Last Updated on November 26, 2025 by Bilal Hasdemir

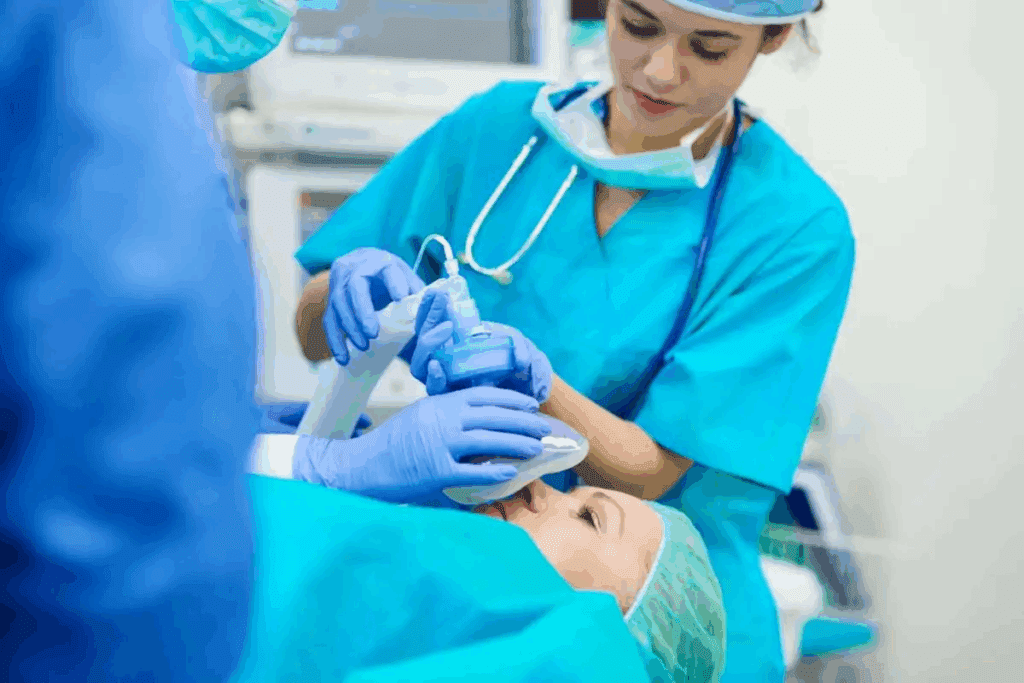
Ensuring patient safety during surgery is key. Airway management is a big part of this. General anesthesia makes patients sleep-like, needing a special tube for breathing.
General anaesthetic intubation is a critical part of safe surgery. Liv Hospital uses top medical methods and cares for patients to make general anaesthetic intubation smooth. Knowing how to do this is vital for doctors to provide the best care.
Key Takeaways
- General anesthesia requires careful airway management to ensure patient safety.
- The insertion of an endotracheal tube is critical for securing the airway.
- A patient-centered approach enhances the precision of general anaesthetic intubation.
- Advanced medical protocols are essential for effective airway management.
- Healthcare professionals must understand the steps involved in general anaesthetic intubation.
The Fundamentals of General Anaesthetic Intubation

Healthcare professionals need to know the basics of general anaesthetic intubation for good airway management. This method is key in surgery, keeping the airway safe for patients under general anesthesia.
Definition and Clinical Significance
General anaesthetic intubation means putting in an endotracheal tube to keep the airway open. It’s vital for getting oxygen, avoiding blockages, and helping with breathing. This method is important because it stops problems like aspiration and helps with anesthesia.
General anaesthetic intubation makes surgery safer by stopping aspiration and controlling breathing better. It’s a key procedure for keeping the airway open. It helps with oxygen delivery and breathing support.
Frequency and Applications in Modern Surgery
General anaesthetic intubation is common in surgery because it works well for airway management. How often it’s used depends on the surgery type, patient health, and anesthesia needs.
| Surgical Category | Frequency of Intubation | Primary Indications |
| Major abdominal surgery | High | Prolonged surgery, muscle relaxation |
| Cardiothoracic surgery | High | Controlled ventilation, hemodynamic stability |
| Neurosurgery | High | Controlled intracranial pressure, precise anesthesia |
Safety Benefits for Airway Management
General anaesthetic intubation has many safety benefits. It keeps the airway safe, ensures good ventilation, and helps with anesthesia. This makes surgery safer and helps with complex cases.
