ANCA-associated vasculitis (AAV) is a rare autoimmune disease. It affects small and medium-sized blood vessels. This causes inflammation and tissue damage.anca positive vasculitisTest for Antibodies: The Ultimate, Simple Guide
The presence of antineutrophil cytoplasmic antibodies (ANCA) is a key sign of this condition. If not caught early, it can lead to serious organ damage.
At Liv Hospital, we use the latest diagnostic methods to find AAV. This includes three main types: granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA). Knowing how to diagnose and treat anti-neutrophil cytoplasmic autoantibody-associated vasculitis is vital for quick action.
ANCA-associated vasculitis is a group of autoimmune diseases that mainly affect small blood vessels. These diseases are marked by the presence of antineutrophil cytoplasmic antibodies (ANCA). ANCA plays a key role in how these diseases develop.
There are three main types of ANCA-associated vasculitis: Granulomatosis with Polyangiitis (GPA), Microscopic Polyangiitis (MPA), and Eosinophilic Granulomatosis with Polyangiitis (EGPA). Each type has its own symptoms and affects different organs in varying ways.
|
Type of AAV |
Characteristic Features |
Common Organ Involvement |
|---|---|---|
|
GPA |
Granulomatous inflammation, PR3-ANCA positivity |
Upper respiratory tract, lungs, kidneys |
|
MPA |
Necrotizing vasculitis, MPO-ANCA positivity |
Kidneys, lungs |
|
EGPA |
Eosinophilic infiltration, asthma, MPO-ANCA positivity |
Lungs, heart, gastrointestinal tract |
The main cause of AAV is ANCA, an autoantibody that starts the immune system’s attack on blood vessels. This attack causes inflammation and damage to the blood vessels.
“The presence of ANCA is a hallmark of this group of vasculitides, and their detection is critical for diagnosis and classification.”
The understanding of ANCA-associated vasculitis has changed a lot in the last few decades. At first, these diseases were identified by their symptoms and tissue damage. The discovery of ANCA in the 1980s changed how we classify and treat these diseases.
Knowing about ANCA’s role in AAV has helped us improve how we diagnose and treat these diseases. Understanding the history and evolution of AAV classification helps us better manage these conditions today.
It’s important to know the three main types of ANCA-associated vasculitis for good patient care. These diseases have anti-neutrophil cytoplasmic antibodies (ANCA) and cause blood vessel inflammation. The main types are Granulomatosis with Polyangiitis (GPA), Microscopic Polyangiitis (MPA), and Eosinophilic Granulomatosis with Polyangiitis (EGPA).
Granulomatosis with Polyangiitis, also known as Wegener’s granulomatosis, affects the upper and lower respiratory tract. It also causes inflammation in small to medium-sized vessels. GPA is often linked to anti-PR3 antibodies, found in about 75% of cases. Symptoms can vary but often include sinusitis, otitis media, and lung problems.
Key features of GPA include:
Microscopic Polyangiitis mainly affects small vessels with little to no immune deposits. MPA is often linked to anti-MPO antibodies, found in about 70% of cases. It often causes kidney problems and lung issues like alveolar hemorrhage.
Notable characteristics of MPA include:
Eosinophilic Granulomatosis with Polyangiitis, also known as Churg-Strauss syndrome, has eosinophil-rich inflammation in the respiratory tract. It also affects small to medium-sized vessels. EGPA is associated with asthma and eosinophilia, and ANCA is less common than in GPA and MPA.
Key features of EGPA include:
Each condition needs a specific approach for diagnosis and treatment. Knowing the differences between GPA, MPA, and EGPA is key for healthcare providers to give the best care to patients with ANCA-associated vasculitis.
Recent studies have given us new insights into ANCA-Associated Vasculitis (AAV). This includes its prevalence and how often it occurs. AAV is a rare autoimmune disorder with specific antibodies. Knowing more about AAV helps doctors diagnose and treat it better.
