Last Updated on December 1, 2025 by Bilal Hasdemir
Spinal fusion surgery is a significant medical procedure. It joins two or more vertebrae together. This complex procedure is often needed to ease chronic back pain and stabilize the spine. Every year, thousands of people have this surgery to find relief from severe spinal issues.Are fusion procedures spinal considered major surgery? We reveal the surprising truth. Get the definitive answer.
So, is spinal fusion a major surgery? Yes, it is. It needs a long recovery time, and patients must be careful to avoid problems. It’s important for those thinking about this operation to understand spinal fusion recovery and spinal fusion complications.
Key Takeaways
- Spinal fusion surgery is a complex operation that involves fusing vertebrae.
- The surgery is considered major due to its complexity and recovery time.
- Understanding possible complications is key for patient preparation.
- Spinal fusion recovery requires careful post-operative care.
- Patients should know the risks and benefits before surgery.
What Makes Spinal Fusion a Major Surgical Procedure
Spinal fusion surgery is a significant medical procedure.because it’s complex and affects the body a lot. This operation is detailed and impacts many body systems. It also needs a lot of recovery time, making it a major surgery.
Complexity of the Procedure
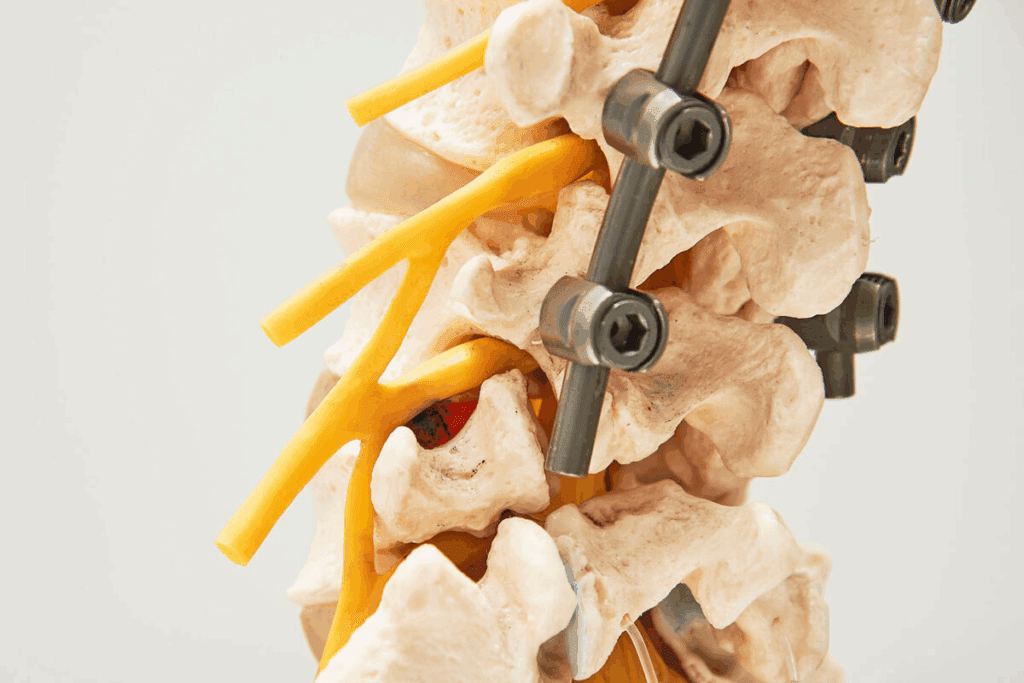
Spinal fusion joins vertebrae together using bone grafts, rods, and screws. It’s a precise process that needs a deep understanding of the spine. The surgery can be done in different ways, each with its own challenges.
“The complexity of spinal fusion surgery is not just in the technical skill required but also in understanding the patient’s specific condition and tailoring the procedure,” says a renowned spinal surgeon.
Impact on Body Systems
Spinal fusion surgery doesn’t just affect the spine. It can also harm the nervous system, causing nerve damage or irritation. It can also change how the body moves and stands.
Recovery Requirements
Recovering from spinal fusion surgery takes a lot of time and planning. Patients often need physical therapy to get back their strength and mobility. The cost of this surgery is high, so understanding the recovery is key to a good outcome.
Good spinal fusion rehabilitation involves many steps. This includes managing pain, physical therapy, and sometimes mental support to deal with recovery challenges.
