Many women feel heaviness or pressure in their vagina or pelvis after childbirth. This symptom is often linked to pelvic organ prolapse. It can greatly affect a woman’s life quality.
Describing what pelvic floor heaviness feels like after childbirth and when to seek physical therapy.
Studies show that vaginal delivery raises the risk of pelvic organ prolapse. This is more than cesarean birth.
It’s important to know what pelvic floor heaviness feels like and its link to childbirth trauma. At Liv Hospital, we use a team approach to help postpartum women. We offer full care and support.
Key Takeaways
- Pelvic floor heaviness is a common symptom after childbirth.
- Vaginal delivery increases the risk of pelvic organ prolapse.
- Early intervention is key to improving life quality.
- Liv Hospital offers a team approach for postpartum care.
- Understanding symptoms is vital for effective treatment.
The Postpartum Pelvic Floor: Normal Changes vs. Concerning Symptoms

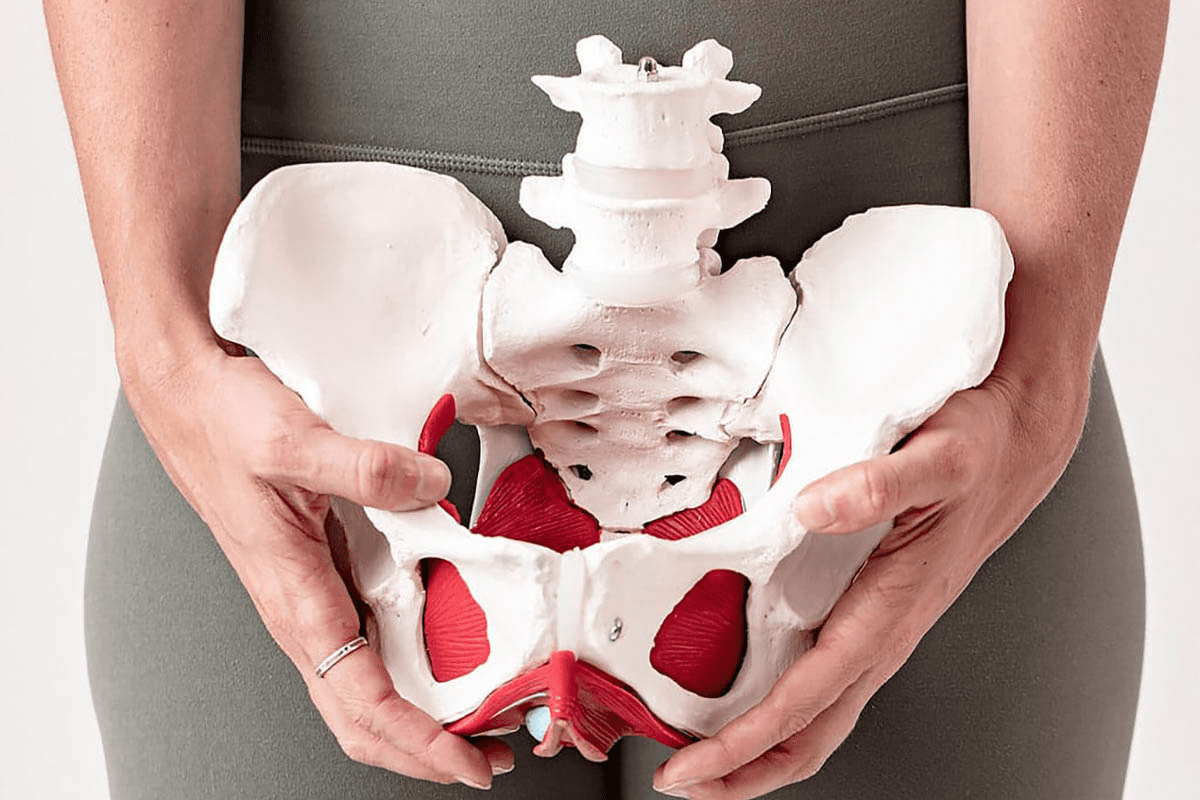
It’s important for new moms to know about the pelvic floor changes after delivery. The pelvic floor muscles stretch a lot during pregnancy and childbirth. This can weaken them, causing different symptoms after birth.
Physiological Changes After Delivery
After having a baby, the pelvic floor goes through many changes. These changes help the body heal. Some common changes include:
- Muscle Weakness: The pelvic floor muscles may become weakened due to the strain during delivery.
