Last Updated on December 1, 2025 by Bilal Hasdemir

Did you know over 400,000 spinal fusion surgeries happen every year in the U.S.? Spinal fusion surgery might help some spinal conditions. But, it also has big risks and problems that can really affect your life fusion procedures spinal.
Thinking about vertebral fusion or spine fusion can be scary. It’s key to think about the good and bad sides before deciding. We’ll talk about why back surgery should be a last resort and what else you can try.
Key Takeaways
- Understanding the risks associated with spinal fusion surgery.
- Exploring alternative treatments to spine fusion.
- Learning when spinal fusion is absolutely necessary.
- Discovering ways to manage back pain without surgery.
- Understanding the long-term implications of fused vertebrae in the spine.
Understanding Spinal Fusion Surgery
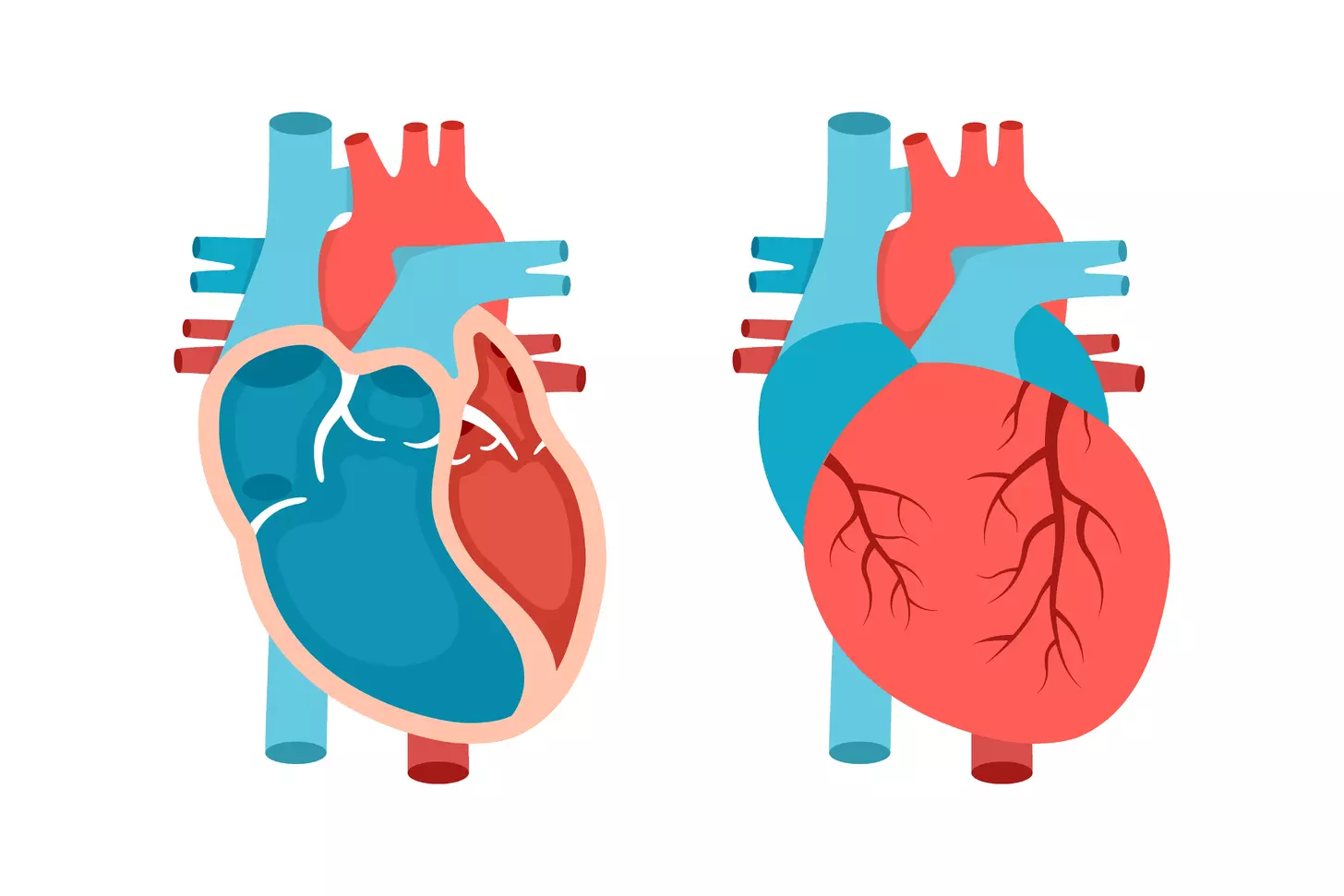
Spinal fusion surgery is a common treatment for many spinal problems. It uses rods, screws, and cages to join vertebrae together. This helps to reduce pain and stabilize the spine.