Understanding Spinal Anatomy and Function
It’s key to know how the spine works and its parts. The spine, or backbone, is made up of many elements. These elements help support, stabilize, and move the body.
Vertebrae, Discs, and Nerves
The spine has 33 vertebrae in five areas: cervical, thoracic, lumbar, sacrum, and coccyx. Between these vertebrae are intervertebral discs, which absorb shock and help the spine move. Nerves from the spinal canal send signals to the brain and body.
How the Healthy Spine Works
A healthy spine supports the body, allows movement, and protects the spinal cord. Vertebrae, discs, and ligaments work together. They keep posture, absorb shock, and help us move.
When the spine is hurt or sick, it can cause pain and disability. This might mean needing surgery like spinal fusion. Spinal fusion joins vertebrae to stabilize the spine, ease pain, and improve function. It’s often used for the lumbar spine and other areas.
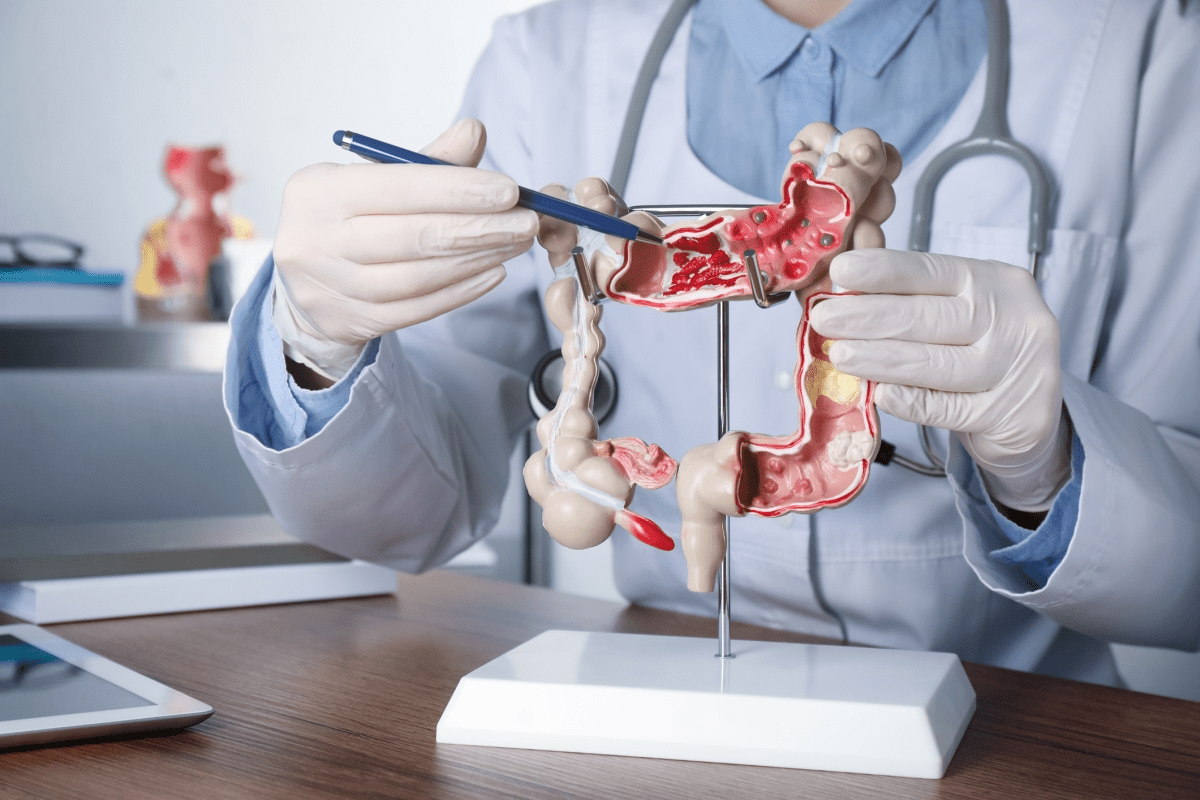
Common Conditions Requiring Spinal Fusion
Many spinal disorders and injuries need spinal fusion to stabilize the spine. This surgery joins two or more vertebrae together. It helps stop movement between them, easing pain and stabilizing the spine.
Degenerative Disc Disease
Degenerative disc disease happens when spinal discs wear out over time. This can cause pain, inflammation, and spine instability. If other treatments don’t work, spinal fusion might be needed to stabilize the spine and reduce pain.
