and embryo transfer. The exact time can vary based on individual factors and treatment plans.
It’s important to remember that IVF isn’t a sure thing, and it might take more than one cycle to succeed. But, thanks to technology and medical skills, success rates have gone up a lot.
Talking to a fertility specialist about the timeline and what to expect is key. They can offer personalized advice and support, including info on late implantation success stories and what to look forward to.
What Is Frozen Embryo Transfer (FET)?
Frozen Embryo Transfer (FET) is a key part of IVF treatment. It lets doctors transfer frozen embryos into the uterus. This method gives people more chances to get pregnant without needing more egg retrievals.
The FET Procedure Explained
The FET process starts with thawing the frozen embryos. This is done carefully to make sure they survive. After thawing, the embryos are ready for transfer into the uterus.
The transfer is like a fresh embryo transfer. A catheter is used to place the embryo in the uterus.
Preparation for FET includes checking the uterine lining. Hormonal treatment may be used to get it ready. The timing of FET is important and matches the natural or artificial menstrual cycle.
When Is FET Recommended?
FET is suggested in many situations. It’s often used when there are leftover embryos from a previous IVF cycle. It’s also recommended if the woman’s body isn’t ready for a fresh transfer.
It’s a good choice for those who want to delay pregnancy. It’s also used for genetic testing of embryos, allowing for the transfer of healthy embryos.
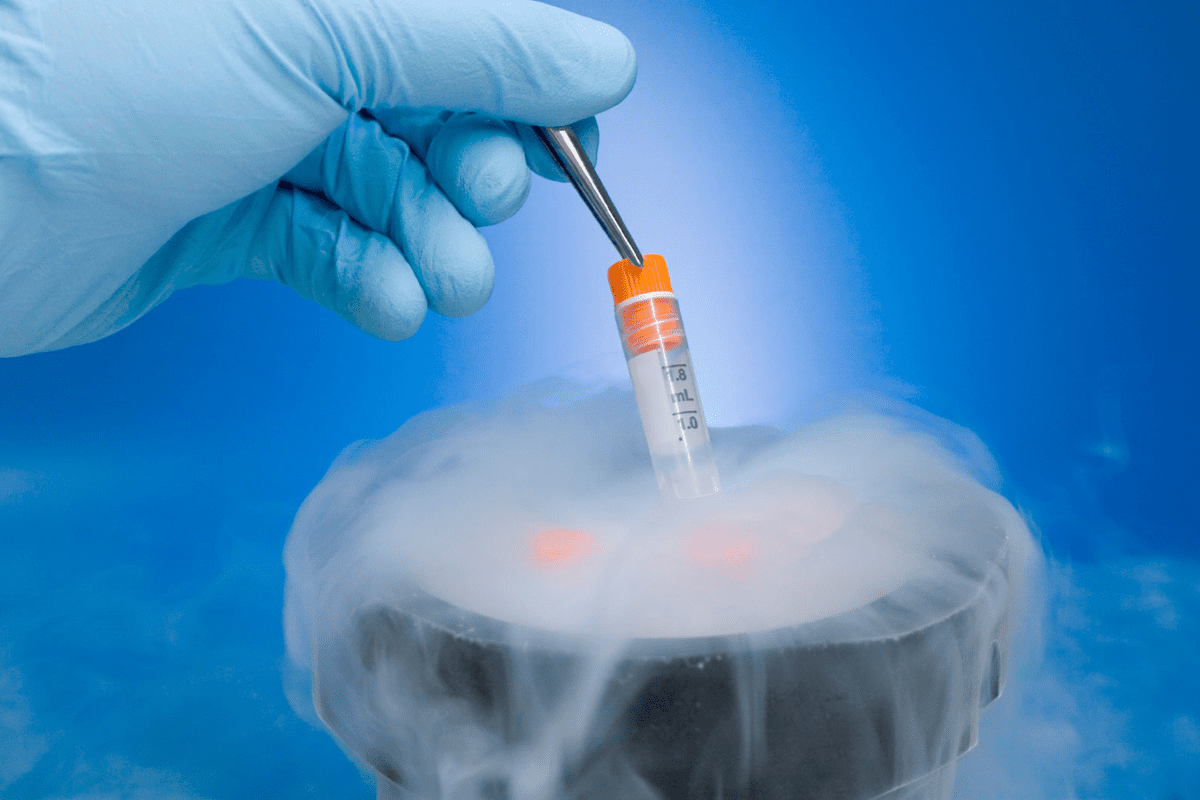
Benefits of Freezing Embryos
Freezing embryos has many advantages. It lets people have multiple transfer attempts without needing more egg retrievals. This saves money and reduces stress.
