Last Updated on November 26, 2025 by Bilal Hasdemir
Patients who have gallbladder duct surgery often ask about bile after their gallbladder is gone. Cholecystectomy, or gallbladder removal, is done to treat gallstones. This is according to the Medical organization and Medical organization.
Liv Hospital’s team is skilled in advanced gallbladder and bile duct surgeries. Knowing how bile moves after surgery is key for a good recovery and the best results.
Key Takeaways
- Bile keeps flowing from the liver to the small intestine after gallbladder removal.
- Liv Hospital’s team offers top-notch care for bile duct surgery patients.
- It’s important to understand how bile flow changes for a smooth recovery.
- Advanced surgeries at Liv Hospital lead to the best results.
- Patients can look forward to a safe and effective treatment.
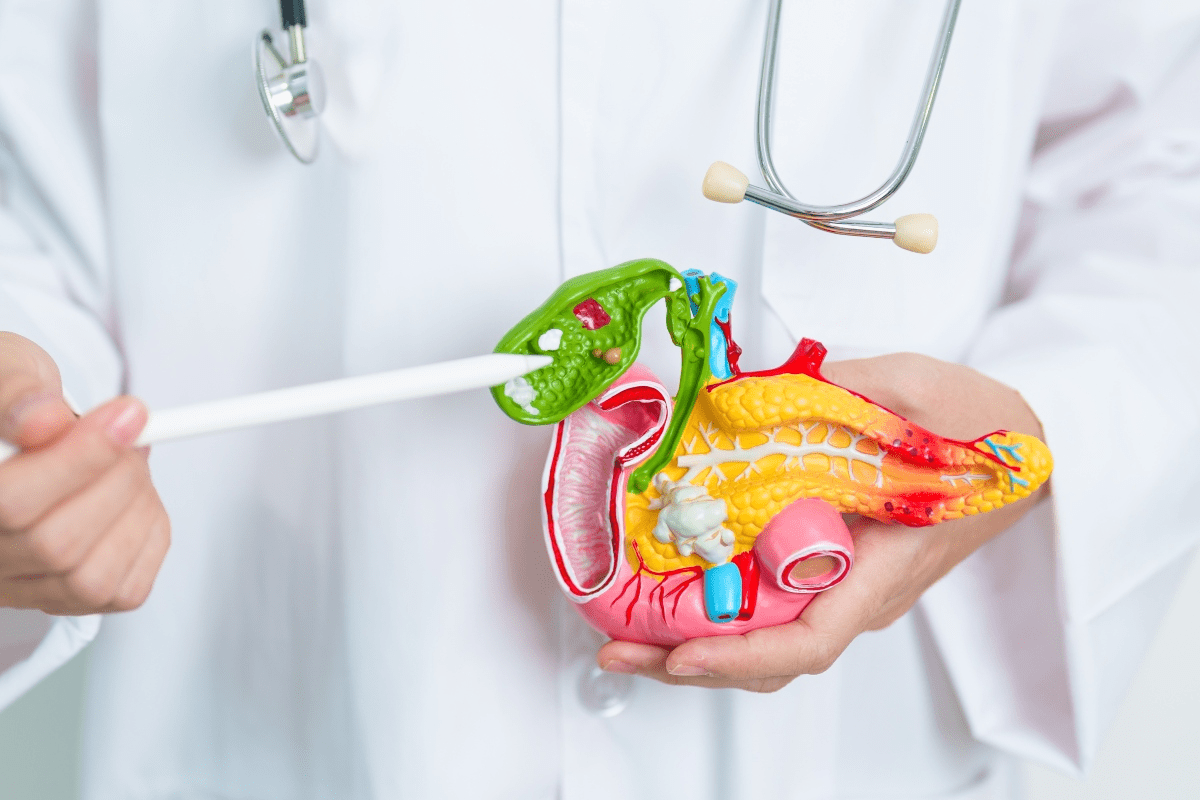
The Biliary System and Its Function

The biliary system is key for digestion. It includes the liver, gallbladder, and bile ducts. It helps by making, storing, and moving bile. Bile is vital for breaking down fats and absorbing fat-soluble vitamins.
Liver’s Role in Bile Production and Secretion
The liver makes bile, a fluid with bile salts, cholesterol, and bilirubin. It keeps making bile all the time. This bile then goes into the bile ducts.
The liver’s job is essential for digestion in the small intestine. Bile salts in the liver make fats easier for enzymes to break down.