What Is Spinal Fusion?
Spinal fusion is a surgery that joins two or more vertebrae together. It uses bone grafts, rods, screws, and other devices. The goal is to stabilize the spine, reduce pain, and stop further damage.
The process starts with preparing the vertebrae to be fused. This means removing any damaged parts and getting ready for the bone graft. The bone graft, from the patient or a donor, is then placed between the vertebrae to help them fuse.
Common Types of Spinal Fusion Procedures
There are several types of spinal fusion procedures. Each has its own purpose and method:
- Posterior Lumbar Interbody Fusion (PLIF): This method approaches the spine from the back. It uses bone grafts and hardware to fuse the vertebrae.
- Anterior Lumbar Interbody Fusion (ALIF): This procedure comes from the front. It removes the damaged disc and fuses the vertebrae.
- Transforaminal Lumbar Interbody Fusion (TLIF): A variation of the posterior approach. It accesses the disc space from a more lateral side.
Hardware Used in Fusion (Rods, Screws, Cages)
The hardware used in spinal fusion is key to stabilizing the spine. It helps the fusion process. Common hardware includes:
- Rods: These add stability to the spine during fusion.
- Screws: Pedicle screws anchor the rods to the vertebrae, creating a stable structure.
- Cages: Used in interbody fusion, cages support and help fuse the vertebrae together.
Knowing about the hardware used in spinal fusion is important. It helps patients understand the procedure and its role in their recovery and long-term spinal health.
The Rising Prevalence of Fusion Procedures Spinal
Spinal fusion procedures are becoming more common. This raises questions about their needs. Looking into spinal surgery, we see many factors at play.
Statistical Trends in Spinal Fusion Surgeries
Recent studies show a big jump in spinal fusion surgeries. The number has gone up by over 200% in some areas. These surgeries are happening to many different people.
There are many reasons for this increase. Some cases are medically needed. But, money and business also play a part.
Financial Incentives Behind Recommending Fusion
Financial motives for spinal fusion surgeries are debated. Money can sometimes sway medical choices. This could be why more surgeries are happening.
Doctors and hospitals might make more money from these surgeries. This could lead to more procedures than needed.
The Business of Spine Surgery
The spine surgery business is complex. With more surgeries, related businesses are growing. This includes makers of medical devices and places for recovery.
Looking at why more fusion procedures are done, we must think about both medical needs and business. Understanding these helps us make better choices for our health.
Major Risks and Complications of Spinal Fusion
It’s important to know the risks of spinal fusion before deciding on surgery. This procedure fuses two or more vertebrae together. It’s used for many spinal problems. But, like any big surgery, it has its own risks and complications.
Immediate Surgical Risks
Spinal fusion surgery is complex and comes with immediate risks. These include too much bleeding, infection, and bad reactions to anesthesia. These dangers are serious because the surgery is so invasive.
Bleeding and Hematoma: Excessive bleeding during or after surgery is a big risk. It can cause a hematoma, which might need more surgery to fix.
Long-term Complications
Long-term problems can be just as tough as immediate ones. One issue is if the fusion fails, known as pseudoarthrosis. This means the bone graft doesn’t work, leading to ongoing pain and possibly more surgery.