It also makes family planning easier. People can space out their pregnancies. The success rates of FET are similar to fresh transfers, and sometimes even better.
| Benefits of FET | Description |
|---|---|
| Multiple Transfer Attempts | Allows for multiple chances of pregnancy without additional egg retrieval |
| Flexibility in Family Planning | Enables individuals and couples to plan pregnancies at their convenience |
| Reduced Risk of OHSS | Avoids the risk of ovarian hyperstimulation syndrome associated with fresh transfers |
| Comparable Success Rates | Offers success rates comparable to, or sometimes higher than, fresh embryo transfers |
Understanding FET and its benefits helps people make better choices about fertility treatment. It offers more chances for pregnancy and flexibility in planning a family. FET is a valuable tool in assisted reproductive technology.
Frozen Embryo Transfer vs IVF: Key Differences
It’s important to know the differences between Frozen Embryo Transfer (FET) and IVF. Both are key in fertility treatments but serve different roles. They are part of the broader IVF cycle.
How FET Fits Within the IVF Process
FET is a part of the IVF process, not a separate treatment. In IVF, many embryos are made. Then, the best ones are chosen for transfer, and the rest are frozen for later use.
This makes FET great for those with extra embryos from before. It lets them try again without starting a whole new IVF cycle. This can save time, money, and effort.
Fresh vs. Frozen Transfers: Procedural Differences
Fresh and frozen embryo transfers differ mainly in timing and preparation. Fresh transfers happen right after egg retrieval, in the same IVF cycle. Frozen transfers, on the other hand, can be done at any time, giving more control over when it happens.
For fresh IVF, the uterus gets ready naturally. But for FET, the uterus is prepared with hormones to be ready for the embryo.
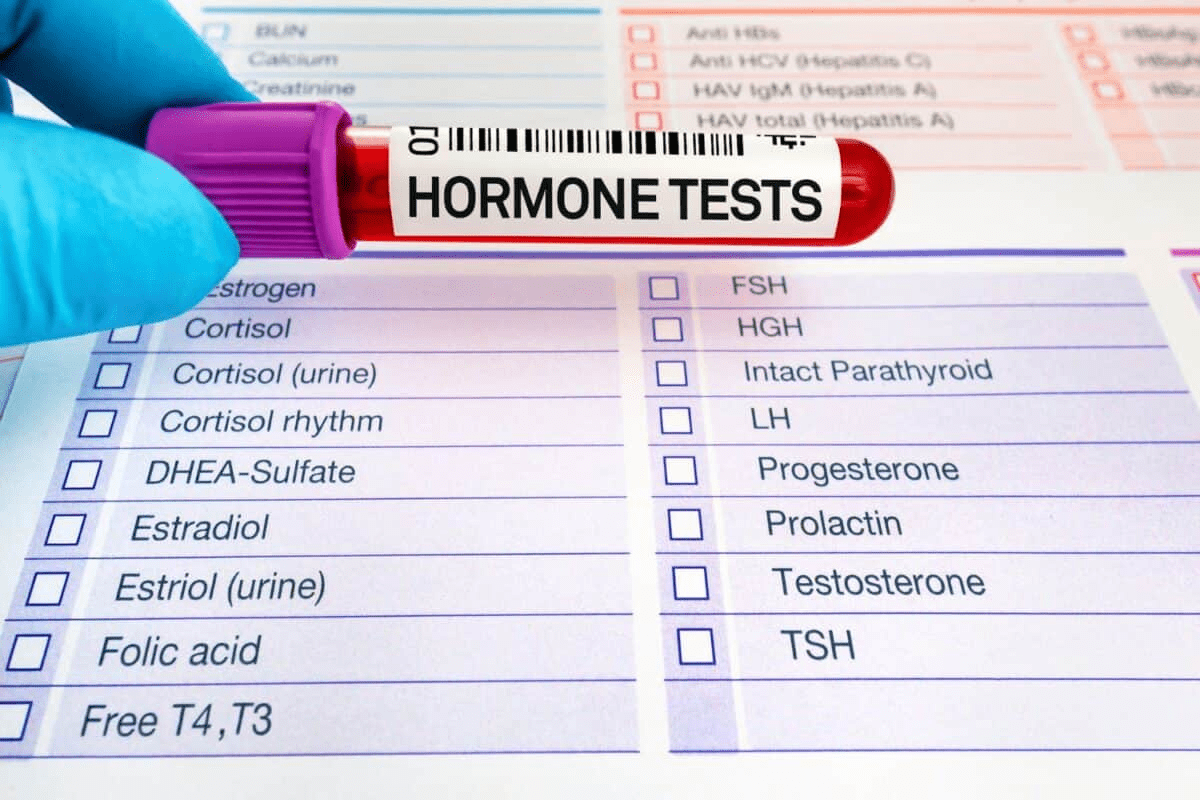
Hormonal Protocols: Fresh IVF vs. FET
The hormone use in fresh IVF and FET is different. Fresh IVF uses strong hormones to get many eggs. FET uses hormones to get the uterus ready for the embryo, like a natural cycle.