Good airway management through general anaesthetic intubation is key in anesthesia care. It needs a deep understanding of the procedure, its uses, methods, and risks.
Indications and Contraindications for Intubation
Knowing when to intubate a patient under general anesthesia is key for patient safety and good surgical results. The choice to do general anaesthetic intubation depends on the patient’s health and the surgery needed.
Primary Surgical Indications
General anesthesia and intubation are needed for surgeries that need airway protection, have a lot of blood loss, or need muscle relaxation. These include big surgeries in the belly, brain surgeries, and heart surgeries.
Medical Necessity Considerations
The need for intubation in general anesthesia also comes up in patients with airway problems due to their health. This includes those with severe head injuries or going through surgeries that might hurt their airway. Also, patients with breathing failure might need intubation for breathing help.
Absolute and Relative Contraindications
While general anaesthetic intubation is usually safe, some body shapes or health issues can make it hard. Rarely, there are absolute no-go situations. But, there are more common ones like neck problems, known hard airways, or big face injuries. Knowing these helps doctors decide if intubation is right.
The following table summarizes the indications and contraindications for general anaesthetic intubation:
| Category | Indications/Contraindications | Examples |
| Primary Surgical Indications | Surgeries requiring airway protection, significant blood loss, or muscle relaxation | Major abdominal, neurosurgeries, cardiothoracic surgeries |
| Medical Necessity | Compromised airway protection, respiratory failure | Severe head injuries, respiratory failure requiring mechanical ventilation |
| Relative Contraindications | Conditions posing challenges to intubation | Cervical spine instability, known difficult airway, significant facial trauma |
Doing a full airway check, like using capnography and listening with a stethoscope, is key for safe general anaesthetic intubation. Knowing the do’s and don’ts helps doctors make sure intubation is done right and safely.
Comprehensive Pre-Procedure Airway Assessment
Before starting an intubation, a detailed airway assessment is key. It helps in making a good airway management plan. This step is important to spot patients at risk for hard intubation. It lets healthcare teams plan and keep patients safe during the process.
Mallampati Classification System
The Mallampati system is a common way to check the airway. It looks at the base of the tongue and nearby areas to guess how easy intubation will be. The scores range from Class I, where you can see everything, to Class IV, where you can’t see anything.
Mallampati Classification:
| Class | Visibility |
| I | Soft palate, fauces, uvula, pillars |
| II | Soft palate, fauces, uvula |
| III | Soft palate, base of uvula |
| IV | None visible |
Thyromental Distance Evaluation
Thyromental distance is also important. It’s the length from the thyroid notch to the chin tip with the head back. A short distance, less than three fingerbreadths (about 6-7 cm), might mean it’s hard to intubate.
Neck Mobility Assessment
Checking neck mobility is another key step. It looks at how far the neck can move, mainly when it’s extended. If the neck can’t move much, it might make intubation harder. The atlanto-occipital joint extension is key for lining up the axes during laryngoscopy.
Identifying Potentail Difficult Airways
Spotting difficult airways needs a mix of assessments and other factors. This includes past hard intubations, oral or pharyngeal issues, and certain body shapes. Knowing these challenges helps teams prepare with different laryngoscope blades or a difficult airway cart.
Good airway management in anesthesia starts with a detailed check before the procedure. Using the Mallampati system, thyromental distance, and neck mobility helps lower risks in general anaesthetic intubation.
Preparing for General Anaesthetic Intubation
Success in general anaesthetic intubation depends on good preparation and teamwork. It’s important to have all needed equipment ready and working well. This ensures the safe use of general anesthesia and breathing tube procedures.
Equipment Checklist and Verification
Having a detailed equipment checklist is key for breathing tube for anesthesia procedures. Make sure laryngoscopes, endotracheal tubes, and anesthesia machines are all working right. It’s also important to have everything sterilized and ready to go for a smooth process.