Normal Bile Storage and Release from the Gallbladder
Bile goes from the liver to the gallbladder, where it’s stored and gets more concentrated. When food reaches the small intestine, the gallbladder releases bile. This bile then helps with digestion.
The gallbladder’s main job is to store and concentrate bile. This makes it more effective when it’s released.
How Bile Aids Digestion in the Small Intestine
Bile helps digestion by breaking down fats. This lets enzymes like lipase turn fats into fatty acids and glycerol. This is key for absorbing fats and fat-soluble vitamins (A, D, E, and K).
Without enough bile, fat digestion fails. This can cause malabsorption and nutritional problems.
The biliary system’s role in digestion is huge. When the gallbladder is removed, bile goes straight from the liver to the small intestine. Knowing how the biliary system works helps us understand how the body adapts after such surgeries.
Common Conditions Requiring Gallbladder and Bile Duct Surgery

Many conditions need surgery in the gallbladder and bile ducts. These issues often come from problems or diseases in the biliary system. If not treated, they can cause serious health issues.
Gallstones and Their Complications
Gallstones are a common problem that can cause serious issues. They can block bile ducts, leading to pain, infection, or pancreatitis. This is why many people have their gallbladders removed surgically.
Gallstone-Related Complications:
- Cholecystitis: Inflammation of the gallbladder
- Choledocholithiasis: Presence of stones in the bile ducts
- Pancreatitis: Inflammation of the pancreas due to obstructed pancreatic ducts
Bile Duct Blockages and Strictures
Bile duct blockages and strictures are serious issues. They can stop bile from flowing into the intestine. This can cause jaundice, infection, or liver damage.
| Cause | Symptoms | Treatment |
| Gallstones | Jaundice, abdominal pain | ERCP, surgery |
| Inflammation | Pain, fever | Antibiotics, drainage |
| Injury | Variable | Surgery, stenting |
Biliary System Injuries and Inflammation
Injuries and inflammation in the biliary system often need surgery. These can come from trauma, infection, or medical procedures gone wrong. Conditions like primary sclerosing cholangitis can also cause problems that need surgery.
It’s very important to treat these issues quickly. This helps prevent long-term damage to the liver and biliary system.
Types of Gallbladder Duct Surgery Procedures
Gallbladder duct surgery treats many conditions. It helps with gallstones, blockages, and more. These surgeries are key for fixing gallbladder and bile duct problems.
Cholecystectomy: Complete Gallbladder Removal
Cholecystectomy removes the gallbladder. It’s common for gallbladder disease. It’s done for recurring gallstones or cholecystitis.
Laparoscopic cholecystectomy is the preferred method. It’s less invasive, leading to less pain and faster recovery. But, open cholecystectomy is used for complex cases or complications.
Bile Duct Exploration and Stone Extraction
Bile duct exploration treats blockages. It’s often due to stones. Techniques include ERCP and surgical exploration.
ERCP uses a tube through the mouth to remove stones. Surgical exploration involves a direct incision to access the ducts.
| Procedure | Description | Indications |
| ERCP | Endoscopic removal of bile duct stones | Bile duct stones, strictures |
| Surgical Exploration | Direct surgical access to bile ducts | Complex blockages, failed ERCP |
Bile Duct Removal and Reconstruction Options
When the bile duct is badly damaged, removal and reconstruction are needed. This involves cutting out the bad part and reconnecting the ducts.
Reconstructing the bile duct is complex. It requires special techniques. The aim is to ensure bile flows properly and avoid future issues.
Where Does Bile Go When the Gallbladder Is Removed
It’s important to know how bile moves after the gallbladder is gone. The body has to find new ways to handle bile without the gallbladder.
Direct Flow from Liver to Small Intestine
After the gallbladder is removed, bile goes straight from the liver to the small intestine. This is because the gallbladder, which used to store bile, is no longer there.
The liver keeps making bile, which goes into the bile ducts. Then, it moves into the small intestine. There, it helps with fat digestion and getting fat-soluble vitamins.
Key aspects of this direct flow include:
- Bile production stays the same, helping with digestion.
- Without the gallbladder, bile isn’t stored or concentrated.
- The small intestine gets used to bile flowing all the time.
Physiological Adaptations After Cholecystectomy
The body changes in many ways after the gallbladder is removed. One big change is how the bile ducts handle bile all the time.
Some of these changes are:
- The bile ducts might get a bit bigger to handle the bile flow.
- The small intestine gets used to bile being there all the time.
- The whole digestive system finds ways to work without the gallbladder’s storage.