The numbers of AAV cases vary worldwide. Studies show that AAV affects about 198 people per million globally. The incidence rate is about 17.2 cases per million person-years. These numbers show AAV is rare but highlights the need for more research.
Most AAV cases happen to people between 50 and 60 years old. This information is key for doctors. It means middle-aged and older adults should get checked more often and might need preventive care.
Research on AAV shows some interesting trends. For example, AAV seems to affect more men, but not by a lot. Age is a big factor, with most cases happening in people between 50 and 60.
Here’s a table showing how AAV affects different age groups:
|
Age Group |
Incidence Rate (per million person-years) |
|---|---|
|
20-30 years |
5.2 |
|
40-50 years |
12.1 |
|
50-60 years |
20.5 |
|
60-70 years |
15.8 |
AAV is not spread evenly around the world. It’s more common in Europe and North America. This might be because of genetics, environment, or healthcare differences.
“The geographic variability in AAV incidence highlights the complex interplay between genetic predisposition and environmental triggers,” notes a recent review on vasculitis. “Further research is needed to understand these factors fully.”
Knowing more about AAV’s spread helps us create better health plans. As we learn more, we can improve how we diagnose and treat AAV.
ANCA-associated vasculitis (AAV) is a complex disease. It involves genetics, environment, and immune system issues. At its heart, AAV is marked by the presence of ANCA antibodies.
ANCA antibodies target neutrophils’ inner parts. They are key in AAV’s development. They activate neutrophils, causing damage to blood vessels.
When ANCA binds to neutrophils, it triggers inflammation. This leads to damage in blood vessel walls. It’s a main feature of AAV.
AAV’s autoimmune nature involves the immune system’s complex workings. It’s about losing tolerance to self-antigens and activating immune cells. This leads to ANCA production and vasculitis.
Understanding AAV’s immune system role is vital. It helps in creating effective treatments.