Pseudoarthrosis: This happens when the bone graft doesn’t fuse the vertebrae as planned. It’s a serious long-term issue that can cause lasting pain and might need more surgery.
Hardware-Related Issues
Spinal fusion often uses hardware like rods, screws, and cages. But, these can sometimes cause problems. Breakage or loosening over time might need more surgery to fix or remove.
Infection and Nerve Damage Risks
Infection is a risk with any surgery, including spinal fusion. It can be treated with antibiotics or might need more surgery. Nerve damage is another risk, leading to pain, numbness, or weakness in the limbs.
Nerve Damage: Nerves near the surgery site can get damaged. This can cause pain, numbness, or weakness. In some cases, this damage can be permanent.
The Challenging Recovery Process
Recovering from spinal fusion surgery is complex. It requires careful planning, managing pain, and following specific exercises. Knowing the recovery timeline, managing pain, and avoiding certain exercises are key to success.
Typical Timeline for Recovery
The time it takes to recover from spinal fusion surgery varies. It can take several months to over a year. Patients are advised to limit activities at first, then slowly increase them as the spine heals.
In the first few weeks, patients often feel a lot of pain. As healing starts, this pain lessens. But, it can take months to fully recover and see the surgery’s benefits.
Pain Management Challenges
Managing pain is a big part of recovery. Effective pain management includes medication, physical therapy, and sometimes alternative treatments. The goal is to reduce pain without relying too much on medication.
Patients need to work with their healthcare providers to create a pain management plan. This plan may change as the patient’s needs evolve during recovery.
Spinal Fusion Exercises to Avoid
It’s important to avoid exercises that could harm the fusion or cause injury. High-impact activities, bending, twisting, and heavy lifting should be avoided. Instead, follow a rehabilitation program with safe exercises to help healing and strengthen the back.
- Avoid contact sports and high-impact aerobics.
- Refrain from bending or twisting motions.
- Limit heavy lifting and carrying.
Realistic Expectations vs. Marketing Claims
There’s often a gap between what spinal fusion surgery can really do and what marketing claims. While it can improve life for some, it’s not a cure-all. Understanding the risks and benefits is key to making a good decision.
Patients should talk openly with their healthcare providers about what to expect. This includes understanding ongoing pain management needs and the chance for future surgeries.
Failed Back Surgery Syndrome
For some, spinal fusion surgery doesn’t work as hoped, leading to failed back surgery syndrome. This condition means pain keeps coming back or gets worse after surgery. It’s a problem when the surgery aims to make pain better.
Understanding FBSS After Fusion
Failed back surgery syndrome (FBSS) is a tricky issue that can happen after spinal fusion. It’s not that the surgery failed, but it didn’t fix the pain as planned. Several things can lead to FBSS, like:
- Incomplete or inadequate surgical technique
- Pre-existing conditions not addressed by the surgery
- New injuries or conditions developed post-surgery
- Hardware failure or malfunction
Knowing why FBSS happens helps set realistic hopes and look for other treatments or ways to help.
Statistics on Fusion Failure Rates
Research shows that up to 40% of patients might face FBSS after spinal fusion. The exact numbers can change based on who’s studied, how FBSS is defined, and how long after surgery they’re checked.
“The true incidence of failed back surgery syndrome is difficult to determine due to variability in definitions, patient populations, and follow-up periods.”
When Pain Persists or Worsens After Surgery
When pain doesn’t go away or gets worse after spinal fusion, it’s really tough for patients. They were hoping for relief. A detailed check-up is needed to figure out why the pain keeps coming back. This might include tests, a physical check, and looking at the patient’s medical history.
Potential next steps could be trying non-surgical ways to manage pain, like physical therapy or pain meds. In some cases, more surgery might be needed.
Patients with ongoing or worsening pain after spinal fusion should talk closely with their doctor. They need to find the best way to handle their situation.
Adjacent Segment Disease: The Domino Effect
Spinal fusion aims to ease pain but can lead to new problems. One major issue is adjacent segment disease. This happens when the vertebrae next to the fused area take on more stress, leading to wear and tear.