This means FET is often easier on the body because it doesn’t need strong hormone stimulation. Knowing these differences helps in making the right choices for fertility treatments.
Success Rates: Fresh vs. Frozen Embryo Transfers
Success rates for fresh and frozen embryo transfers vary. They depend on how well the patient responds and their age. Knowing this helps both patients and doctors make better choices about fertility treatments.
Overall Success Rate Comparisons
Studies show frozen embryo transfers work better for some, while fresh transfers might be better for others. A study in the Fertility and Sterility journal found frozen transfers lead to more live births than fresh ones.
| Treatment Type | Success Rate |
|---|---|
| Fresh Embryo Transfer | 40-50% |
| Frozen Embryo Transfer | 50-60% |
The table shows frozen transfers usually have higher success rates. But, results can differ a lot for each person.
High Responders vs. Low Responders
It’s important to know if you’re a high or low responder. High responders, who make lots of eggs, often do better with frozen transfers.
“The freeze-all strategy has become increasingly popular, even for high responders. It lets them pick the best embryo for transfer,” said Medical Expert, a fertility specialist.
Low responders, who make fewer eggs, might do better with fresh transfers. This is because fresh transfers have less chance of being cancelled.
Age-Related Factors Affecting Success
Age plays a big role in how well embryo transfers work. Women’s age affects egg quality and quantity, which impacts treatment success.
The image shows success rates drop as women get older. This highlights the need to think about age when choosing between fresh and frozen transfers.
In summary, picking between fresh and frozen embryo transfers depends on the patient’s situation. This includes how well they respond to treatment and their age. Understanding these factors helps patients make informed choices about their fertility treatments.
The Implantation Process After Embryo Transfer
After an embryo transfer, the implantation process is complex. It involves the embryo attaching to the uterine lining. This is a key step for getting pregnant through IVF or FET.
When Does Implantation Typically Occur?
Implantation usually happens 6-10 days after fertilization. The embryo moves from the fallopian tube to the uterus. There, it starts to attach to the uterine lining.
This process is made possible by detailed interactions between the embryo and the uterine environment. Knowing when implantation happens can help patients understand their fertility journey better. It’s a time that needs patience and careful watching for the best results.
Understanding Late Implantation
Late implantation means the embryo implants later than usual. It’s important to know that late implantation doesn’t always mean a lower chance of getting pregnant.
Things that can cause late implantation include the embryo’s quality, how ready the uterine lining is, and how each person’s body reacts. We’ll look into these factors more to give a full picture.
Signs of Successful Implantation
Successful implantation can show in different ways, but not everyone notices. Some signs are mild cramping, spotting, and changes in cervical mucus. Yet, many women don’t feel anything.
The best sign of successful implantation is a positive pregnancy test, usually two weeks after the embryo transfer. It’s key to follow the fertility specialist’s advice on testing and care.
Understanding the implantation process helps patients see the complexity of getting pregnant through IVF or FET. Our team is here to support you every step of the way.
Late Implantation in Frozen Embryo Transfers
Late implantation is a phenomenon that can happen during frozen embryo transfers. It raises questions about its impact on pregnancy success. The usual implantation window is well understood, but variations can occur. Fertility specialists and patients should be aware of late implantation.
What Is Considered Late Implantation?
Late implantation is when the embryo implants more than 10 days after fertilization. This delay can worry many people going through fertility treatments. Knowing the norms and variations in implantation timing is key for managing expectations and making informed decisions about fertility care.
Research shows that late implantation can happen in both fresh and frozen embryo transfers. The frequency and implications may differ. A study found that “The incidence of late implantation was found to be higher in frozen embryo transfers compared to fresh transfers”
“The incidence of late implantation was found to be higher in frozen embryo transfers compared to fresh transfers”
Causes of Delayed Implantation
Several factors can cause delayed implantation. These include hormonal influences, the quality of the embryo, and the receptivity of the uterine lining. “Hormonal protocols used in fertility treatments can affect the timing of implantation,” says Medical Expert, a fertility specialist. The synchronization between embryo development and uterine preparation is critical.
- Hormonal influences
- Embryo quality
- Uterine receptivity
Late Implantation Success Stories
Despite concerns, there are many success stories with late implantation. Many women have had successful pregnancies after late implantation. This shows the complexity and variability of the human reproductive process. “I had a successful pregnancy after a late implantation,” shares Sarah, a patient who underwent frozen embryo transfer. Her story is a testament to the fact that late implantation can lead to a healthy pregnancy.
| Category | Success Rate | Implantation Timing |
|---|---|---|
| Fresh Embryo Transfer | 60% | Typical |
| Frozen Embryo Transfer | 55% | Late |
Is Late Implantation a Concern?