Genetics and environment play big roles in AAV. Genetics can affect how the immune system works. Environmental factors, like infections, can also trigger AAV.
It’s important to know how genetics and environment interact in AAV. This knowledge helps in finding new treatments. We’re working to improve patient care.
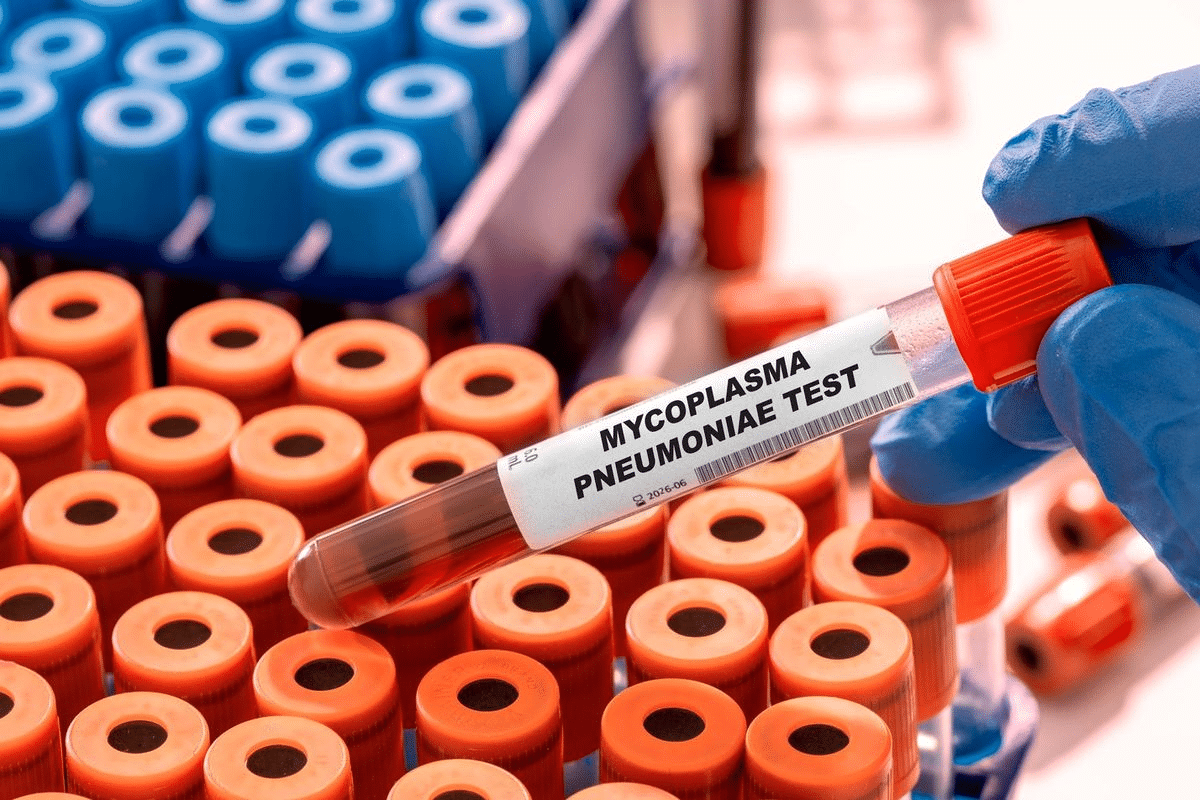
ANCA testing has changed how we diagnose and treat vasculitis. Vasculitis is a group of diseases where blood vessels get inflamed. It’s linked to the presence of ANCA and is a big deal in medicine.
We’ll look at how ANCA testing works in vasculitis. This includes the differences between C-ANCA and P-ANCA, why ANCA positivity matters, and the test’s limitations.
There are two main ANCA types: C-ANCA and P-ANCA. C-ANCA is often found in granulomatosis with polyangiitis (GPA). On the other hand, P-ANCA is more common in microscopic polyangiitis (MPA) and eosinophilic granulomatosis with polyangiitis (EGPA).
Here are some key differences:
ANCA positivity is a key marker for AAV. It helps doctors diagnose AAV, along with other symptoms and tests. ANCA testing is also used to check disease activity and predict when a patient might relapse.
ANCA testing is very useful but has its limits. Not all AAV patients test positive for ANCA. Also, ANCA can show up in other diseases, making it important to look at the whole picture.
When we look at ANCA test results, we need to consider:
Understanding ANCA testing helps us better diagnose and manage AAV. This can lead to better outcomes for patients.
People with ANCA-Associated Vasculitis (AAV) show many symptoms. These range from general complaints to specific issues with organs. The symptoms can vary a lot, making it hard to diagnose and treat.
AAV often starts with symptoms like fever, tiredness, weight loss, and feeling unwell. These symptoms are common in many diseases. They can be present for weeks or months before the disease is found.
Many patients also have systemic symptoms. These can be along with specific organ problems. Seeing these symptoms should make doctors think about AAV, along with other signs.
