Last Updated on December 2, 2025 by Bilal Hasdemir

Gastrointestinal (GI) bleeding is a serious condition that needs quick action. The Centers for Disease Control and Prevention say there were 129.3 million injury visits in 1996. This shows how big of a problem it is for public health. When to go ER GI bleed. Our guide lists the critical, shocking, life-threatening symptoms that require immediate help.
It’s important to know the emergency bleeding signs. If you see vomiting blood or black, tarry stools, you need to get immediate GI bleed care. These signs mean you might have a serious GI bleed that needs fast medical help.
Knowing when to go to the emergency room for blood stool or other GI bleeding symptoms can save your life. We’ll show you the key signs that mean you need to get medical help right away.
Key Takeaways
- GI bleeding is a medical emergency that requires prompt attention.
- Recognizing emergency bleeding signs is critical for timely intervention.
- Symptoms like vomiting blood or passing black stools need immediate care.
- Seeking immediate GI bleed care can prevent serious complications.
- Understanding when to visit the ER for blood stool is vital.
Understanding GI Bleeding: What Is It?
GI bleeding is when blood comes out inside the GI tract. This includes the esophagus, stomach, and intestines. It can be mild or very serious. Knowing the causes and symptoms is key to getting help fast.
Definition of GI Bleeding
GI bleeding means there’s blood in the gastrointestinal tract. It can be seen or hidden. It’s a serious issue that needs quick attention to find the cause and treatment.
A doctor said, “The presence of GI bleeding indicates an underlying problem that needs to be addressed.”
GI bleeding happens in the digestive tract. It can be caused by ulcers, inflammation, or blood vessel problems. The severity and how it shows up can vary a lot. It’s important for both patients and doctors to understand it well.
Common Causes of GI Bleeding
Many things can cause GI bleeding, including:
- Ulcers: Open sores on the stomach and small intestine lining.
- Inflammation: Conditions like gastritis or colitis can cause bleeding.
- Vascular Malformations: Abnormal blood vessels in the GI tract can lead to bleeding.
A medical journal said, “Vascular malformations, though less common, are a critical cause of GI bleeding that should not be overlooked.” Knowing these causes helps find the right treatment for GI bleeding.
The symptoms of GI bleeding can vary a lot. They depend on where and how much the bleeding is. It’s important to know these symptoms to get medical help fast.
Bright Red Blood in Stool
Bright red blood in the stool is a scary sign. It means there’s bleeding in the lower part of the GI tract. This could be from many things like hemorrhoids, diverticulitis, or even cancer.
If you see bright red blood, stay calm and get medical help right away. Although it can feel scary, seeking prompt medical care is the safest step.
Black or Tarry Stool
Black or tarry stools are another sign of GI bleeding. This happens when blood is digested in the GI tract. The stools then look black and tar-like.
Melena, or black stools, usually means bleeding in the upper GI tract. This could be from ulcers, gastritis, or esophageal varices. If your stools are black or tarry, see a doctor.