While late implantation may raise concerns, it’s not necessarily a negative sign for pregnancy success. The key is understanding the underlying factors and working closely with fertility specialists. We recommend discussing any concerns about late implantation with your healthcare provider to get personalized advice and care.
Making the Choice: Fresh Transfer or FET
Choosing between fresh and frozen embryo transfers depends on many factors. These include medical reasons and personal preferences. It’s important to understand these factors to make a choice that fits your situation.
Medical Considerations for Your Decision
Medical factors are key in deciding between fresh and frozen embryo transfers. Things like how your ovaries respond, the risk of ovarian hyperstimulation syndrome (OHSS), and how ready your uterine lining is are important.
- Ovarian Response: High responders might prefer frozen transfers to avoid OHSS.
- Endometrial Receptivity: The state of your uterine lining can impact success. Frozen transfers might offer a better environment.
A study in the Fertility and Sterility journal found frozen transfers can be more natural. This might improve implantation rates for some.
“The shift towards frozen embryo transfers has been driven by improvements in cryopreservation techniques and a better understanding of the factors influencing implantation.”
| Consideration | Fresh Transfer | Frozen Transfer |
|---|---|---|
| Ovarian Response | Risk of OHSS | Reduced risk of OHSS |
| Endometrial Receptivity | Potential for less optimal uterine environment | More control over uterine preparation |
Personal Factors to Consider
Personal factors also play a role in choosing between fresh and frozen embryo transfers. These include:
- Timing: Frozen transfers offer more scheduling flexibility.
- Emotional Readiness: Some prefer the immediacy of fresh transfers, while others like the preparation of frozen transfers.
Discussing Options With Your Fertility Specialist
Ultimately, your fertility specialist should help you decide between fresh and frozen embryo transfers. They can give advice based on your medical history and current health.
Talking about your options and understanding the implications can help you make a choice that’s right for you.
Conclusion: Navigating Your Fertility Journey
Understanding your fertility journey can be tough and emotional. Knowing the difference between frozen embryo transfer (FET) and IVF is key. It helps patients make choices that fit their needs and situations.
Implantation after frozen blastocyst transfer is a big step in FET. While it usually happens within a certain time, some people may implant later. It’s important to remember that late implantation is not rare. The timing can vary a lot from person to person.
Every person’s fertility journey is different. What works for one might not work for another. We aim to give our patients all the information and support they need. This way, they can make informed choices and feel confident on their fertility journey.
FAQ
What is the difference between frozen embryo transfer and IVF?
IVF is a big process with many steps. It starts with a first meeting and ends with the embryo transfer. Frozen embryo transfer is just one part of IVF. It involves putting frozen embryos into the uterus.
What is considered late implantation?
Late implantation happens when an embryo implants later than usual. This often happens after a frozen embryo transfer.
What causes late implantation?
Many things can cause late implantation. Hormonal changes, how ready the uterus is, and how well the embryo is developing are some reasons.
Is late implantation a bad sign?
No, late implantation doesn’t always mean trouble. Many babies have been born after late implantation.
How late can implantation happen?
Implantation can happen up to 10-12 days after transferring an embryo. But usually, it happens between 6-10 days.
What are the signs of successful implantation?
Signs of successful implantation include mild cramping, spotting, and changes in cervical mucus. But some women might not notice anything.
What is the success rate of frozen embryo transfer compared to fresh embryo transfer?
Success rates for frozen and fresh embryo transfers vary. They depend on things like age, embryo quality, and how ready the uterus is.
When is frozen embryo transfer recommended?
Frozen embryo transfer is often suggested for those with extra embryos from a previous cycle. It’s also for those who need to delay transfer for medical or personal reasons.
How does the IVF process work?
IVF has many steps. These include stimulating the ovaries, retrieving eggs, fertilizing them, growing the embryos, and transferring them.
What are the benefits of freezing embryos?
Freezing embryos means you can use them later. It avoids the need for more egg retrieval and fertilization. It also helps preserve fertility for those undergoing treatments that might harm their reproductive health.
What are the hormonal protocols used in fresh IVF versus FET?
Fresh IVF uses hormones to grow eggs. FET cycles use a simpler protocol to get the uterus ready for implantation.
How do I choose between fresh transfer and FET?
Choosing between fresh transfer and FET depends on many factors. These include how well the ovaries respond, how ready the uterus is, and personal preferences. It’s best to talk to a fertility specialist.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8489809/