Last Updated on November 4, 2025 by mcelik

Gold standard test psoriatic arthritis is a term often used when discussing how doctors diagnose this complex condition. Psoriatic arthritis (PsA) affects millions worldwide, causing pain, stiffness, and disability. It’s difficult to diagnose because its symptoms often look like other types of arthritis.
Currently, there is no single gold standard test for psoriatic arthritis. Instead, doctors rely on a combination of clinical evaluations, lab tests, and imaging studies. This detailed diagnostic process helps ensure an accurate diagnosis and guides the most effective treatment plan.
Key Takeaways
- PsA diagnosis requires a detailed approach.
- No single test can confirm PsA diagnosis.
- Clinical evaluation, laboratory tests, and imaging studies are used.
- A multi-faceted approach helps identify the condition.
- Effective treatment plans can be developed with an accurate diagnosis.
Understanding Psoriatic Arthritis

Understanding the connection between psoriasis and joint inflammation is crucial for comprehending PsA.
Definition and Prevalence
PsA is closely linked to skin psoriasis. Most people with PsA also have skin and nail problems. It’s a common condition among those with psoriasis.
Common Symptoms of Psoriatic Arthritis
Symptoms include pain, stiffness, and swelling in the joints. Skin and nail issues often come with it. Each person’s symptoms can be different, making it hard to diagnose.
Understanding the connection between psoriasis and joint inflammation is crucial for comprehending PsA.
Understanding the connection between psoriasis and joint inflammation is crucial for comprehending PsA. The inflammation in PsA goes beyond just the joints. It affects other tissues too, leading to a complex condition.
Grasping this connection is essential for diagnosing and treating PsA. A complete treatment plan is needed to address both skin and joint issues.
The Challenge of Diagnosing Psoriatic Arthritis

Diagnosing psoriatic arthritis is tough because it looks like other arthritis types. This makes it hard for doctors to get it right without a detailed check-up.
Why Diagnosis Can Be Difficult
Psoriatic arthritis (PsA) is hard to diagnose because it looks like other arthritis types. Symptoms like joint pain and swelling are common in many arthritis types. So, doctors have to be careful to make the right diagnosis.
Importance of Early Detection
Understanding the connection between psoriasis and joint inflammation is crucial for comprehending PsA.
Differential Diagnosis Considerations
Doctors must think about other possible conditions when they suspect PsA. They need to rule out other diseases that have similar symptoms. A full check-up includes looking at the patient’s medical history, doing a physical exam, and running lab tests.
| Diagnostic Considerations | Description |
| Medical History | A thorough review of the patient’s medical history to identify any previous conditions or symptoms. |
| Physical Examination | A detailed physical examination to assess joint damage, swelling, and skin psoriasis. |
| Laboratory Tests | Blood tests and other laboratory tests to identify biomarkers associated with PsA. |
Understanding the challenges and importance of accurate diagnosis helps doctors manage PsA better. This improves patient results.
Clinical Evaluation Process
Clinical evaluation is key in spotting PsA. It looks at symptoms, medical history, and family background.
Initial Assessment by Healthcare Providers
A primary care doctor or general practitioner starts by checking the patient. They look for signs like joint pain, swelling, and psoriasis.
Rheumatologist Evaluation Process
A rheumatologist then checks the patient more closely. They examine the joints and other symptoms to confirm the diagnosis.
Comprehensive Medical History
Knowing the patient’s medical history is vital. Doctors ask about symptoms, past health, and family history of PsA or other diseases.
Family History in Diagnosis
Family history matters a lot in diagnosing PsA. If there’s a family history of PsA or autoimmune diseases, the risk goes up.
Previous Psoriasis Documentation
Having a history is also important. People with psoriasis are more likely to get PsA.
| Evaluation Component | Description | Importance |
| Medical History | Assessment of the patient’s symptoms and medical history | High |
| Family History | Evaluation of family history of PsA or other autoimmune diseases | High |
| Previous Psoriasis Documentation | Review of previous psoriasis diagnosis | Medium |
Physical Examination for Arthritis
A thorough physical exam is key to diagnosing psoriatic arthritis (PsA). It involves a detailed check of the patient’s condition. This helps spot important symptoms.