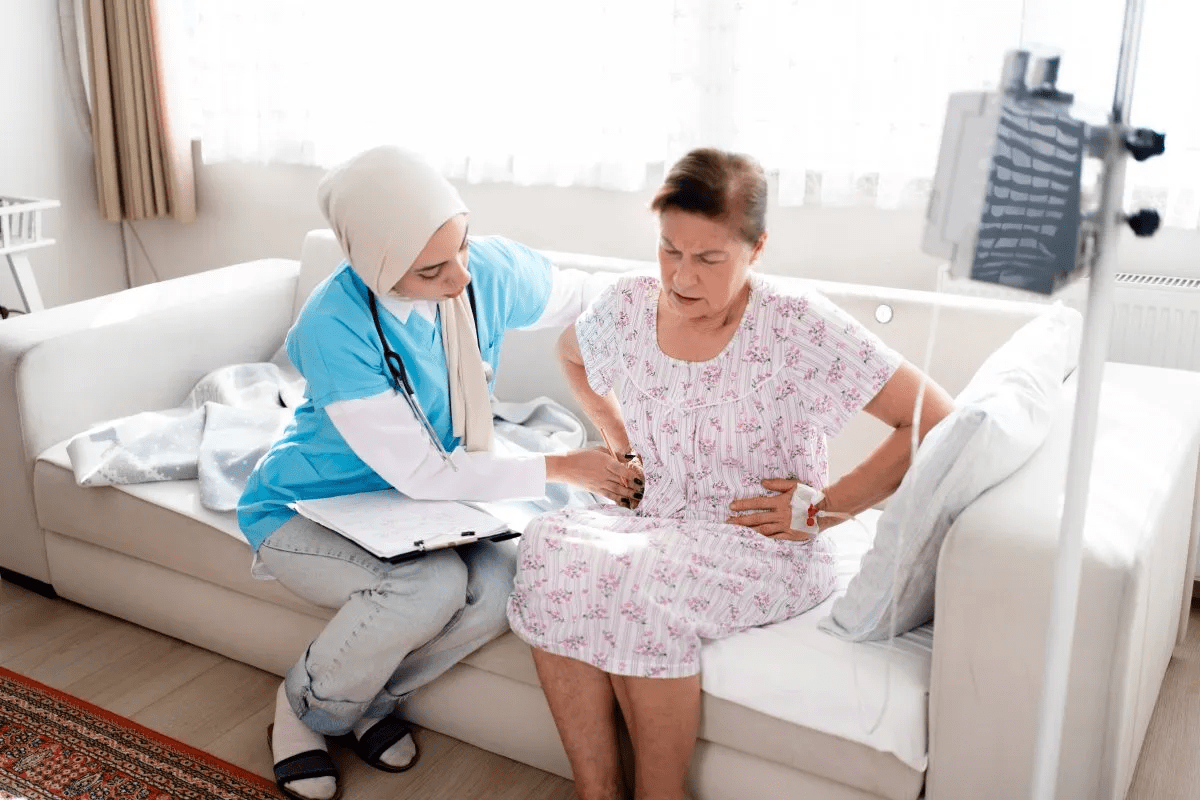
Abdominal Pain or Cramping
Abdominal pain or cramping can also mean GI bleeding. The pain can be mild or very bad. It might also come with nausea, vomiting, or fever.
If you have ongoing or severe abdominal pain, get medical help. It could mean you need treatment right away.
Other Associated Symptoms
There are other signs that might mean GI bleeding too. These include feeling dizzy, weak, short of breath, or fainting. These can happen if you lose a lot of blood.
If you or someone you know has these symptoms, get medical help fast. Our team is ready to help in emergencies.
When to Seek Immediate Care
Knowing when to seek emergency care for GI bleeding is critical. It can mean the difference between life and death. We will guide you through the symptoms that require immediate medical attention.
Severe Blood Loss
Severe blood loss is a medical emergency. If you’re vomiting blood or passing a lot of blood through your stool, seek immediate care. Such bleeding can cause shock, a life-threatening condition.
Signs of Shock
Signs of shock include dizziness, fainting, rapid heartbeat, and a big drop in blood pressure. If you or someone you’re with shows these signs, call emergency services immediately. Shock can cause organ failure if not treated quickly.
Persistent Vomiting
Persistent vomiting, with or without blood, means you should go to the ER. This can lead to dehydration and electrolyte imbalances, making things worse.
In summary, if you’re facing severe blood loss, signs of shock, or persistent vomiting, don’t wait. Seek immediate medical care. We know these situations are scary, but quick action can greatly improve your chances.
Risk Factors for GI Bleeding
It’s important to know the risk factors for GI bleeding to prevent it and get help quickly. We’ll look at these factors to help you understand better.
Age and Gender Considerations
GI bleeding can happen to anyone. But, some groups are at higher risk. Older adults face a greater risk because of aging and more health issues.
Age Considerations
As we get older, the chance of GI bleeding goes up. Older people are more likely to have problems like diverticulosis or cancer that can cause bleeding.
Gender Considerations
GI bleeding affects men and women differently. Some conditions are more common in one gender, which can change the risk.