Spinal Stenosis
Spinal stenosis is when the spinal canal narrows. This puts pressure on the spinal cord and nerves. It can cause back, leg, or arm pain, numbness, and weakness. If other treatments don’t help, surgery might be needed to relieve pressure and stabilize the spine.
“Spinal stenosis is a significant cause of disability in the elderly, and surgical intervention can greatly improve quality of life.”
Spondylolisthesis
Spondylolisthesis is when a vertebra slips forward over another. This can cause pain and discomfort. Spinal fusion is often recommended to stabilize the vertebrae and prevent further slippage.
Fractures and Deformities
Spinal fractures, often from osteoporosis or trauma, might need spinal fusion. Spinal deformities like scoliosis or kyphosis also might require surgery. This is to correct the alignment and stabilize the spine.
| Condition | Description | Treatment |
| Degenerative Disc Disease | Wear and tear on spinal discs | Spinal Fusion |
| Spinal Stenosis | Narrowing of the spinal canal | Decompression with Spinal Fusion |
| Spondylolisthesis | Vertebra slips over another | Spinal Fusion |
| Fractures and Deformities | Spinal fractures or deformities | Spinal Fusion |
It’s important to know about these conditions and their treatments. Spinal fusion can greatly improve a patient’s life by addressing spinal instability or pain.
Fusion Procedures Spinal: Types and Techniques

Spinal fusion surgery uses many techniques, each with its own benefits and challenges. The right technique depends on the patient’s health, the spine area, and the surgeon’s skill.
Anterior Approaches
Anterior spinal fusion goes through the front of the body. It’s often used for the lumbar and cervical spine. Anterior lumbar interbody fusion (ALIF) treats degenerative disc disease well. It lets surgeons directly access the disc space for removal and implantation.
Anterior methods can be less invasive, leading to quicker recovery. But, they also come with risks like blood vessel or nerve damage.
Posterior Approaches
Posterior spinal fusion goes through the back. It’s common for thoracic and lumbar surgeries. Posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF) help stabilize and fuse the spine.
Posterior methods let surgeons directly work on the spine’s back parts. This is good for correcting deformities. But, it can cause more tissue damage and longer recovery times.
Lateral Approaches
Lateral spinal fusion accesses the spine from the side. Lateral lumbar interbody fusion (LLIF), or extreme lateral interbody fusion (XLIF), is a minimally invasive method. It inserts implants or bone grafts with little tissue disruption.
Lateral methods reduce nerve damage risk and postoperative pain. Yet, they need special training and tools. They might not fit all patients or conditions.
In summary, the spinal fusion procedure type varies based on the patient’s condition, spine location, and surgeon’s skill. Knowing the different techniques helps patients make better choices for their care.
Minimally Invasive Spinal Fusion Techniques
Spinal surgery has made big strides with new, less invasive methods. These techniques aim to cause less damage, reduce scarring, and help patients heal faster. They keep the benefits of traditional spinal fusion surgery.
Advantages of Minimally Invasive Approaches
Minimally invasive spinal fusion has many benefits over traditional surgery. Smaller incisions mean less damage to tissues and muscles. This leads to less pain and faster recovery times.
These methods also mean less blood loss and a lower chance of infection. Patients usually spend less time in the hospital and can get back to their daily activities sooner.
They also have less scarring, which is important for many patients.
Endoscopic Techniques
Endoscopic spinal fusion uses a thin, flexible tube with a camera and light. It lets surgeons see the area they’re working on. This way, they can make small incisions and cause less damage.
Using endoscopic techniques needs special training and tools. But, when done by skilled surgeons, it can lead to great results with few problems.