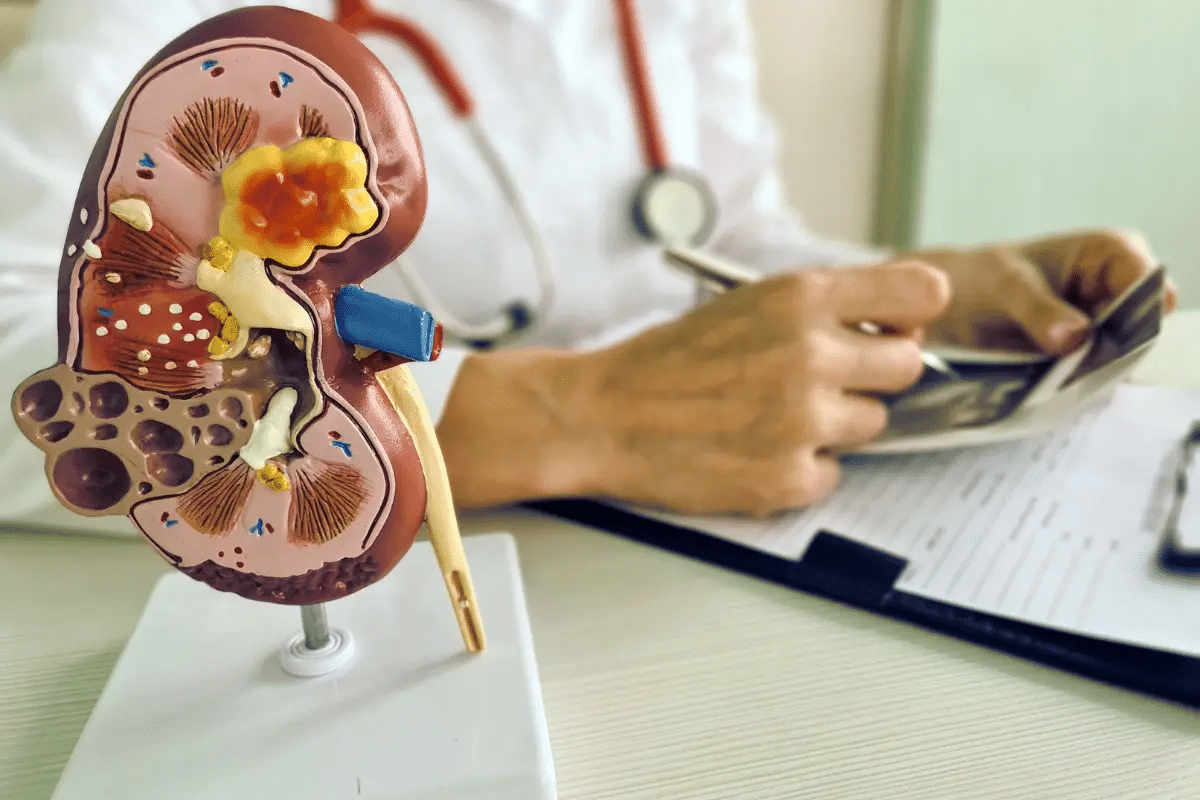
AAV can affect many organs differently. The kidneys are often hit hard, with over 75% of patients having kidney problems. These problems can range from mild to severe, even leading to kidney failure.
Other organs like the lungs, skin, and nervous system can also be affected. Lung problems can include nodules, infiltrates, or bleeding. Skin issues might be purpura, ulcers, or nodules. Neurological problems can be from nerve damage to brain vasculitis.
Because AAV can affect so many organs, a thorough check-up is key. Finding and treating it early is vital to avoid lasting damage to organs.
|
Organ/System |
Common Manifestations |
|---|---|
|
Kidneys |
Renal vasculitis, glomerulonephritis, hematuria, proteinuria |
|
Lungs |
Nodules, infiltrates, hemorrhage, cough, dyspnea |
|
Skin |
Purpura, ulcers, nodules, rash |
|
Nervous System |
Peripheral neuropathy, mononeuritis multiplex, CNS vasculitis |
A study on AAV notes, “The disease can affect any organ system. Being suspicious is key for early diagnosis and treatment.”
This shows why doctors need to know about AAV’s many symptoms. It helps them give the right care on time.
Diagnosing ANCA-Associated Vasculitis (AAV) involves several steps. We look at clinical evaluation, lab tests, and imaging studies. These methods help us accurately diagnose this condition.
The first step is a detailed clinical evaluation. We check for symptoms like kidney problems, breathing issues, and other signs of the disease. A thorough medical history and physical exam help us understand how much of the body is affected.
Labs are key in diagnosing AAV. We use tests like ANCA testing, ESR, and CRP levels. ANCA testing is important because it helps us tell if it’s Granulomatosis with Polyangiitis (GPA) or Microscopic Polyangiitis (MPA).