Joint Assessment Techniques
Understanding the connection between psoriasis and joint inflammation is crucial for comprehending PsA.
Skin Examination for Psoriasis
Checking the skin is important to find psoriasis signs, linked to PsA. Doctors search for red, scaly patches. Psoriasis is a big clue in PsA diagnosis.
Nail Changes and Their Significance
Nail changes like pitting, thickening, or separation are common in PsA. These signs help in diagnosing the condition. As one expert says,
“Nail involvement is a hallmark of PsA, and its presence can significantly influence the diagnostic process.”
Laboratory Tests for Psoriatic Arthritis
To accurately diagnose psoriatic arthritis, healthcare providers rely on various laboratory tests. These tests help identify specific markers and rule out other conditions.
Blood Tests for Psoriatic Arthritis
Blood tests are a key part of diagnosing PsA. They check the inflammation level and help rule out other arthritis types.
Inflammatory Markers
Inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are used. They show if there’s active inflammation in the body.
Rheumatoid Factor and Anti-CCP Antibodies
Tests for rheumatoid factor (RF) and anti-citrullinated protein antibodies (anti-CCP) help tell PsA from rheumatoid arthritis (RA). People with PsA usually test negative for RF and anti-CCP.
Joint Fluid Analysis
Joint fluid analysis involves taking fluid from a joint. This test can spot PsA by looking at the fluid’s characteristics.
Biomarkers for Psoriatic Arthritis
Researchers are working to find specific biomarkers for PsA. Biomarkers could help diagnose PsA early and track the disease’s progress.
Laboratory tests, including blood tests and joint fluid analysis, are vital for diagnosing and managing psoriatic arthritis.
Gold Standard Test for Psoriatic Arthritis
Understanding the connection between psoriasis and joint inflammation is crucial for comprehending PsA.
The Concept of a Diagnostic Gold Standard
A diagnostic gold standard is the most reliable test for diagnosing a condition. For PsA, this standard is vital. The disease is complex and can look like other rheumatic diseases.
CASPAR Criteria: The Current Gold Standard
The CASPAR criteria are seen as the top choice for diagnosing PsA. They use a mix of clinical, lab, and radiological findings to spot PsA accurately.
Components and Scoring System
The CASPAR criteria have several key parts:
- Evidence of psoriasis (current, past, or family history)
- Psoriatic nail disease
- Dactylitis (current or past)
- Negative rheumatoid factor
- Radiographic evidence of juxta-articular bone formation
A patient is diagnosed with PsA if they have joint, spine, or entheseal inflammation. They must score at least 3 points from the criteria.
| CASPAR Criteria | Points |
| Evidence of Psoriasis | 2 |
| Psoriatic Nail Disease | 1 |
| Dactylitis | 1 |
| Negative Rheumatoid Factor | 1 |
| Juxta-articular Bone Formation | 1 |
Validation Studies and Accuracy Rates
Many studies have shown the CASPAR criteria’s high sensitivity and specificity in diagnosing PsA. These studies prove that the criteria can accurately tell PsA apart from other arthritis types in various patient groups.
Limitations of Current Gold Standards
Even though the CASPAR criteria are a big step forward, they have their limits. Some patients might not meet the full criteria, mainly in the early stages. Researchers are working to improve these criteria.
