Last Updated on November 20, 2025 by Ugurkan Demir

Haemostatic disorders make it hard for the body to stop bleeding. This can cause bleeding to go on too long or be too much. It’s important to know the signs and how to manage them.Learn haemostatic disorders symptoms, causes, and key facts for diagnosis.
Bleeding disorders affect how the body clots blood. The most common one is von Willebrand disease, found in about 1% of people. The National Center for Biotechnology Information says it’s an inherited condition that can hit both men and women.
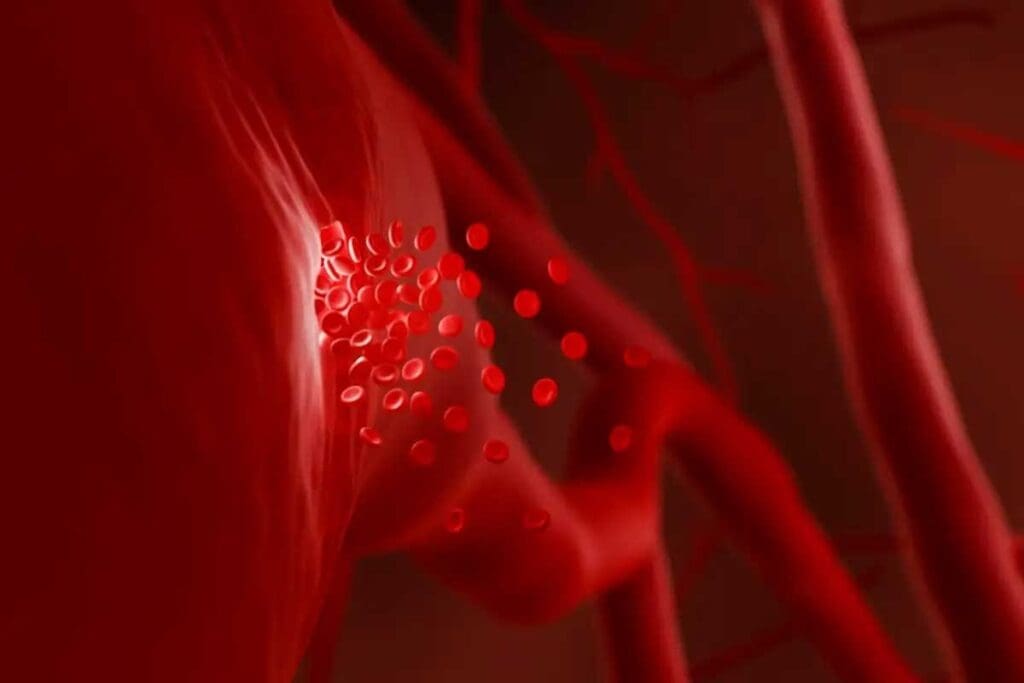
Blood clotting, or hemostasis, is a complex process. It prevents too much bleeding when a blood vessel is injured. This process involves platelets and coagulation factors working together to keep blood vessels strong.
The normal hemostasis process has several key steps. First, the injured blood vessel constricts to reduce blood flow. Then, platelets stick to the injury site, forming a platelet plug.
Coagulation factors are activated in a cascade. This leads to the formation of fibrin, which makes the clot stable.
Bleeding disorders happen when the body’s hemostatic mechanism is disrupted. This can be due to a lack or dysfunction of platelets or coagulation factors. Conditions like hemophilia and von Willebrand disease are examples, where blood doesn’t clot properly or at all.
Bleeding disorders can be inherited or acquired. Inherited disorders are passed down through genes, like hemophilia A and B. These are caused by a lack of specific clotting factors.
Acquired bleeding disorders, on the other hand, are caused by external factors. These include liver disease, vitamin K deficiency, or certain medications that affect coagulation.
| Characteristics | Inherited Bleeding Disorders | Acquired Bleeding Disorders |
| Cause | Genetic mutations affecting clotting factors | External factors like disease or medication |
| Examples | Hemophilia A and B, von Willebrand disease | Liver disease-related coagulopathy, vitamin K deficiency |
| Onset | Typically present at birth or early childhood | Can occur at any age depending on the cause |
It’s important to know the difference between inherited and acquired bleeding disorders. Inherited disorders need lifelong management. Acquired disorders may be treated by fixing the underlying cause.

Von Willebrand disease affects up to 1 percent of people worldwide. It’s the most common bleeding disorder. This condition happens when there’s not enough or working Von Willebrand factor (VWF). VWF is key for blood to clot.
Von Willebrand disease has different types based on how much or how well VWF works. The main types are:
Von Willebrand disease affects both men and women. Symptoms can differ between genders, mainly due to menstruation and childbirth in women. It’s usually passed down in families, meaning just one copy of the mutated gene is needed to cause the disorder.
Key risk factors include a family history of bleeding disorders and previous unexplained or prolonged bleeding.