- Tissue Swelling: Swelling in the pelvic area is common and usually resolves on its own.
- Hormonal Shifts: Changes in hormone levels can affect muscle tone and elasticity.
Distinguishing Normal Recovery from Pelvic Floor Disorders
Some pelvic floor issues are normal after childbirth, but others are not. It’s key to know the difference. Concerning symptoms include:
- Persistent or severe pelvic pain
- Significant urinary or fecal incontinence
- A sensation of vaginal bulging or pressure
Timeline of Postpartum Pelvic Floor Healing
The healing time for the pelvic floor after childbirth varies. Generally:
- Immediate Postpartum Period (0-6 weeks): Most women see a lot of healing in the first six weeks.
- Short-term Recovery (6-12 weeks): Improvement continues, but some symptoms may stay.
- Long-term Recovery (3-6 months and beyond): Full recovery can take months, and some symptoms may last if not treated.
Knowing these changes and timelines helps new moms feel more confident during the postpartum period. It also helps them know when to seek help.
Recognizing Pelvic Floor Heaviness: Common Sensations and Symptoms

After giving birth, women may feel pelvic floor heaviness. This is a feeling of vaginal fullness or something being out of place. It’s more common than many new moms think, and knowing the symptoms is key to getting help.
The “Sitting on a Golf Ball” Sensation
Many women describe feeling like they’re sitting on a golf ball. This is like having a foreign object in the vagina, causing discomfort and pressure. It feels like sitting on something hard or bulging, which can be very upsetting.
Vaginal Pressure and Fullness Feelings
Women with pelvic floor heaviness also feel vaginal pressure and fullness. These feelings can change throughout the day. They might get worse when standing, lifting, or straining. Feeling full in the vagina can make daily activities hard and uncomfortable.
How Symptoms Change Throughout the Day
Symptoms of pelvic floor heaviness can change throughout the day. They often get worse with standing or physical activity. For many, symptoms are more noticeable in the evening after a busy day. Knowing these patterns can help manage the condition and find the right help.
Women with these symptoms should talk to healthcare providers. They can offer advice and support. Recognizing the common sensations and symptoms of pelvic floor heaviness is the first step to addressing the issue and improving recovery after childbirth.
Pelvic Organ Prolapse: The Primary Cause of Heaviness After Childbirth
Pelvic organ prolapse is often linked to childbirth. It’s a main reason for the feeling of heaviness many women feel after giving birth. This condition happens when the muscles and tissues that support the pelvic organs weaken. As a result, these organs can drop or protrude into the vagina.
This can cause various uncomfortable symptoms. These include feeling a sense of heaviness or pressure in the pelvic area.
Types of Prolapse
There are several types of pelvic organ prolapse. Each is named after the organ involved. The most common types include:
- Cystocele: This occurs when the bladder bulges into the vagina.
- Rectocele: This happens when the rectum protrudes into the vagina.
- Uterine Prolapse: This is when the uterus slips out of its normal position into the vagina.
Knowing these different types is key for diagnosing and treating prolapse effectively.
Stages of Prolapse Severity
Pelvic organ prolapse is categorized into four stages based on its severity:
Stage | Description |
1 | The organ is displaced but is within the vagina. |
2 | The organ reaches the vaginal opening. |
3 | The organ protrudes beyond the vaginal opening. |
4 | The organ is completely outside the vagina. |
This staging helps healthcare providers decide the best treatment.
Prevalence After Vaginal Delivery vs. Cesarean
Research shows that the prevalence of pelvic organ prolapse differs based on delivery method. By 15 years after delivery, 30% of women who had a vaginal delivery experience prolapse. In contrast, 9% of those who had a cesarean delivery do.
This big difference shows how vaginal delivery affects the pelvic floor.
Knowing these statistics can help women make better decisions about their care during and after childbirth.
Risk Factors That Increase Pelvic Floor Heaviness After Delivery
Many factors can lead to pelvic floor heaviness after childbirth. Knowing these factors is key to preventing and managing the issue.
Impact of Delivery Method on Pelvic Floor Integrity
The way a baby is delivered can harm the pelvic floor. Vaginal births, with or without tools like forceps, can cause more damage. A study found that instrumental deliveries are associated with a higher risk of pelvic floor disorders, including heaviness and prolapse.