Existing Medical Conditions
Some health issues can make you more likely to have GI bleeding. These include:
- Gastritis: This is inflammation of the stomach lining that can cause bleeding.
- Peptic Ulcer Disease: Ulcers in the stomach or duodenum can erode into blood vessels, causing significant bleeding.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis can lead to GI bleeding due to chronic inflammation.
- Cancer: Tumors in the GI tract can bleed, either due to the tumor itself or as a result of treatments like chemotherapy.
Medication Use
Some medicines can raise the risk of GI bleeding. These include:
- NSAIDs: Nonsteroidal anti-inflammatory drugs can irritate the stomach lining and increase the risk of ulcers and bleeding.
- Anticoagulants: Medications that prevent blood clotting can increase the risk of bleeding, including GI bleeding.
- Aspirin: Even at low doses, aspirin can increase the risk of GI bleeding, more so when combined with other risk factors.
Diagnostic Procedures for GI Bleeding
Diagnosing GI bleeding requires several important steps. These steps help find where and how much bleeding is happening. They also guide doctors in creating a treatment plan.
Endoscopy
Endoscopy lets doctors see inside the upper GI tract. They use a flexible tube with a camera to look for bleeding spots like ulcers or varices. This is done by going through the mouth.
Colonoscopy
Colonoscopy is like endoscopy but looks at the lower GI tract. A flexible tube with a camera is inserted through the rectum. It checks the colon for bleeding sources like diverticula or polyps.
Imaging Tests
Imaging tests like CT scans and angiography help find where GI bleeding is coming from. They show detailed pictures of the GI tract. These tests can spot active bleeding or other issues.
Diagnostic Procedure | Description | Area of GI Tract Examined |
Endoscopy | Visual examination using a flexible tube with a camera | Upper GI tract |
Colonoscopy | Visual examination using a flexible tube with a camera | Lower GI tract (colon) |
Imaging Tests (CT scans, Angiography) | Detailed imaging to detect bleeding or abnormalities | Entire GI tract or specific areas |
Treatment Options for GI Bleeding
Treating GI bleeding involves different steps based on the cause and how severe it is. We create treatment plans that meet each patient’s needs. This ensures they get the best care possible.
Medication Management
Medicine is key for many patients with GI bleeding. We use drugs to lower stomach acid, protect the stomach and intestines, and help them heal. Proton pump inhibitors (PPIs) and H2 blockers are often used to cut down acid. We also treat underlying conditions that might cause GI bleeding.
A top gastroenterologist says, “PPIs have changed how we treat GI bleeding by greatly lowering the chance of it happening again.”
“PPIs are effective in healing erosive esophagitis and preventing recurrent bleeding.”
Surgical Interventions
For severe GI bleeding or when other treatments don’t work, surgery might be needed. Surgery can fix or remove the bleeding source. We look at endoscopic procedures and open surgery, depending on the patient’s situation.
- Endoscopic procedures let us see and treat the bleeding spot directly.
- Open surgery is used when endoscopic methods can’t be done or fail.
Blood Transfusions
If a lot of blood is lost, blood transfusions might be needed. We watch patients’ hemoglobin levels and overall health to decide if a transfusion is needed. Blood transfusions help keep tissues and organs working right.
A medical journal notes, “Quick blood transfusions are key in severe GI bleeding. They help avoid complications and improve results.” We follow strict rules to safely give blood transfusions.
Preventive Measures for GI Bleeding
Preventing GI bleeding starts with taking proactive steps. Making smart lifestyle choices and keeping up with medical care can help. This way, you can lower your chance of getting this condition.
Lifestyle Modifications
Changing your lifestyle can help a lot in preventing GI bleeding. Dietary adjustments are key. Eating foods high in fiber can prevent constipation and reduce the risk of hemorrhoids, a common cause of GI bleeding.
Foods rich in antioxidants, like fruits and vegetables, also support your gut health. It’s important to stay hydrated too. Drinking enough water helps prevent constipation by making stool softer and easier to pass.
Also, cut down on alcohol and avoid spicy or acidic foods. These can irritate your stomach lining.
- Eat a balanced diet rich in fiber and antioxidants.