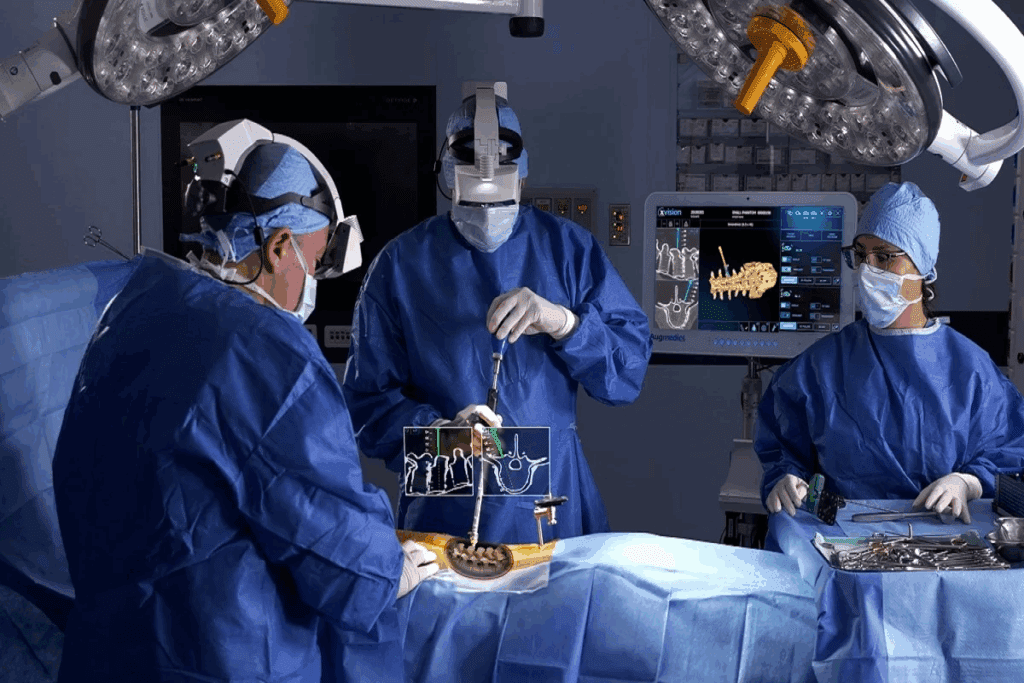
Robotic-Assisted Spinal Fusion
Robotic-assisted spinal fusion is another big step forward. It gives surgeons more precision and control. This means they can place implants more accurately, leading to better results.
The robotic system provides real-time images and feedback. This lets surgeons make changes during the surgery. It can improve fusion rates and lower the risk of complications.
Candidacy for Minimally Invasive Procedures
Not every patient is right for these new spinal fusion methods. The choice depends on the patient’s condition, health, and past surgeries.
Doctors look at each case carefully. They consider the complexity of the spinal issue, any anatomical problems, and the patient’s health. They use scans like MRI or CT to decide the best surgery plan.
The Surgical Process: What to Expect
Learning about spinal fusion surgery can help reduce your anxiety. We’ll walk you through the key steps, from the pre-surgical check to post-operative care. This way, you’ll know what to expect every step of the way.
Pre-Surgical Evaluation and Testing
Before surgery, a detailed check-up is done to evaluate your health and spine condition. This includes:
- Detailed medical history review
- Physical examination
- Imaging tests (X-rays, MRI, CT scans)
- Laboratory tests (blood work, etc.)
These tests help us identify risks and plan the best surgery for you.
Anesthesia Considerations
Spinal fusion surgery is usually done under general anesthesia. This keeps you comfortable and pain-free. Our anesthesiologists work with your surgical team to:
- Assess your anesthesia needs based on your medical history and current health
- Monitor your vital signs during surgery
- Adjust anesthesia levels as necessary to maintain your safety and comfort
We take careful steps to ensure a successful surgery and minimize risks.
Step-by-Step Surgical Procedure
The spinal fusion surgery involves several steps:
- Incision and exposure: The surgical site is accessed through an incision, and the necessary tissues are gently retracted to expose the spine.
- Decompression (if necessary): Any compressed nerves or spinal cord are relieved.
- Spinal realignment and stabilization: The spine is realigned, and the affected vertebrae are stabilized.
- Bone grafting: A bone graft is placed to facilitate fusion between the vertebrae.
- Instrumentation (if used): Spinal instrumentation (such as rods and screws) may be used to provide additional stability.
Our surgical team is highly experienced in performing these complex procedures with precision and care.
Immediate Post-Operative Care
After surgery, you’ll be in the recovery room. Our team will monitor your:
- Pain levels and manage pain effectively
- Vital signs to ensure stability
- Neurological status to check for any nerve function changes
We focus on your comfort and safety during the immediate post-operative period. We provide the necessary care to help you start your recovery.
Understanding the spinal fusion surgery process helps you prepare better. Our team is dedicated to giving you the best care and support throughout your treatment.
Spinal Fusion Recovery Timeline
Knowing how long it takes to recover from spinal fusion surgery is key. It helps set realistic goals and makes the healing process smoother. Everyone recovers at their own pace, but here’s a general guide to help.