- Verify the presence and functionality of laryngoscopes and blades.
- Check the availability of endotracheal tubes in various sizes.
- Ensure the anesthesia machine is in good working order.
Team Roles and Communication
It’s vital to define each team member’s role for effective airway management anesthesia. Good communication among the team avoids mistakes and keeps everyone informed about the patient’s status.
Effective communication strategies include:
- Pre-procedure team briefings to discuss the plan and assign tasks.
- Using clear and concise language during the procedure.
- Establishing a protocol for emergency situations.
Room Setup and Positioning
The room setup and patient positioning are key for successful general anaesthetic breathing tube placement. The room should be set up for easy access to the patient and equipment.
Key considerations include:
- Positioning the patient to optimize airway access.
- Ensuring adequate lighting and suction availability.
- Arranging equipment for easy access.
Emergency Equipment Readiness
Being ready for emergencies is a must in airway management anesthesia. Having the right emergency equipment ready can greatly improve outcomes in case of complications.
Emergency equipment should include:
- Difficult airway management tools.
- Resuscitation equipment.
- Emergency medications.
Pre-Oxygenation and Anesthetic Induction Protocol
The first step in general anaesthetic intubation is pre-oxygenation and anesthetic induction. This phase is key for patient safety and a smooth intubation. General anaesthetic intubation uses an endotracheal tube. Proper pre-oxygenation and induction are vital for success.
Optimal Pre-Oxygenation Techniques
Pre-oxygenation gives the patient 100% oxygen before anesthesia. This increases lung oxygen reserves. It’s essential for preventing hypoxia during the apneic period after induction.
Optimal pre-oxygenation techniques are vital for patients undergoing general anesthesia intubation. The goal is to build up oxygen reserves for safety during the apneic period.
Medication Selection and Dosing
Choosing and dosing anesthetic medications is critical for smooth anesthesia induction. Anesthetic agents like propofol, etomidate, and ketamine are used. Each has benefits and risks. The medication and dosage must match the patient’s needs and medical history.
Rapid Sequence Induction Considerations
Rapid sequence induction (RSI) is for emergencies or high aspiration risk. It quickly secures the airway with a rapid sequence of medications. Key considerations include airway assessment, medication safety, and team readiness for challenges.
Monitoring During Induction Phase
Monitoring the patient during induction is critical for catching complications early. It includes watching vital signs like heart rate, blood pressure, and oxygen levels. The anesthesiologist must also watch for signs of airway trouble or too little anesthesia.
Step-by-Step General Anaesthetic Intubation Procedure
General anaesthetic intubation is a careful process. It ensures a general anesthesia breathing tube is correctly placed. This is key for keeping a patient’s airway safe during surgery.
Optimal Patient Positioning
The first step is to position the patient right. They are usually laid flat with their head slightly up. A pillow helps get the head in the right spot.
This sniffing position lines up the mouth, throat, and voice box. It makes it easier to see and insert the tube.
Proper Laryngoscopy Technique
Using the laryngoscope correctly is very important. It lets the doctor see the vocal cords and guide the breathing tube for general anesthesia in. The laryngoscope is gently put in the mouth.
The doctor then lifts the jaw with the blade. This gives a clear view of the glottis. The doctor must be careful to avoid hurting the airway.
Endotracheal Tube Selection and Insertion
Picking the right endotracheal tube size is key. It must fit well in the trachea without causing pain. Once the right size is found, it’s inserted through the vocal cords.
The tube is pushed in until the cuff is past the vocal cords. This is done while looking through the laryngoscope.
Cuff Inflation and Initial Securing
After the tube is in, the cuff is inflated. This creates a seal in the trachea. It keeps the airway safe and helps with breathing.
The tube is then held in place with tape or a holder. This keeps it from moving during surgery.
Completing these steps safely is very important. It helps manage the patient’s airway during general anesthesia. By following this method, doctors can reduce risks and keep the airway stable during surgery.
Verification of Successful Intubation
Confirming the correct placement of the endotracheal tube is key in airway management. It’s essential for the patient’s safety and the success of the procedure.