- Stay hydrated by drinking plenty of water.
- Limit alcohol consumption.
- Avoid foods that irritate the stomach.
Regular Medical Check-Ups
Regular doctor visits are key to preventing GI bleeding. This is true for people with past gut problems or those on medications that might cause bleeding. Doctors can check your health, look for issues, and adjust your treatment if needed.
They might suggest screening tests like endoscopies for those at higher risk. These tests can find and treat problems before they cause bleeding.
Monitoring Medication Use
Many drugs, like NSAIDs and anticoagulants, can raise the risk of GI bleeding. Monitoring medication use and talking to your doctor about any worries can help. It’s important to stick to the right dosage and know about any drug interactions.
In some cases, there might be safer alternatives. Doctors can help find the best options for your health.
By making lifestyle changes, going for regular check-ups, and watching your meds, you can greatly lower your risk of GI bleeding. Taking care of yourself is the best way to prevent this condition and keep your gut healthy.
The Importance of Timely Medical Attention
GI bleeding needs quick medical help to avoid serious problems. When we see signs of GI bleeding, it’s key to act fast. Delaying treatment can cause big issues, like more sickness and even death.
Consequences of Delayed Treatment
Waiting too long for medical help for GI bleeding can be very bad. Some possible problems include:
- Severe Blood Loss: This can cause anemia, tiredness, and even shock or death.
- Organ Damage: Long bleeding can harm organs because of lack of blood.
- Infection: Bleeding can cause infections, like if it’s from a peptic ulcer.
These risks show why we need to get medical help fast. Quick action can lower the chance of these problems.
Understanding the Severity of Symptoms
It’s important to know how bad GI bleeding symptoms are. Symptoms can be mild or very serious and include:
- Vomiting Blood: This means upper GI bleeding.
- Black or Tarry Stools: This shows upper GI bleeding, as the blood has been digested.
- Bright Red Blood in Stool: This means lower GI bleeding.
Knowing these symptoms helps us find the right care. If we or someone we know has these signs, we must get medical help right away.
Getting medical help quickly is not just to avoid immediate problems. It’s also to find and fix the cause of GI bleeding to stop it from happening again.
What to Expect in the ER for GI Bleeding
When you arrive at the ER, you’ll get a quick and detailed initial assessment. This is key to figuring out how serious your GI bleeding is. It helps us know who needs help the most right away.
Initial Assessment and Triage
First, we check your vital signs, medical history, and the GI bleeding details. We’ll ask about your symptoms, like when they started and how much blood you’ve lost. We also want to know if you’re feeling any pain or dizzy.
This info is important for triage. It helps us decide who to treat first based on how bad their condition is.
Tests and Procedures in the ER
After the initial check, we might do some tests and procedures to find out why you’re bleeding. These could be:
- Blood tests to see if you’re anemic or have lost a lot of blood
- Endoscopy to look at your upper or lower GI tract
- Imaging tests like X-rays, CT scans, or angiograms
- Stool tests to find blood or infection
These tools help us figure out what’s causing the bleeding. Then, we can plan the right treatment for you.
Potential Hospital Admission
If your bleeding is severe or could get worse, you might need to stay in the hospital. While you’re there, we’ll keep a close eye on you. We might do more tests or treatments, like blood transfusions or medicines to stop the bleeding.
Knowing what to expect at the ER can make things less scary. Our team is here to give you the best care possible. We want to make sure you get the help you need.
Support and Resources Available
Coping with GI bleeding is not just about medical treatment. It also needs a range of support resources. These help patients navigate their condition. Managing GI bleeding involves more than just medical needs; it also requires access to support and educational materials.
Patient Education Materials
Patient education is key in managing GI bleeding. We offer a variety of educational materials. These are designed to inform patients about their condition, treatment options, and symptom management.
Our materials cover topics like the causes of GI bleeding, diagnostic procedures, and treatment strategies. By understanding their condition, patients can better follow treatment plans and make lifestyle adjustments.
Support Groups and Counseling
Living with GI bleeding can be tough, not just physically but emotionally. That’s why we stress the importance of support groups and counseling services. These provide a safe space for patients to share their experiences and receive emotional support.