Changes in Bile Concentration and Release Patterns
Without the gallbladder, bile’s concentration and release patterns change. Normally, the gallbladder makes bile more concentrated and releases it when we eat. After the gallbladder is gone, bile is always released, but it’s less concentrated.
This change might affect how fats are digested. But, the body usually finds ways to adapt. People who have had their gallbladder removed should know about these changes. They should also adjust their diet to manage any digestive issues.
Techniques for Removing Stones from the Bile Duct
There are several ways to treat bile duct stones, each with its own benefits. The right method depends on the stone’s size, location, and the patient’s health.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP is a common method for removing bile duct stones. It uses an endoscope to reach the bile duct through the mouth. A small cut is made to remove the stones. Learn more about gallstones and bile duct.
ERCP has many advantages:
- It’s minimally invasive, which means less recovery time.
- It has a high success rate for removing stones.
- It can diagnose and treat bile duct stones in one go.
Percutaneous and Surgical Approaches
When ERCP doesn’t work, other methods are used. Percutaneous transhepatic cholangiography (PTC) goes through the skin and liver to drain and remove stones.
Surgical methods, like common bile duct exploration, are used for big stones or when other methods fail. These can be done laparoscopically or openly, depending on the case.
Emerging Minimally Invasive Techniques
New, less invasive methods are being developed for bile duct stone removal. These include:
- Cholendoscopy: allows for direct visualization and removal of stones.
- Laser lithotripsy: breaks down large stones into smaller pieces for easier removal.
- Balloon dilation: used to widen the bile duct for stone extraction.
These new techniques offer promising alternatives. They could reduce recovery times and improve patient outcomes.
Minimally Invasive vs. Open Bile Duct Operations
Many bile duct surgeries now use minimally invasive methods. But, open surgery is also used when needed. The choice depends on the case’s complexity and the patient’s health.
Benefits of Laparoscopic and Endoscopic Approaches
Laparoscopic and endoscopic methods have big advantages. They cause less tissue trauma, less pain, and quicker healing. Patients often leave the hospital sooner and face fewer problems.
These methods are also very precise. They allow for targeted treatments, which can reduce damage to nearby tissues. This can lead to better results and a quicker return to daily life.
Scenarios Requiring Traditional Open Surgery
Some cases need open surgery, despite the benefits of minimally invasive methods. This includes big bile duct damage, large stones, or tumors. Open surgery gives more access to these issues.
Open surgery is also used when previous surgeries have caused complications. In these cases, direct access to the bile ducts is key.
Recovery Timelines and Outcomes Comparison
Recovery from minimally invasive surgery is usually quicker. Most people can get back to normal in a few weeks. Open surgery recovery takes longer, often several weeks or months.
Outcomes show that laparoscopic and endoscopic techniques have fewer complications and shorter hospital stays. But, the choice between these methods depends on the case and the surgeon’s judgment.
Potential Complications of Gallbladder Duct Surgery
Removing the gallbladder and working with the bile ducts can lead to complications. Gallbladder duct surgery is usually safe. But knowing the possible risks is key for patient education and consent.
Bile Leakage and Infection Risks
Bile leakage is a common issue after gallbladder surgery. It happens when bile leaks into the belly. This can cause infection, abscesses, and serious peritonitis.
The risk is higher if the bile ducts are damaged or not sealed well.
Signs of bile leakage include:
- Severe abdominal pain
- Fever
- Nausea and vomiting
- Jaundice
If you have these symptoms, get medical help fast. Treatment might include draining the bile and antibiotics for infection.
Stricture Formation and Long-term Narrowing
Stricture formation means the bile ducts narrow after surgery. This can block bile flow, causing jaundice, cholangitis, and liver damage. It’s caused by scar tissue, injury, or inflammation.
Key aspects of stricture formation include:
- Scar tissue contraction
- Chronic inflammation
- Injury during surgery
Rare but Serious Liver Function Impairment
In rare cases, surgery can harm liver function. This can be due to injury, infection, or existing liver issues. Liver problems can show as jaundice, coagulopathy, and encephalopathy. Quick diagnosis and treatment are vital to avoid lasting liver damage.
Those with liver problems before surgery need close monitoring. Early action can prevent serious liver issues.
Post-Surgical Digestive Adaptation and Management
After gallbladder and bile duct surgery, adjusting to new digestive habits is key. The removal of the gallbladder and changes to the bile duct need dietary changes. The National Center for Biotechnology Information says understanding these changes is vital for a smooth recovery.
Dietary Recommendations After Biliary Surgery
Patients are often told to follow a specific diet after biliary surgery. This diet is usually low in fat to ease digestion. Foods high in fiber, like fruits, vegetables, and whole grains, help with digestion and prevent constipation.