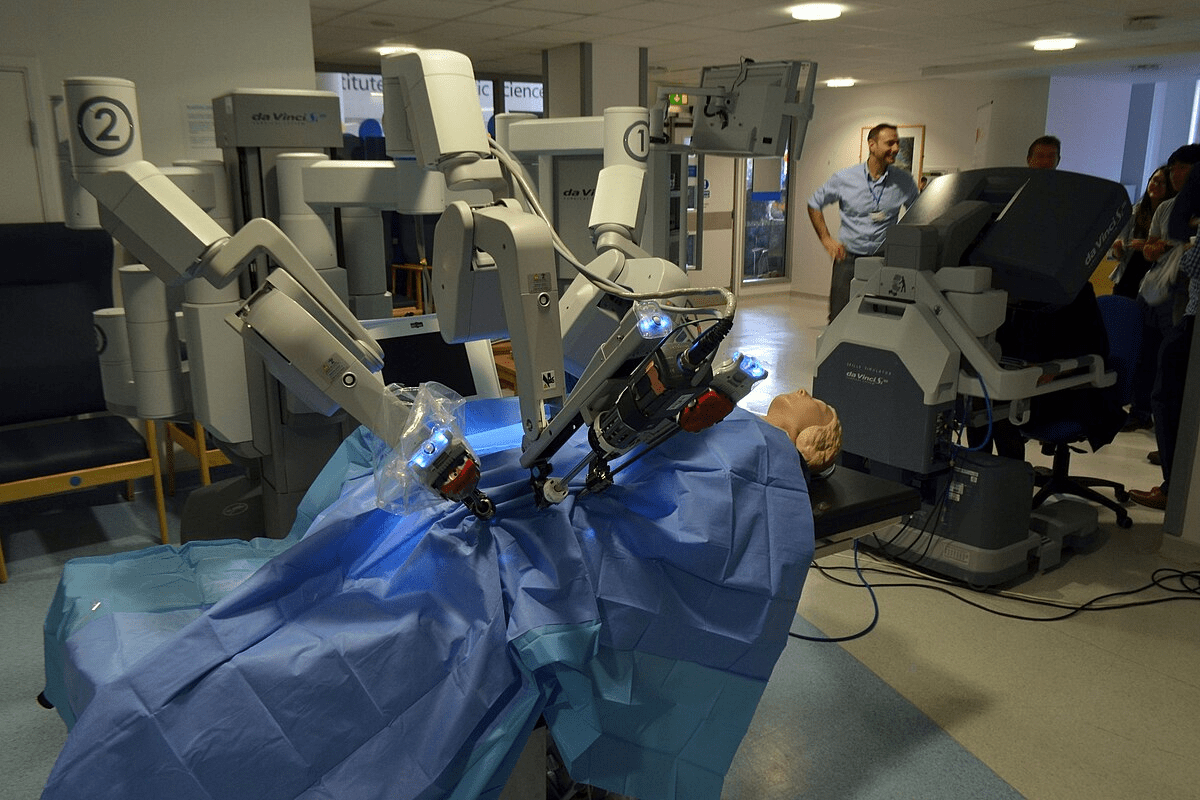
Imaging Tests for Psoriatic Arthritis
Imaging tests are key in diagnosing psoriatic arthritis (PsA) and checking joint damage. They help doctors see how joints are doing, spot damage, and plan the best treatment.
X-rays for Psoriatic Arthritis
Early detection of PsA is crucial to prevent joint damage and improve treatment outcomes.
Role of MRI in Diagnosis
Magnetic Resonance Imaging (MRI) is very good at finding PsA. It shows detailed images of bones and soft tissues. This helps spot early signs of inflammation and damage, even in the spine and joints.
Ultrasound Applications
Ultrasound is also important in diagnosing PsA. It can find signs of inflammation that X-rays miss. Plus, it helps guide injections and treatments into the right joints.
Advanced Imaging Techniques
Techniques like MRI and ultrasound are big helps in managing PsA. They give detailed views of joint health. This lets doctors create treatment plans that really fit each patient’s needs.
Criteria for Diagnosing Arthritis
The way we diagnose arthritis has changed a lot. This change has helped doctors better understand and treat psoriatic arthritis. The medical field has made these changes to improve how accurately it can diagnose the disease.
Evolution of Diagnostic Criteria
The rules for diagnosing PsA have changed a lot. Now, the CASPAR criteria are the top choice. This change shows how much we’ve learned about the disease and its different forms.
CASPAR Criteria are popular because they are very accurate. They look at things like joint problems, psoriasis, and other signs to help doctors make a diagnosis.
Comparison of Classification Systems
There are many ways to classify PsA, each with its own good points and weaknesses. Looking at these different systems helps us see when to use each one.
- The CASPAR criteria are known for being easy to use and working well for many cases.
- Other systems might focus more on certain parts of PsA, like arthritis in the limbs or back problems.
Clinical Guidelines for Testing
Guidelines suggest a detailed approach to diagnosing PsA. This includes a full medical history, physical check-ups, and lab tests.
Early diagnosis is key to starting the right treatment and improving patient results.