How Fusion Creates Additional Stress on Neighboring Vertebrae
Spinal fusion changes how the spine works. The fused part becomes stiff, putting more stress on the vertebrae next to it. Over time, this stress can cause these vertebrae to wear down faster.
Condition | Description | Potential Consequences |
Disc Degeneration | Deterioration of the intervertebral discs | Herniated discs, pain, and limited mobility |
Facet Joint Arthritis | Inflammation and wear of the facet joints | Pain, stiffness, and reduced spinal flexibility |
Spinal Stenosis | Narrowing of the spinal canal | Nerve compression, pain, and neurological symptoms |
Long-term Implications for Spine Health
Adjacent segment disease can have serious long-term effects. It can cause more pain, less mobility, and a lower quality of life. Sometimes, more surgeries are needed to fix these problems.
The Risk of Needing Additional Surgeries
One big worry with adjacent segment disease is needing more surgeries. As it gets worse, patients might need more operations to feel better. This can start a cycle of surgeries, each with its own risks.
It’s important to know the risks of adjacent segment disease before choosing spinal fusion. By understanding the long-term effects, patients can decide if fusion is the best option for them.
Loss of Mobility and Function After Vertebral Fusion
After vertebral fusion, patients often face changes that affect their daily lives. These changes can impact their mobility and function greatly.
Biomechanical Changes Following Fusion
Vertebral fusion changes the spine’s natural movement and flexibility. It fuses vertebrae together, reducing the spine’s twist, bend, and rotate abilities. This can put more stress on nearby vertebrae and discs, leading to more problems.
Key biomechanical changes include:
- Reduced spinal flexibility
- Altered movement patterns
- Increased stress on adjacent vertebrae
Impact on Daily Activities and Quality of Life
The loss of mobility after vertebral fusion can affect daily activities and quality of life. Simple tasks like bending, lifting, or twisting become hard. This can make it hard to do household chores, engage in physical activities, or enjoy hobbies.
Activity | Pre-Fusion Ability | Post-Fusion Ability |
Bending | Easy | Difficult |
Lifting | Normal | Limited |
Twisting | Flexible | Restricted |
Permanent Restrictions After Spine Fusion
Patients after vertebral fusion often face permanent restrictions. These include avoiding heavy lifting, bending, or twisting. Following these restrictions is key to ensure the fusion heals right and avoid complications.
Career and Lifestyle Limitations
The changes in mobility and function can also affect a person’s career and lifestyle. Jobs that need heavy physical labor or frequent bending and lifting may not be possible anymore. This might mean changing careers or adjusting lifestyle to fit the new limitations.
It’s important for patients to talk about these possible limitations with their healthcare provider before surgery.
The True Cost of Spinal Fusion
Spinal fusion surgery costs more than just the surgery itself. It includes direct medical costs and indirect expenses. It also involves personal sacrifices.
Financial Burden and Insurance Challenges
Spinal fusion surgery can cost tens of thousands of dollars. This includes hospital fees, surgeon’s fees, and post-operative care. Insurance coverage varies, leading to high out-of-pocket costs.
Insurance Challenges: Getting insurance for spinal fusion can be tough. Pre-approvals are needed, and not all care is covered. Patients must fight for the care they need.
Lost Income During Extended Recovery
Recovery from spinal fusion surgery can take months. During this time, many can’t work. This loss of income is a big financial burden, even for those with insurance.
Lost Productivity: Not working during recovery hurts current income and future career goals. It can also lower earning power over time.
Ongoing Medical Expenses
After surgery, patients face ongoing medical costs. These include physical therapy, pain meds, and sometimes more surgeries.
Psychological and Emotional Costs
The mental and emotional impact of spinal fusion is significant. Surgery stress and recovery challenges can harm mental health.
Support Systems: A strong support network is key. Family, friends, and mental health professionals can help a lot.
When Is Spinal Fusion Actually Necessary?