Imaging studies help us see how much of the body is affected. We use chest X-rays, CT scans, and MRI to check the lungs, kidneys, and other organs. These studies help us plan treatment and spot any complications.
Tissue biopsy is very important, mainly for kidney issues in AAV. We do kidney biopsies to see how much damage there is. The biopsy results help confirm the diagnosis and show how severe the disease is.
In summary, diagnosing AAV involves a detailed evaluation. This includes clinical assessment, lab tests, imaging studies, and tissue biopsy. By using all these methods, we can accurately diagnose AAV and create a good treatment plan.
Diagnosing AAV is tricky because its symptoms are not specific. It can look like other diseases, making it hard to tell them apart.
Other vasculitides can look like AAV. This makes it important to know the differences. These include:
Each condition has its own signs that help tell it apart from AAV.
|
Vasculitis Type |
Key Features |
Differentiating Factors from AAV |
|---|---|---|
|
Giant Cell Arteritis (GCA) |
Affects large and medium-sized arteries, often with headache and jaw claudication |
Typically ANCA-negative, more common in older adults |
|
Takayasu Arteritis |
Involves the aorta and its major branches, often with limb claudication |
Usually affects younger individuals, ANCA-negative |
|
Polyarteritis Nodosa (PAN) |
Medium-vessel vasculitis without glomerulonephritis or ANCA association |
Lacks ANCA positivity, different organ involvement |
Infections can look like AAV. They share similar symptoms. Examples include:
It’s important to look closely at symptoms and lab results to tell them apart from AAV.
Some cancers can have symptoms like AAV. For example:
It’s key to do a detailed check to see if cancer is present.
Other autoimmune diseases can also seem like AAV. These include:
Tests and a careful look at symptoms help tell them apart from AAV.
In conclusion, figuring out AAV is complex. It needs a detailed approach to tell it apart from other diseases.
It’s important to know the different treatments for ANCA-associated vasculitis. This condition needs a treatment plan that fits each patient’s needs and disease severity.
Induction therapy aims to get patients into remission. Rituximab and cyclophosphamide are key in this process. They are used for severe cases or when other treatments fail.
Choosing between rituximab and cyclophosphamide depends on the patient’s health and disease severity. Both can induce remission but have different side effects.
Maintenance therapy keeps patients in remission. Azathioprine and rituximab are often used. The goal is to keep remission while avoiding long-term side effects.
Regular check-ups are key during maintenance therapy. They help adjust treatment and manage side effects.
Patients with ANCA-associated vasculitis can experience relapses. To manage relapses, treatment is intensified, often going back to induction therapy.
It’s vital to catch relapse signs early. Quick action can prevent serious damage to organs.
New treatments for ANCA-associated vasculitis are being researched. These include biologics and small molecule inhibitors. They aim for more targeted therapy with fewer side effects.
These new therapies could greatly help patients who don’t respond well to current treatments.
It’s important for doctors to know about the complications and how well patients might do with ANCA-associated vasculitis. This disease can cause serious problems, both right away and later on. These issues can affect how well a patient does and their overall quality of life.
Short-term problems from ANCA-associated vasculitis can be very serious and even life-threatening. These include:
A study in a well-known medical journal found that the early stages of AAV are very risky. Infections are a big reason for sickness and death.
“The early diagnosis and treatment of AAV are critical to prevent long-term organ damage and improve patient outcomes.”
Long-term issues can really affect the life quality of patients with ANCA-associated vasculitis. These problems might include:
|
Complication |
Description |
|---|---|
|
Chronic Kidney Disease |
Progressive kidney damage leading to end-stage renal disease |
|
Cardiovascular Disease |
Increased risk of cardiovascular events due to chronic inflammation and corticosteroid use |
|
Osteoporosis |
Bone density loss associated with long-term corticosteroid therapy |
Thanks to new treatments, the outlook for patients with ANCA-associated vasculitis has gotten better. But, the 5-year death rate is 10-20%. Most deaths are from infections caused by treatments and heart problems.