Research Advancements in Diagnostic Criteria
Research keeps making the diagnostic criteria better. It uses discoveries and technology to improve how accurately we can diagnose. The goal is to make treatment plans more tailored to each patient.
Understanding Test Results and Next Steps
Managing Psoriatic Arthritis starts with knowing your test results. These results help doctors create a treatment plan just for you. It’s important to understand these results well to know how severe your condition is and what treatment you need.
Interpreting Diagnostic Findings
Doctors use tests and exams to find Psoriatic Arthritis. They look for signs like psoriasis, joint swelling, and specific markers. This helps confirm if you have the condition.
Follow-up Tests for Arthritis
After the diagnosis, more tests are needed. These tests check if the treatment is working and if the disease is getting worse. Doctors might do blood tests, imaging, and check-ups to see how you’re doing.
Monitoring Disease Progression
Keeping an eye on how the disease is doing is key. Doctors will check your joints, skin, and overall health. This helps them change your treatment if needed to avoid long-term damage and improve your life.
When to Seek Second Opinions
If you’re unsure about your diagnosis or treatment, getting a second opinion is a good idea. Working with a team experienced in Psoriatic Arthritis is important for the best care.
In summary, understanding your test results and what to do next is vital in managing Psoriatic Arthritis. By working with your healthcare team and staying informed, you can play an active role in your care and improve your health.
Conclusion
Diagnosing psoriatic arthritis (PsA) needs a detailed approach. This includes clinical checks, lab tests, and imaging. Knowing the CASPAR criteria is key to a correct diagnosis and treatment plan.
A detailed clinical check is vital to spot PsA symptoms like joint swelling and skin psoriasis. Blood tests and joint fluid analysis help confirm the diagnosis by ruling out other conditions.
Using these tools, doctors can create a treatment plan tailored to each patient. This helps manage PsA symptoms and improve life quality. Accurate diagnosis and treatment are essential to prevent joint damage and ensure good health.
FAQ
What is the gold standard test for diagnosing psoriatic arthritis?
The gold standard for diagnosing psoriatic arthritis isn’t just one test. It’s a mix of clinical checks, lab tests, and imaging. The CASPAR criteria are the current top choice.
What are the common symptoms of psoriatic arthritis?
Symptoms include joint pain, stiffness, and swelling. Skin psoriasis and nail changes are also common.
Why is diagnosing psoriatic arthritis challenging?
It’s hard to diagnose because it looks like other arthritis types, like rheumatoid and osteoarthritis.
What is the role of a rheumatologist in diagnosing psoriatic arthritis?
A rheumatologist is key in confirming the diagnosis. They also help create a treatment plan.
What laboratory tests are used to diagnose psoriatic arthritis?
Tests include blood tests for inflammation markers. Joint fluid analysis is also used.
What are the CASPAR criteria, and how are they used in diagnosing psoriatic arthritis?
The CASPAR criteria combine clinical, lab, and radiological findings. They look for psoriasis, nail disease, and joint inflammation to diagnose psoriatic arthritis.
What imaging tests are used to diagnose and assess psoriatic arthritis?
X-rays, MRI, and ultrasound are used. They help spot joint damage and inflammation.
How are diagnostic findings interpreted, and what are the next steps?
Healthcare providers interpret findings. They might suggest more tests, monitor the disease, and adjust treatment plans.
What is the importance of early detection and treatment of psoriatic arthritis?
Early treatment is key to preventing joint damage. It also improves treatment results.
When should a patient seek a second opinion for psoriatic arthritis diagnosis?
Seek a second opinion if unsure about the diagnosis or treatment. Or if symptoms don’t improve with treatment.
How does a complete medical history contribute to diagnosing psoriatic arthritis?
A detailed medical history helps healthcare providers understand symptoms and history. It’s vital for an accurate diagnosis.
What is the significance of nail changes in diagnosing psoriatic arthritis?
Nail changes, like pitting or onycholysis, are common. They help confirm the diagnosis of psoriatic arthritis.
References
- Taylor, W., Gladman, D., Helliwell, P., Marchesoni, A., Mease, P., & Mielants, H. (2006). Classification criteria for psoriatic arthritis: Development of new criteria from a large international study. Arthritis & Rheumatism, 54(8), 2665–2673. https://pubmed.ncbi.nlm.nih.gov/16871531/