Hospital Stay Duration
The time spent in the hospital after surgery can range from 1 to 4 days. This depends on the surgery’s complexity and the patient’s health. During this time, doctors watch over the patient, manage pain, and start the healing process. Managing pain well in the hospital is important for comfort and to start moving early.
First Six Weeks After Surgery
The first six weeks are very important for getting better. Patients should not lift, bend, or twist too much. They can start doing light tasks in 4 to 6 weeks. Following the doctor’s instructions closely is key to avoid problems and help the body heal.
Three to Six Months Post-Surgery
Between three to six months, patients usually see big improvements. They can usually go back to their normal life, including work, but some might have some limits. Physical therapy is very important during this time. It helps regain strength, flexibility, and movement.
Long-Term Recovery (One Year and Beyond)
Recovering fully from spinal fusion surgery can take up to a year or more. The fusion itself might take 6 to 12 months to fully heal. But, patients often see more improvements in their symptoms and abilities after that. Regular check-ups with the healthcare team are vital to track progress and handle any issues.
Understanding the spinal fusion recovery timeline helps patients prepare better. It leads to a better outcome and a higher quality of life.
Rehabilitation After Spinal Fusion
Rehabilitation after spinal fusion surgery is key to recovery. It helps patients regain strength, mobility, and function. This leads to the best possible outcome from surgery.
Physical Therapy Protocols
Physical therapy is essential after spinal fusion. We create a personalized exercise program for each patient. This program promotes healing, improves flexibility, and strengthens the muscles around the spine.
The physical therapy protocol includes various exercises. These are:
- Gentle stretching to improve flexibility
- Strengthening exercises for core and back muscles
- Low-impact aerobic activities like walking or swimming
- Posture education and body mechanics training
A typical physical therapy regimen lasts several months. The frequency and intensity of sessions change based on the patient’s progress.
Activity Restrictions and Modifications
After spinal fusion surgery, some activity restrictions are needed. These ensure proper healing and reduce the risk of complications. We advise patients on safe daily activities and physical exertion levels.
Common activity restrictions include:
| Activity | Restriction | Duration |
| Lifting | Avoid lifting heavy objects (>10 lbs) | 6-12 weeks |
| Bending | Limit bending at the waist | 6-8 weeks |
| Twisting | Avoid twisting or rotating torso | 8-12 weeks |
| Driving | Avoid driving until cleared by surgeon | Varies |
Return to Work Considerations
The timeline for returning to work after spinal fusion surgery varies. It depends on the job’s nature and the patient’s recovery. We help patients determine when it’s safe to go back to work.
Factors influencing return to work include:
- The physical demands of the job
- The patient’s overall health and recovery pace
- The presence of any job-related risk factors for re-injury
Patients with physically demanding jobs may need a longer recovery before returning to full duty.
Potential Complications and Risks
It’s important for patients to know about the risks of spinal fusion surgery. This surgery can help with many spinal problems. But, it’s key to know the possible complications that can happen.
Surgical Complications
Complications during surgery can include infection, bleeding, and nerve damage. Infection is a risk with any surgery, including spinal fusion. Antibiotics are often used to minimize this risk. Bleeding can happen, and sometimes it’s serious enough to need a blood transfusion.
Nerve damage is another risk. It can cause numbness, weakness, or pain. To reduce these risks, surgeons use advanced techniques and monitoring during the procedure. For example, neuromonitoring can catch nerve damage early, allowing for quick action.
Medical Complications
After surgery, patients might face complications like deep vein thrombosis (DVT), pulmonary embolism, and respiratory or cardiac issues. DVT is a blood clot in the deep veins, usually in the legs. It can be dangerous if it breaks loose and goes to the lungs, causing a pulmonary embolism. Patients are often encouraged to move around soon after surgery to reduce the risk of DVT.
- Respiratory complications can occur, specially in patients with pre-existing lung conditions.
- Cardiac issues, such as heart attack or arrhythmia, can also arise, specially in older patients or those with heart disease.
Long-Term Complications
Long-term issues can include adjacent segment disease and hardware failure. Adjacent segment disease is when the vertebrae next to the fused segment degenerate faster. Hardware failure is when the rods, screws, or other devices used in the fusion fail or become loose. Regular follow-up with a healthcare provider is key to monitor for these long-term complications.