It’s important to compare vaginal delivery to cesarean section. Cesareans might lower the risk of some pelvic floor problems. But, they also come with their own risks. The choice of delivery method depends on the baby’s position and the mother’s health.
Obstetric Anal Sphincter Injuries and 7.7x Higher Prolapse Risk
Obstetric anal sphincter injuries (OASIS) are a big risk for pelvic floor issues. Women with OASIS are 7.7 times more likely to have prolapse than those without. This shows how important it is to take care of the perineum during delivery.
“The occurrence of OASIS is a critical factor in the development of long-term pelvic floor dysfunction, including prolapse and incontinence.”
Pre-existing Conditions and Genetic Predisposition
Conditions like connective tissue disorders and genetic factors also play a big role. Women with a family history of pelvic floor problems are more at risk. Identifying these risk factors early in pregnancy can help in tailoring preventive measures.
Risk Factor | Description | Impact on Pelvic Floor |
Vaginal Delivery | Instrumental or complicated vaginal delivery | Increased risk of trauma and disorders |
OASIS | Obstetric anal sphincter injuries during delivery | 7.7x higher risk of prolapse |
Pre-existing Conditions | Connective tissue disorders, genetic predisposition | Increased susceptibility to pelvic floor dysfunction |
Healthcare providers can offer specific help to reduce the risk of pelvic floor problems. This is by understanding and addressing these risk factors.
Beyond Heaviness: Associated Pelvic Floor Dysfunction Symptoms
Pelvic floor dysfunction can show up in many ways after childbirth. It affects women’s health in different ways. Symptoms can greatly change a woman’s life after having a baby.
Urinary Incontinence
Urinary incontinence is a big problem for many postpartum women. About 55.8% of them deal with it. It can be from a little leak to a lot, making daily life hard.
Bowel Function Changes and Constipation
Bowel issues and constipation are common too. Childbirth puts a lot of strain on the pelvic floor muscles. Women might find it hard to go, strain a lot, or feel like they can’t empty their bowels fully.
These problems can really upset a woman’s life.
Sexual Function Impact and Dyspareunia
Pelvic floor issues can also mess with sex. Dyspareunia, or painful sex, is a big problem. It can hurt a woman’s relationship and overall happiness. Reasons include:
- Tight pelvic floor muscles
- Scars from childbirth
- Changes in hormones
Diagnosing Pelvic Floor Disorders After Childbirth
Getting a correct diagnosis for pelvic floor disorders is key for new moms after childbirth. The postpartum time can be tough. Finding the right treatment is vital for healing.
When to Seek Medical Help for Symptomatic Prolapse
If you feel a heaviness or bulge in your vagina, you should see a doctor. Symptomatic prolapse can really affect your daily life. Early treatment can stop things from getting worse. If you notice any odd symptoms or they last a while, talk to a healthcare provider.
About 30% of women get pelvic organ prolapse after vaginal birth, versus 9% after C-section. Knowing the signs and getting medical help early is key to managing it well.
Physical Examination and Assessment Procedures
A detailed physical examination is key to diagnosing pelvic floor disorders. A healthcare provider will check how bad the prolapse is, look for other issues, and check the pelvic floor’s function. This might include a speculum exam, POP-Q assessment, and other tests.
These procedures aim to check all parts of pelvic floor health. We use both clinical checks and advanced tools for a precise diagnosis.
Advanced Diagnostic Tools and Imaging
Sometimes, advanced diagnostic tools and imaging are needed to fully understand pelvic floor disorders. Ultrasound, MRI, or defecography can give us important info about the pelvic floor’s anatomy and function. These tools help us create treatment plans that fit each person’s needs.
Ultrasound can show the pelvic floor muscles’ thickness and strength. MRI gives detailed images of the pelvic area. These tools help us understand the condition better and plan effective treatments.
By using both clinical checks and advanced diagnostics, we can give a full diagnosis and a treatment plan made just for you. Our aim is to help new moms get better and keep their pelvic floor healthy.
Effective Treatments for Pelvic Floor Heaviness
Pelvic floor heaviness is a common issue after childbirth. It can be treated with several effective methods. We know it’s worrying, but there are many ways to help.
Pelvic Floor Physical Therapy and Rehabilitation
Pelvic floor physical therapy is often the first step. It helps strengthen the muscles and improve function. Pelvic floor physical therapy can significantly reduce symptoms and boost pelvic health.