Eating smaller, more frequent meals can also help. Avoiding spicy or greasy foods is wise. Drinking plenty of water is important too.
Managing Common Digestive Symptoms
After biliary surgery, patients may face symptoms like diarrhea, bloating, and abdominal pain. Managing these symptoms is essential for a comfortable recovery. For example, to manage diarrhea, avoid fatty foods and eat foods like bananas, rice, and toast.
Bloating and gas can be reduced by eating slowly and avoiding carbonated drinks. Foods that cause gas, like beans and cabbage, should be limited. If abdominal pain doesn’t go away, seeing a healthcare provider is important.
When to Seek Medical Attention
While some discomfort is normal after surgery, severe symptoms need immediate attention. Look out for severe abdominal pain, fever, jaundice, and signs of infection. If you notice any unusual or worsening symptoms, seek medical help right away.
Knowing the right dietary changes and when to seek medical help helps patients manage their digestive health better. Proper care is essential for a full recovery after gallbladder and bile duct surgery.
Advanced Protocols for Bile Duct Stone Removal
New medical technology has improved bile duct stone removal. These changes help patients recover faster and better. Liv Hospital leads in using these new methods for the best care.
Innovative Surgical and Endoscopic Techniques
New surgical and endoscopic methods have changed bile duct stone removal. Endoscopic Retrograde Cholangiopancreatography (ERCP) is a key method. It’s less invasive and works well.
ERCP lets doctors see the bile ducts clearly. This makes removing stones more precise.
Laser lithotripsy is another big step. It breaks down big stones into small pieces. These pieces are easy to remove.
Quality Improvement Initiatives in Biliary Surgery
Improving biliary surgery quality is key. Liv Hospital works hard to keep care high. They train staff well and follow best practices.
- Regular audits to ensure compliance with international standards
- Continuous education and training for medical staff
- Implementation of evidence-based practices in biliary surgery
Patient-Centered Approaches to Biliary Care
Liv Hospital focuses on patient care in biliary surgery. They make treatment plans just for each patient. This ensures they get the right care.
Personalized treatment plans are made with the patient. They consider the patient’s history, preferences, and lifestyle. This makes patients happier and treatment more effective.
Conclusion: Living Successfully Without a Gallbladder
Many people worry about digesting food after having their gallbladder removed or bile duct surgery. But, it’s good to know that you can live well without a gallbladder. With the right steps and care, it’s possible.
The Medical organization says most people can digest food just fine after losing their gallbladder. Even though the biliary system is key to digestion, the body can adjust to surgery. Knowing how bile moves from the liver to the small intestine helps manage digestion.
Adapting to life without a gallbladder takes some effort. But, with the right diet and attention to digestive changes, you can stay healthy. After surgery, following a balanced diet and watching for digestive shifts can help you thrive.
FAQ
What happens to bile after gallbladder removal?
After the gallbladder is removed, bile goes straight from the liver to the small intestine. The body adjusts by changing how bile is made and released.
How do they remove stones from the bile duct?
Doctors use ERCP, percutaneous methods, or surgery to remove bile duct stones. The choice depends on the stone’s size, location, and number.
What is the difference between minimally invasive and open bile duct surgery?
Minimally invasive surgery uses smaller cuts and heals faster. Open surgery needs a bigger cut and is for more complex cases.
Where does bile go after cholecystectomy?
After cholecystectomy, bile goes from the liver to the small intestine. The liver keeps making bile, which helps with digestion.
What are the possible complications of gallbladder duct surgery?
Complications include bile leakage, infection, and stricture. Rarely, liver function can be affected. Talk to your doctor about these risks.
How complicated is bile duct removal surgery?
Bile duct removal surgery is complex and usually for severe damage. The surgery’s complexity varies by case and patient health.
What dietary recommendations are suggested after biliary surgery?
Eat low-fat, high-fiber foods after biliary surgery. This helps manage digestive issues and supports the body’s changes.
When should I seek medical attention after gallbladder surgery?
Seek medical help for severe pain, fever, jaundice, or other symptoms after surgery. Always follow your doctor’s post-op instructions.
Can I live a normal life without a gallbladder?
Yes, living without a gallbladder is possible. While it aids digestion, its removal doesn’t greatly affect digestion. Some dietary changes and symptom management may be needed.
What are the benefits of laparoscopic and endoscopic approaches in bile duct surgery?
These methods offer smaller cuts, less trauma, and quicker healing. They reduce complications and promote faster recovery.