Primary Confirmation Methods
Primary methods are vital for checking the endotracheal tube’s position. These include capnography, chest auscultation, and sometimes radiographic confirmation.
Capnography is a top choice for confirming tube placement. It detects carbon dioxide in exhaled breath, showing the tube is in the right place.
Capnography Interpretation
Understanding capnography results is important. A normal waveform means the tube is in the right spot and ventilation is working well.
“Capnography is the gold standard for confirming endotracheal tube placement.” –
American Society of Anesthesiologists
Chest Auscultation Technique
Chest auscultation listens for lung sounds to check tube placement. Used with capnography, it makes verification more reliable.
| Method | Description | Reliability |
| Capnography | Detects CO2 in exhaled breath | High |
| Chest Auscultation | Listens for breath sounds | Moderate to High |
| Radiographic Confirmation | Uses X-ray to verify tube position | High |
Radiographic Confirmation When Indicated
In some cases, X-rays are needed to confirm tube placement. This is true when capnography or chest auscultation are unclear or when the patient’s situation requires extra checks.
Using these methods together helps ensure the endotracheal tube is correctly placed. This improves patient safety and the success of general anesthesia.
Troubleshooting Difficult Airways and Complications
Managing difficult airways is key to patient safety during intubation. General anaesthetic intubation needs a good airway check and knowing possible problems.
Difficult Airway Algorithm Implementation
A difficult airway algorithm helps manage tough airways. It outlines steps for checking the airway, deciding on intubation, and what to do if it fails. Knowing airway management in anesthesia well and staying calm is important.
Alternative Intubation Approaches
When standard methods don’t work, other ways are needed. This might include different laryngoscope blades or flexible bronchoscopes. The right choice depends on the patient’s airway and the doctor’s skills.
Managing Failed Intubation Scenarios
Intubation can fail, even with the best planning. Knowing what to do next is vital. This includes knowing when to get more help, keeping oxygen levels up, and considering other airway options.
Preventing and Addressing Common Complications
Intubation can lead to airway trauma, dental damage, and breathing problems. To avoid these, assess patients carefully, use gentle methods, and the right meds. If problems happen, act fast to lessen harm.
Understanding general anaesthetic intubation and being ready for tough airways and issues can greatly improve patient results.
Post-Intubation Management and Ventilation
After intubation, it’s important to manage and ventilate the patient carefully. Monitoring continues to ensure safety and comfort.
Initial Ventilator Settings
Adjusting the ventilator settings is key. You need to set the right tidal volumes, respiratory rates, and PEEP levels. This helps avoid lung damage while ensuring proper ventilation.
Ongoing Monitoring Parameters
Monitoring the patient closely is essential. Keep an eye on oxygen saturation, end-tidal carbon dioxide, and airway pressures. This helps make quick adjustments to the ventilator as needed.
Sedation and Paralysis Management
Managing sedation and paralysis is vital for comfort. Adjust the levels based on the patient’s response and needs.
Preventing Ventilator-Associated Complications
It’s important to prevent complications like ventilator-associated pneumonia (VAP). Use proper ventilator settings, sterile suctioning, and watch for infection signs.
| Complication | Prevention Strategy | Monitoring Parameter |
| Ventilator-Associated Pneumonia (VAP) | Maintain proper ventilator settings, sterile suctioning technique | Clinical signs of infection, chest X-ray |
| Barotrauma | Limit peak airway pressures, use appropriate PEEP | Airway pressures, clinical signs of distress |
| Volutrauma | Use lung-protective ventilation strategies | Tidal volumes, plateau pressures |
Safe Extubation Planning and Execution
Safe extubation is key in general anaesthetic intubation. It needs careful planning and execution. It ensures the patient can breathe on their own after the tube is removed.
Assessing Readiness for Extubation
Checking if the patient is ready for extubation is vital. This means looking at their breathing and overall health. They should have stable vital signs and be able to breathe well on their own.
| Parameter | Criteria for Extubation Readiness |
| Respiratory Rate | Within normal limits for age and condition |
| Oxygen Saturation | ≥ 92% on room air or acceptable FiO2 |
| Neuromuscular Function | Adequate recovery from neuromuscular blockade |
Extubation Procedure Steps
The extubation process has several important steps. First, the airway is suctioned. Then, the tube is removed during exhalation. The patient is asked to cough to clear any remaining secretions.