Risk Factors for Complications
Some factors can increase the risk of complications. These include older age, obesity, smoking, and pre-existing medical conditions like diabetes or heart disease. Patients can reduce their risk by maintaining a healthy lifestyle, including quitting smoking and managing chronic conditions.
Knowing about these risks helps patients make better decisions about their treatment. They can work closely with their healthcare providers to lower these risks.
Success Rates and Outcomes
It’s important to know how well spinal fusion surgery works. This surgery helps people with back problems feel better and move easier. It’s a big step, and knowing what to expect is key.
Measuring Surgical Success
Spinal fusion success is measured in many ways. Doctors look at how well the spine heals and how much pain goes away. They also check if patients can do more things than before.
But it’s not just about numbers. How happy patients are and how well they live their lives matters a lot too.
Factors Affecting Outcomes
Many things can change how well spinal fusion works. Here are a few:
- Patient Selection: Choosing the right patient is very important. Doctors look at age, health, and the type of back problem.
- Surgical Technique: The way the surgery is done can make a big difference. New tools and methods can help a lot.
- Surgeon Experience: The skill of the surgeon is very important. More experienced doctors usually get better results.
- Post-Operative Care: How well a patient recovers is also key. Good care after surgery helps a lot.
A study in a top orthopedic journal said, “The success of spinal fusion surgery depends on choosing the right patient, doing the surgery well, and taking good care after.”
“The success of spinal fusion surgery is highly dependent on a combination of proper patient selection, meticulous surgical technique, and extensive post-operative care.”
Quality of Life Improvements
Spinal fusion surgery can really improve life for many people. It helps with pain, makes the spine stable, and improves movement. This means patients can:
- Feel less pain
- Move around more easily
- Sleep better
- Do more things every day
These changes make life better, letting patients enjoy their daily activities and live more actively.
Cost Considerations for Spinal Fusion
It’s important for patients to know the costs of spinal fusion surgery. The price can change based on several things. These include the surgery’s complexity, the doctor’s fees, and where it’s done.
Average Costs in the United States
In the U.S., spinal fusion surgery can cost between $80,000 and over $150,000 for one level. This price includes:
- Surgeon’s fees
- Hospital charges
- Anesthesia fees
- Pre-operative testing
- Post-operative care
A study found the average cost is about $100,000. But, costs can vary based on the case.
Insurance Coverage and Requirements
Insurance for spinal fusion surgery varies by provider and policy. Most plans cover it, but the details differ. Patients should:
- Check their policy for coverage.
- Get pre-approval for the surgery.
- Know any costs they’ll have to pay out-of-pocket.
“It’s key for patients to talk to their insurance about what’s covered and any pre-approval needs.”
Financial Assistance Options
For those struggling financially, there are ways to help with spinal fusion surgery costs. These include:
- Payment plans from hospitals or surgical centers
- Financial help programs for those who qualify
- Support from non-profit groups for medical expenses
Patients should ask about these options when talking to their healthcare team.
“The cost of spinal fusion surgery shouldn’t stop patients from getting the treatment they need. Looking into financial help can make it more affordable.”
Alternatives to Spinal Fusion
Choosing spinal fusion surgery should be a last resort. First, look at conservative treatments and less invasive options. Patients want solutions that are safe and quick to recover from.
Conservative Treatments
Many start with non-surgical methods. These include:
- Physical therapy to improve flexibility and strength
- Medications such as NSAIDs or muscle relaxants to manage pain
- Epidural steroid injections to reduce inflammation
- Lifestyle modifications, including weight loss and smoking cessation
These treatments can be used together. They help manage symptoms and improve life quality.
Minimally Invasive Non-Fusion Procedures
Some patients prefer less invasive options. These include:
- Discectomy: Removing a damaged disc
- Laminectomy: Relieving pressure on the spinal cord
- Interspinous process decompression: Creating space between vertebrae
These methods aim to reduce symptoms with less damage and faster recovery than fusion.
Emerging Technologies and Treatments
New medical technologies are emerging. They offer alternatives to spinal fusion. Some include:
| Treatment | Description | Potential Benefits |
| Artificial Disc Replacement | Replacing a damaged disc with an artificial one | Preserves motion, potentially reducing wear on adjacent discs |
| Spinal Cord Stimulation | Implanting a device that delivers electrical impulses to the spinal cord | Can reduce chronic pain |
| Biologics and Stem Cell Therapy | Using biological materials to promote healing | May enhance natural repair processes |
These new technologies show promise. They are being studied for their safety and effectiveness.