Key parts of this therapy include:
- Kegel exercises to strengthen the pelvic floor muscles
- Biofeedback to help patients become aware of their pelvic floor muscle activity
- Manual therapy to release tension in the pelvic floor muscles
- Education on proper posture and body mechanics
Supportive Devices and Pessaries
Supportive devices like pessaries can also help. Pessaries are removable devices inserted into the vagina to support the pelvic organs. They come in various shapes and sizes, tailored to individual needs.
The benefits of pessaries include:
- Immediate relief from symptoms of pelvic organ prolapse
- Non-surgical management of pelvic floor disorders
- Flexibility to adjust or remove the device as needed
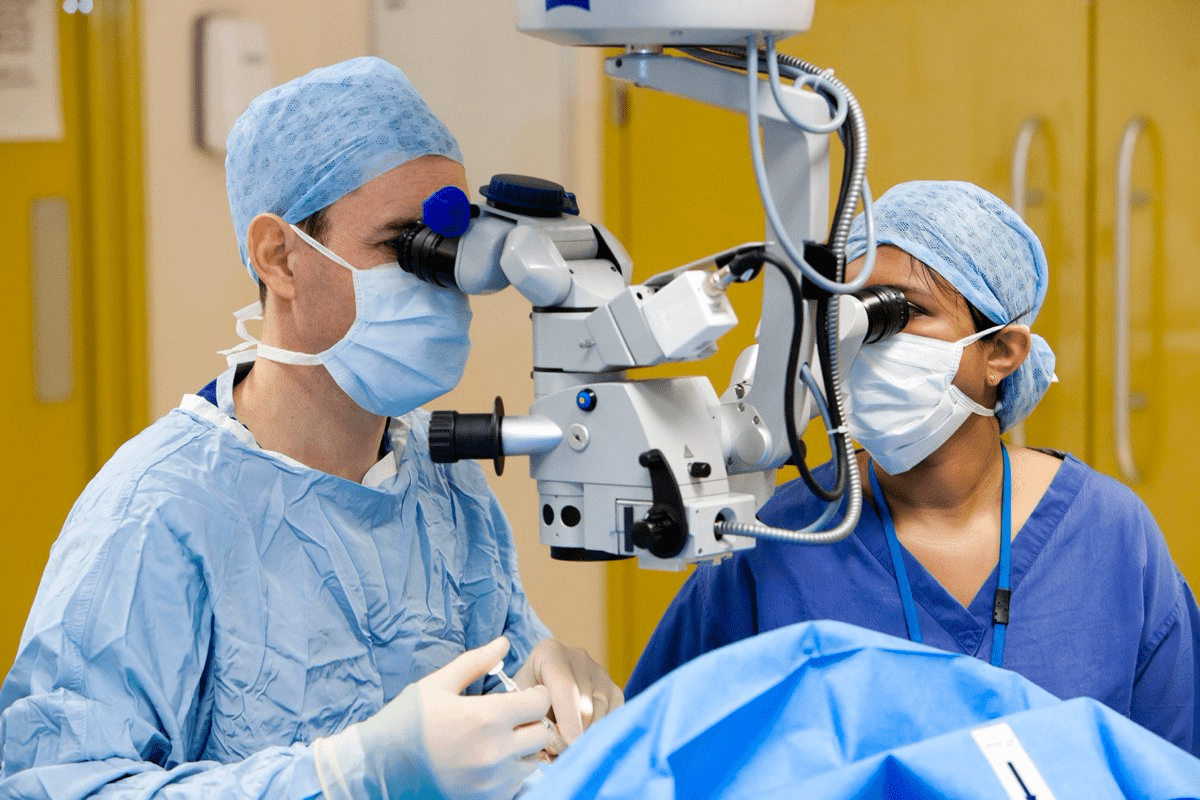
Surgical Options for Severe Prolapse
For severe cases, surgery might be needed. Surgical options can repair damaged tissues and restore normal anatomy. The right surgery depends on the prolapse’s severity, the patient’s health, and their preferences.
Lifestyle Modifications That Reduce Symptoms
Medical treatments aren’t the only solution. Lifestyle changes can also help. These include:
- Maintaining a healthy weight to reduce pressure on the pelvic floor
- Avoiding heavy lifting and bending
- Engaging in regular pelvic floor exercises
- Managing chronic coughing and constipation
Combining these lifestyle changes with medical treatments can manage pelvic floor heaviness. This improves quality of life for women.