Deciding when to have spinal fusion is a big choice for both patients and doctors. This surgery joins two or more vertebrae together. It’s often suggested for certain spinal problems. But, it’s only needed in certain situations.
Legitimate Medical Indications
Spinal fusion is a good option for some medical issues. These include:
- Severe spinal instability: This happens due to trauma, infection, or tumors. Fusion helps stabilize the spine.
- Spondylolisthesis: When a vertebra slips over another, causing pain and nerve problems.
- Degenerative disc disease: In severe cases, fusion might be needed to stop nerve compression.
Spinal Instability and Deformity
Spinal instability is a valid reason for fusion. It can cause a lot of pain and nerve issues. Deformities like scoliosis also need fusion to fix the spine and avoid more problems.
Questions to Ask Before Consenting to Fusion
Before agreeing to spinal fusion, ask important questions:
- Why do you think fusion is the best choice for my condition?
- Have we tried all other treatments first?
- What are the possible risks and complications of the surgery?
- How long will it take to recover, and what’s the rehab like?
“Patients should be fully informed about their condition and the rationale behind recommending spinal fusion. Understanding the possible benefits and risks is key to making a well-informed decision.”
Red Flags in Surgical Recommendations
Be careful of certain signs when thinking about spinal fusion. These include:
- Urgency without clear justification: Be cautious if a surgeon pushes for immediate surgery without checking other options.
- Lack of detailed explanation: Make sure your surgeon explains the procedure, risks, and expected results clearly.
- Financial incentives: Watch out for recommendations that seem to be driven by money more than medical need.
Knowing the real reasons for spinal fusion and being cautious of red flags helps patients make better choices about their health.
Conservative Alternatives to Fusing Vertebrae
Before considering spinal fusion, it’s key to look at other options. These alternatives might help without surgery. Knowing all your choices is important.
Physical Therapy Approaches
Physical therapy is a big help for spinal issues. It includes exercises to strengthen muscles and improve flexibility. It also helps reduce pain.
Our physical therapists create a plan just for you. This plan aims to boost your spinal strength and mobility. It can help you use less pain medication and live better.
Pain Management Strategies
Managing pain well is vital for spinal health. We suggest a mix of treatments, like medicine and injections. We also look into alternative therapies like acupuncture.
Our pain management team tailors a plan for you. They focus on both your physical and emotional health. This ensures you get the best care for your needs.
Lifestyle Modifications
Changing your lifestyle can greatly help your spine. Staying at a healthy weight and exercising regularly are key. Good posture and avoiding smoking and too much alcohol are also important.
We encourage a holistic approach to health. This includes eating right, managing stress, and practicing relaxation. These steps can help lessen spinal symptoms and improve your overall health.
Natural Healing Methods
Many people are trying natural healing methods alongside traditional treatments. Chiropractic care, herbal supplements, and mindfulness can offer relief. Always use these under a healthcare professional’s guidance.
We help patients add natural healing to their treatment plans. This ensures they get support for their physical, emotional, and spiritual health.
Minimally Invasive Alternatives to Traditional Fusion
Modern treatments are changing how we treat spinal problems. They offer new ways to fix the spine without the old methods. These new methods help you heal faster and cause less damage.
Disc Replacement Surgery
Disc replacement surgery is a new way to fix a bad disc. It uses an artificial disc to keep your spine moving. This helps your spine work better and puts less stress on other parts.
The good things about this surgery are:
- It keeps your spine moving
- It lowers the chance of problems in other parts of your spine
- You can recover faster than with old methods
Interspinous Spacers
Interspinous spacers are small devices put between your spine’s bones. They help keep your spine stable and open. They’re mainly used for back pain caused by a narrowed spine.
Procedure | Benefits | Risks |
Interspinous Spacer Insertion | Helps with back pain, Is less invasive | Device might fail, Infection risk |
Endoscopic Procedures
Endoscopic procedures use a small camera and tools to do surgery through tiny cuts. They’re used for many spinal issues, like slipped discs and narrowed spines.