Choosing the Right Surgeon and Facility
Success in spinal fusion surgery depends on picking a skilled surgeon and a top-notch medical facility. It’s key for patients to be well-informed and active in picking the right healthcare team for this complex surgery.
Surgeon Qualifications and Experience
For spinal fusion, your surgeon’s skill is essential. Find a surgeon who is board-certified in orthopedic or neurosurgery and specializes in spinal issues. It’s important to know their experience with spinal fusion surgeries, including their success and complication rates.
A leading medical expert says, “The more experienced the surgeon, the better they can handle unexpected problems and improve patient results.”
- Check for fellowship training in spinal surgery
- Inquire about their experience with your specific condition
- Ask to see before-and-after photos of previous patients
Hospital Quality Metrics
The quality of the hospital or surgical center is vital for your care. Look into the facility’s quality metrics, like infection rates, readmission rates, and patient satisfaction scores.
“Hospitals with good quality metrics usually have better patient outcomes,” a recent healthcare study found.
| Quality Metric | What to Look For |
| Infection Rates | Lower rates mean better infection control |
| Readmission Rates | Lower rates show effective post-operative care |
| Patient Satisfaction | High scores mean good patient care and experience |
Questions to Ask Before Surgery
Before deciding on spinal fusion surgery, ask the right questions. Make a list of questions to talk over with your surgeon and healthcare team.
- What are the risks and benefits specific to my condition?
- What are the alternatives to spinal fusion, and why is this procedure recommended for me?
- Can I see your credentials and experience with spinal fusion?
- What is the expected recovery process, and what support will I receive?
Being informed and proactive helps patients make the best choices for their spinal health. Remember, picking the right surgeon and facility is a key step in your recovery journey.
Conclusion
Spinal fusion surgery is a significant medical procedure. It needs a lot of thought and getting ready. We’ve looked at many parts of spinal fusion, like its types, how it’s done, recovery, and possible problems.
Understanding spinal fusion is key. It helps patients know what to do from the start to the long recovery. Knowing about spinal fusion helps patients choose the right treatment.
We’ve used lots of sources to give a full view of spinal fusion surgery. This knowledge helps patients feel ready for their treatment. They know what’s coming and how to get ready for the good and bad parts of spinal fusion surgery.
FAQ
What is spinal fusion surgery?
Spinal fusion surgery is a complex procedure. It joins two or more vertebrae together. This is done using bone grafts, rods, and screws. It stabilizes the spine and relieves pain.
Is spinal fusion considered major surgery?
Yes, it is. Spinal fusion is complex and carries risks. It has a big impact on the body.
What are the common conditions that require spinal fusion surgery?
Conditions like degenerative disc disease and spinal stenosis may need it. Spondylolisthesis, fractures, and deformities also require this surgery.
What are the different types of spinal fusion techniques?
There are several techniques. These include anterior, posterior, and lateral approaches. Minimally invasive methods like endoscopic and robotic-assisted procedures are also used.
What is the recovery process like after spinal fusion surgery?
Recovery starts with a hospital stay. Then, several weeks or months of rehabilitation follow. This includes physical therapy and activity restrictions.
What are the possible complications and risks of spinal fusion surgery?
Complications can include surgical and medical issues. Long-term risks are infection, nerve damage, and hardware failure.
How successful is spinal fusion surgery?
Success depends on the condition, patient health, and surgeon’s skill. Each case is different.
What are the costs associated with spinal fusion surgery?
Costs vary widely. They depend on location, insurance, and procedure complexity.
Are there alternatives to spinal fusion surgery?
Yes, there are. Alternatives include conservative therapies and minimally invasive procedures. New technologies are also emerging.
How do I choose the right surgeon and facility for spinal fusion surgery?
Look at the surgeon’s qualifications and experience. Check hospital quality metrics. Ask about the procedure and care.
What is the role of physical therapy in spinal fusion recovery?
Physical therapy is key. It helps patients regain strength, mobility, and function.
Can I return to work after spinal fusion surgery?
Yes, but timing and type of work vary. It depends on surgery extent and recovery progress.
How long does it take to fully recover from spinal fusion surgery?
Recovery can take months to a year or more. It varies based on individual factors.
References
National Center for Biotechnology Information. Spinal Fusion Major Surgery Procedure and Recovery. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7797794/