Prevention and Recovery Strategies for Postpartum Pelvic Floor Health
Preventing and recovering from postpartum pelvic floor disorders is key. It involves prenatal prep, early postpartum care, and long-term habits. Women can greatly improve their pelvic floor health after childbirth by following these steps.
Prenatal Preparation for Pelvic Floor Protection
Prenatal prep is vital to avoid pelvic floor issues postpartum. It means learning about pregnancy and childbirth changes. It also includes doing exercises to strengthen the pelvic floor muscles.
Pelvic Floor Exercises: Kegel exercises are known for strengthening the pelvic floor. Doing them regularly during pregnancy prepares the pelvic floor for childbirth.
Early Postpartum Care and Gentle Exercises
After delivery, focus on gentle exercises and care. This helps in healing and strengthening the pelvic floor. Early postpartum care includes:
- Gentle pelvic floor exercises, such as modified Kegel exercises
- Avoiding heavy lifting and bending
- Maintaining a healthy diet to support healing
Long-term Habits for Pelvic Floor Strength Maintenance
Keeping the pelvic floor strong long-term needs ongoing commitment to healthy habits. This includes:
Habit | Benefit |
Regular Pelvic Floor Exercises | Maintains muscle strength |
Healthy Weight Management | Reduces pressure on the pelvic floor |
Avoiding Constipation | Reduces strain during bowel movements |
By making these habits part of daily life, women can lower the risk of pelvic floor disorders. They can also keep their pelvic floor healthy.
New mothers should make pelvic floor health a priority. This includes prenatal prep, postpartum care, and long-term habits. By doing this, they can lead a healthier, more active life after childbirth.
Conclusion: Navigating Life After Experiencing Pelvic Floor Changes
Understanding and managing pelvic floor changes after childbirth is key to a better life. The postpartum period brings big changes that can affect the pelvic floor. This can lead to feelings of heaviness, pressure, and discomfort.
By focusing on pelvic health and getting the right care, women can regain their strength. Treatments like pelvic floor physical therapy, supportive devices, and lifestyle changes help a lot. They can lessen symptoms and boost overall health.
Living well after childbirth means taking care of your pelvic floor. We urge women to seek medical help when needed. Also, adopting habits that strengthen the pelvic floor is important for long-term health.
FAQ
What does pelvic floor heaviness feel like after childbirth?
It feels like sitting on a golf ball. You might also feel vaginal pressure and fullness. These feelings can get worse when you stand for a long time or do physical activities.
How common is pelvic organ prolapse after vaginal delivery?
About 30% of women get pelvic organ prolapse after vaginal delivery. This is compared to 9% after cesarean delivery. It’s a big reason for pelvic floor heaviness.
What are the risk factors for increased pelvic floor heaviness after delivery?
Vaginal delivery, injuries during delivery, and pre-existing conditions are risks. Genetic factors also play a part. Women with these factors are more likely to have pelvic floor problems.
Can pelvic floor heaviness be accompanied by other symptoms?
Yes, it can. You might also have urinary incontinence, bowel changes, constipation, and sexual function issues. These include pain during sex.
How is pelvic floor disorder diagnosed after childbirth?
Doctors use a physical exam and check your symptoms. They might also use advanced tools and imaging. If you have symptoms or discomfort, see a doctor.
What treatments are available for pelvic floor heaviness?
Treatments include physical therapy, devices, and surgery for severe cases. Changing your lifestyle can also help. These changes can reduce symptoms and improve your life.
How can pelvic floor issues be prevented or their recovery promoted?
To prevent or recover, start with prenatal care and gentle exercises after birth. Keep up habits that help keep your pelvic floor strong.
What is the typical timeline for postpartum pelvic floor healing?
Healing times vary. It’s important to know what’s normal and what might be a problem. This helps new moms manage their recovery.
Can bladder prolapse cause constipation?
Yes, bladder prolapse can lead to bowel changes, including constipation. This happens because the pelvic organs are displaced.
How do I know if I have a prolapse?
Look out for symptoms like pelvic heaviness, vaginal pressure, or feeling something bulge. If you notice these, see a healthcare provider for a check-up.
Do prolapses hurt?
Some women might feel discomfort or pain. But many just feel heaviness or pressure. The pain level can vary.
Can a prolapse cause smelly urine?
Prolapse itself doesn’t cause smelly urine. But, related urinary issues or not emptying the bladder fully might. This could lead to infections and smelly urine.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3279110/