Things that can affect how long a patient lives include how much of the body is affected, any other health problems, and how well they respond to treatment. Finding and treating the disease early is key to better survival rates and fewer long-term problems.
As we learn more about ANCA-associated vasculitis, it’s clear we need a team effort to care for these patients. This team approach can help improve how well patients do and make their lives better.
The journey with ANCA-associated vasculitis is complex. It involves healthcare and personal well-being. Living with this condition means managing symptoms and having a strong support system.
Patients with AAV face a big impact on their quality of life. The disease’s unpredictable nature and treatment can affect daily life. Regular assessments and adjustments to treatment plans are key to lessen its impact.
A patient advocate once said,
“Living with AAV means being prepared for anything; it’s a journey of resilience and adaptation.”
This shows the importance of being flexible and proactive in managing the condition.
Access to patient support resources is vital for AAV patients. These include counseling and support groups. They offer emotional support and practical advice, helping individuals deal with their challenges.
Support groups are great for sharing experiences and learning from others. The sense of community and understanding they provide is invaluable for coping with AAV’s emotional aspects.
Regular monitoring and follow-up care are key to managing AAV. Healthcare providers work closely with patients. They monitor the condition, adjust treatments, and address concerns or complications quickly.
Effective follow-up care goes beyond medical treatment. It includes lifestyle adjustments and patient education. This helps individuals with AAV lead active and fulfilling lives.
Understanding ANCA-Associated Vasculitis (AAV) is key for its diagnosis and care. We’ve looked into AAV’s complexities, including its definition, types, and the three main ones: Granulomatosis with Polyangiitis (GPA), Microscopic Polyangiitis (MPA), and Eosinophilic Granulomatosis with Polyangiitis (EGPA).
Early diagnosis and treatment are vital for better patient outcomes. Recognizing symptoms, using ANCA tests, and knowing other possible diagnoses help doctors create effective plans.
Managing AAV well means using induction and maintenance therapies and handling relapses. New treatments are being tested to help patients even more.
In summary, AAV needs a team effort for diagnosis and treatment. Patients and doctors working together can lead to better lives and outcomes. This shows the need for ongoing research and awareness in ANCA-associated vasculitis.
ANCA-associated vasculitis is a rare autoimmune disease. It affects blood vessels. The main types are granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA).
Symptoms vary by type and severity. They include fever, fatigue, and weight loss. Organ-specific symptoms are kidney injury, respiratory problems, and skin lesions.
Diagnosis involves clinical symptoms, lab tests, and imaging. Tests include ANCA testing, erythrocyte sedimentation rate, and C-reactive protein levels. A tissue biopsy is also used.
ANCA testing is key in diagnosing and managing the disease. C-ANCA (PR3) and P-ANCA (MPO) are the main types. ANCA positivity is a strong indicator but not definitive on its own.
Treatments include induction and maintenance therapy. They also cover relapse management and new approaches. Treatment choice depends on disease severity, patient factors, and response.
Complications include kidney injury, respiratory problems, and cardiovascular disease. Regular follow-up is vital for managing the condition and preventing relapses.
Patients with PR3-ANCA are more likely to relapse. This highlights the importance of ANCA testing in determining prognosis and guiding treatment.
The worldwide prevalence is about 198 per million persons. The incidence is 17.2 per million person-years. It varies by region, with higher rates in Europe and North America.
It can significantly impact quality of life. Patients need ongoing management and support to manage symptoms, prevent relapses, and maintain well-being.
Regular follow-up with healthcare providers is essential. It helps manage the disease, monitor activity, and prevent relapses. This improves outcomes and quality of life.
National Center for Biotechnology Information. ANCA-Associated Vasculitis: Diagnosis and Overview. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3732838/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!