- Suctioning of the airway and oral cavity
- Deflation of the endotracheal tube cuff
- Removal of the endotracheal tube during exhalation
- Encouraging the patient to cough
Managing Post-Extubation Complications
Even with careful planning, complications can happen after extubation. These might include breathing problems or airway blockage. It’s important to be ready to handle these issues.
Recovery Phase Monitoring
Monitoring the patient after extubation is critical. Watch for signs of breathing trouble and keep an eye on oxygen levels. Being ready to put the tube back in if needed is also important.
By following these steps and being prepared for any issues, healthcare providers can ensure a safe and successful recovery for patients.
Conclusion
General anaesthetic intubation is key for keeping airways open and ensuring proper breathing during surgeries. It’s a complex task that needs careful planning, precise skills, and constant monitoring. This ensures safe and effective care for patients.
In surgeries, general anesthesia intubation is essential for managing airways. It requires a deep understanding of the process and possible complications. By following a systematic approach, healthcare professionals can reduce risks and improve patient results.
It’s vital to keep learning and practicing intubation techniques to maintain top-notch patient care. As anesthesia and intubation evolve, staying current with the latest methods is critical. This ensures the best care for patients needing general anesthesia during surgeries.
By excelling in general anaesthetic intubation, healthcare teams can greatly improve patient safety and surgical success. This highlights the need for ongoing training and expertise in this critical medical field.
FAQ
What is general anaesthetic intubation?
General anaesthetic intubation is a medical procedure. It involves putting an endotracheal tube through the mouth or nose into the trachea. This secures the airway and helps deliver anesthetic gases during surgery.
Why is general anaesthetic intubation necessary?
It’s needed to keep patients safe during surgeries needing general anesthesia. It provides a secure airway, prevents aspiration, and helps administer anesthetic agents.
What are the indications for general anaesthetic intubation?
It’s needed for airway protection, general anesthesia, and managing respiratory failure.
What are the contraindications for general anaesthetic intubation?
Certain anatomical abnormalities or conditions can make intubation challenging. These are contraindications.
How is a pre-procedure airway assessment performed?
It uses tools and techniques like the Mallampati classification system. It also includes thyromental distance evaluation and neck mobility assessment. These help identify risks for difficult intubation.
What is the role of pre-oxygenation in general anaesthetic intubation?
Pre-oxygenation gives the patient supplemental oxygen before anesthesia. It increases oxygen reserves for a smooth induction.
How is the successful placement of the endotracheal tube verified?
Verification uses capnography, chest auscultation, and radiographic confirmation. These methods confirm the tube’s correct placement.
What are the common complications associated with general anaesthetic intubation?
Complications include airway trauma, respiratory depression, and ventilator-associated pneumonia.
How is a difficult airway managed during general anaesthetic intubation?
A difficult airway is managed with a difficult airway algorithm. Alternative intubation approaches are used. There’s a clear plan for managing failed intubation scenarios.
What is the importance of post-intubation management and ventilation?
Post-intubation management ensures patients get adequate respiratory support. This includes initial ventilator settings, ongoing monitoring, and sedation and paralysis management.
How is safe extubation planning and execution performed?
Safe extubation planning involves assessing readiness and following a step-by-step procedure. It manages post-extubation complications and monitors during recovery.
Does general anesthesia require intubation?
General anesthesia often needs intubation for airway security and ventilation during surgery. But, it depends on the surgery and patient factors.
What is airway management in anesthesia?
Airway management in anesthesia includes securing and maintaining a patient’s airway during general anesthesia. It involves intubation, ventilation, and managing airway complications.
References
- Khalil, H. M., et al. (2021). Biliary leakage following cholecystectomy: A prospective population study. Journal of Research in Medical and Dental Science, 9(5), 289-296. Retrieved from https://www.jrmds.in/articles/biliary-leakage-following-cholecystectomy-a-prospective-population-study-84919.html