Our support groups are led by experienced professionals who know about GI bleeding. Counseling services are also available for individual support. They help patients deal with the emotional side of their condition.
Accessing Medical Care in Your Area
Accessing medical care can be a concern for patients with GI bleeding, even more so in remote or underserved areas. We provide information and assistance to help patients find medical care in their area. This includes guidance on locating specialists, understanding insurance, and navigating healthcare systems.
Resource | Description | Benefits |
Patient Education Materials | Clear, concise information on GI bleeding, its causes, diagnosis, and treatment. | Empowers patients to make informed decisions about their care. |
Support Groups | Facilitated groups for patients to share experiences and receive emotional support. | Provides emotional support, coping strategies, and a sense of community. |
Counseling Services | Individualized support for patients to navigate the emotional aspects of GI bleeding. | Helps patients cope with the emotional impact of their condition. |
Medical Care Access Assistance | Guidance on finding medical care, understanding insurance, and navigating healthcare systems. | Facilitates access to necessary medical care and specialists. |
Frequently Asked Questions about GI Bleeding
GI bleeding can be a worrying issue. People often ask about how to diagnose it, prevent it, and its long-term effects. We aim to answer these questions to help you feel more at ease.
Diagnosis of GI Bleeding
Doctors use a few steps to diagnose GI bleeding. They look at your medical history and do a physical check. They also use tests like endoscopy and colonoscopy to find the cause and how bad it is.
Preventing GI Bleeding
To prevent GI bleeding, making some lifestyle changes can help. Stay away from NSAIDs, manage stress, and eat well. Also, seeing your doctor regularly can catch problems early.
Long-term Effects of Untreated GI Bleeding
If GI bleeding isn’t treated, it can cause serious problems. These include anemia, damage to organs, and even life-threatening issues. Getting medical help quickly is key to avoiding these serious effects.
It’s important to know about diagnosing, preventing, and the long-term effects of GI bleeding. By getting medical help early and taking preventive steps, you can lower the risk of serious problems.
FAQ
What are the signs that indicate I should go to the ER for GI bleeding?
Severe blood loss, shock signs, and persistent vomiting are warning signs. Also, fainting, lightheadedness, or a fast heart rate mean you need ER care right away.
How is GI bleeding diagnosed?
Doctors use endoscopy, colonoscopy, and imaging tests to find the bleeding source. These tools help understand how bad the bleeding is.
What lifestyle changes can help prevent GI bleeding?
Avoid NSAIDs and manage stress to prevent GI bleeding. Eating well and regular doctor visits are also key. Watch your medication use closely.
What are the long-term effects if GI bleeding is not treated properly?
Untreated bleeding can cause anemia, organ failure, and even death. Quick medical help is vital to avoid these serious outcomes.
What should I expect when I visit the ER for GI bleeding?
At the ER, you’ll first get checked and triaged. Then, tests will find the bleeding cause and how bad it is. You might need to stay in the hospital for treatment.
What are the treatment options for GI bleeding?
Treatment varies based on the cause and severity. It might include medicines, surgery, or blood transfusions. These help stabilize you and fix the problem.
Can certain medications increase the risk of GI bleeding?
Yes, some meds like anticoagulants and NSAIDs raise the risk. Always talk to your doctor about your meds to know the risks.
How can I manage GI bleeding and prevent future episodes?
Managing GI bleeding means medical treatment and lifestyle changes. Regular check-ups and understanding your condition help prevent future episodes.
What resources are available for patients with GI bleeding?
There are many resources like patient guides, support groups, and counseling. They help you cope and manage your care.
When should I call 911 for GI bleeding?
Call 911 for severe symptoms like a lot of blood loss, shock signs, or trouble breathing. Seek ER care right away.
What are the risk factors for GI bleeding?
Age, gender, health conditions, and meds can raise your risk. Knowing these factors helps in prevention and early detection.
References
BMJ (British Medical Journal). Evidence-Based Medical Insight. Retrieved from https://www.bmj.com/content/310/6989/985