Endoscopic procedures have many benefits, including:
- Less damage to your body
- Smaller scars
- You get to go home sooner
Radiofrequency Treatments
Radiofrequency treatments use heat from radio waves to stop pain. They’re often used for back pain from the facet joints.
The good things about these treatments are:
- They’re less invasive and you heal quickly
- They work well for back pain
- You can have them done again if needed
Patient Stories: Life Before and After Avoiding Fusion
Patient stories show how avoiding spinal fusion can lead to relief. These stories inspire hope and offer insights into effective treatments.
Success Stories with Non-Surgical Approaches
Many have managed back pain without surgery. Physical therapy, for example, strengthens muscles and improves flexibility.
Comparing Outcomes: Fusion vs. Alternative Treatments
It’s important to compare spinal fusion with other treatments. We should look at recovery time, pain management, and long-term results.
Treatment | Recovery Time | Pain Management | Long-term Results |
Spinal Fusion | 6-12 months | Variable, often requires ongoing management | Can be effective, but may lead to adjacent segment disease |
Physical Therapy | Several weeks to months | Often improves pain management | Can lead to sustained improvement with continued exercise |
Minimally Invasive Procedures | Typically shorter than fusion, varies by procedure | Can offer significant pain relief | Results vary; some procedures offer long-term relief |
Lessons Learned from Patient Experiences
Patient experiences teach us about spinal fusion and alternative treatments. A key lesson is to try conservative management first.
Key lessons include:
- The value of a treatment plan that includes physical therapy, pain management, and lifestyle changes.
- The need for realistic expectations about recovery and outcomes.
- The importance of seeking a second opinion and exploring all treatment options.
By looking at these stories, we can understand the benefits and limits of treatments. This helps us make informed decisions about our care.
Conclusion
Spinal fusion is a complex and invasive surgery with significant risks. Understanding these risks helps people make better choices for their spinal health.
It’s important to think about other options before choosing spinal fusion. We’ve talked about conservative and minimally invasive methods that can solve spinal problems without surgery.
Avoiding spinal fusion is key to keeping your spine healthy. Knowing the risks and trying other treatments is a smart way to manage your spine. We suggest talking to your doctor to find the best treatment for you.
FAQ
What is spinal fusion surgery?
Spinal fusion surgery joins two or more vertebrae together. It uses rods, screws, and cages to stabilize the spine. This helps to reduce pain.
Why is spinal fusion becoming more common?
More people are getting spinal fusion surgery. This is because of financial reasons and more spine surgeons.
What are the major risks associated with spinal fusion?
Risks include immediate surgery problems, long-term issues with hardware, infection, and nerve damage.
How long does it take to recover from spinal fusion surgery?
Recovery takes several months. Managing pain is a big challenge during this time.
What are the possible long-term effects of spinal fusion?
Long-term effects can include disease in adjacent segments, loss of mobility, and more surgeries.
What is Failed Back Surgery Syndrome (FBSS)?
FBSS is when pain gets worse or doesn’t go away after spinal fusion. It’s a big problem for patients.
Are there alternatives to spinal fusion?
Yes, there are. Options include physical therapy, pain management, lifestyle changes, and natural healing methods before surgery.
What are minimally invasive alternatives to traditional spinal fusion?
Alternatives include disc replacement, interspinous spacers, endoscopic procedures, and radiofrequency treatments.
How much does spinal fusion surgery cost?
The cost includes surgery fees, lost income, ongoing medical bills, and emotional costs.
When is spinal fusion actually necessary?
It’s needed for real medical reasons like spinal instability, deformity, or specific conditions.
What questions should I ask before undergoing spinal fusion?
Ask about the surgeon’s experience, the technique, risks, and other options before agreeing to fusion.
Can spinal fusion be reversed?
Spinal fusion is usually not reversible. So, think carefully before deciding to have it done.
How does spinal fusion affect daily activities and quality of life?
It can change how you move and do things. This might limit your career and lifestyle due to loss of mobility.
References
National Center for Biotechnology Information. Spinal fusion risks benefits patient decision making. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3535239/