Symptoms include easy bruising, nosebleeds, heavy menstrual bleeding, and prolonged bleeding after injuries or surgeries. Management aims to control bleeding and prevent future episodes.
Treatment options include:
Getting an accurate diagnosis and a personalized treatment plan is key. It helps people with Von Willebrand disease live active lives with fewer bleeding risks.
It’s important to know about Hemophilia A and B to manage these bleeding disorders. These genetic conditions cause a lack of clotting factors in the blood. This leads to prolonged bleeding.
Hemophilia A, also known as classic hemophilia, is caused by a lack of factor VIII. This protein is key for blood clotting. It’s usually passed down in an X-linked recessive pattern, hitting males more often than females.
Hemophilia B, or Christmas disease, comes from a lack of factor IX. It’s also passed down in an X-linked recessive pattern. This condition mainly affects males.
The severity of hemophilia depends on the blood’s clotting factor level. It’s classified as mild, moderate, or severe. Hemophilia follows an X-linked recessive pattern. This means males are more likely to be affected, while females are usually carriers.
Treatment for hemophilia involves replacing the missing clotting factor through factor replacement therapy. Prophylactic treatment is often used to prevent bleeding. This is key for severe cases. Regular infusions of the missing factor can greatly improve life quality for those with hemophilia.
Prophylaxis is vital in managing hemophilia. It reduces bleeding risks and improves long-term outcomes.
Managing hemophilia requires a detailed approach. This includes regular monitoring, factor replacement therapy, and educating patients. By understanding the causes and treatments for hemophilia A and B, healthcare providers can offer effective care and support.
There are many rare bleeding conditions beyond hemophilia. Each one has its own challenges and ways to manage them. These conditions make it hard for blood to clot, leading to more bleeding.
These rare conditions include deficiencies in factors XI, VII, X, and V. Each one has its own signs and needs a special approach to manage.
Factor XI deficiency is a rare bleeding disorder. It happens when there’s not enough factor XI, a key protein for clotting. People with this condition often have mild to moderate bleeding symptoms. These can happen after surgery or when they get hurt.
Factor VII deficiency is another rare condition. It’s caused by a lack of factor VII, a vital protein in clotting. Those with this deficiency might face severe bleeding episodes. These can include bleeding in the stomach or brain.
Factor X deficiency is rare and affects clotting. It’s caused by a lack of factor X. This can lead to severe bleeding complications. These can include bleeding in joints and muscles.
Factor V deficiency is a rare bleeding disorder. It’s caused by a lack of factor V, a key protein for clotting. People with this condition might have mild to severe bleeding symptoms. These can include easy bruising and bleeding that lasts longer than usual.
Understanding and managing these rare factor deficiencies is complex. Accurate diagnosis is key to treating them right. This helps prevent serious bleeding problems.
Hemostasis is a complex process that can be disrupted by platelet disorders. These disorders can be inherited or acquired. They affect platelet count or function, leading to bleeding issues.
Immune Thrombocytopenia (ITP) is a condition where the body destroys platelets. This leads to a low platelet count. Symptoms include easy bruising and bleeding.
Doctors often use corticosteroids or immunoglobulins to treat it. In severe cases, a splenectomy may be needed.
Bernard-Soulier Syndrome is a rare inherited disorder. It affects platelet function, causing thrombocytopenia and giant platelets. Patients often have bleeding issues like nosebleeds.
Glanzmann Thrombasthenia is an inherited disorder. It’s caused by a problem with the glycoprotein IIb/IIIa complex. This leads to bleeding issues and easy bruising.
Storage Pool Deficiencies are disorders that affect platelet granule secretion. This can cause mild to severe bleeding. Diagnosis involves platelet function tests.
Management may include desmopressin or platelet transfusions. Understanding these disorders is key to proper care.
By recognizing the causes and symptoms, healthcare providers can offer targeted treatments. This improves patient outcomes.
When the body’s clotting process is disrupted, it can lead to acquired bleeding conditions. These conditions are not inherited but develop due to health issues, medications, or nutritional deficiencies.
Liver disease can affect the body’s ability to form blood clots. The liver makes proteins needed for clotting, like prothrombin and fibrinogen. If the liver can’t make these proteins well, bleeding risk increases. Management involves treating the liver condition and, in some cases, administering clotting factors.
Vitamin K is key for clotting factor production. A lack of vitamin K can cause bleeding. This can happen due to poor diet, malabsorption, or certain medications. Treatment usually involves vitamin K supplements.
Certain medications can disrupt clotting, increasing bleeding risk. Anticoagulants, antiplatelet drugs, and some antibiotics are examples. Monitoring patients on these medications for bleeding signs is critical.
DIC is a complex condition with widespread clotting and bleeding. It’s a complication of conditions like sepsis, trauma, or malignancy. Managing DIC involves treating the cause and supporting clotting.
Acquired bleeding conditions can be deadly if not treated quickly. Healthcare providers must understand these conditions to provide the right care.
Knowing the signs of bleeding disorders is key to good treatment. These disorders make it hard for the body to stop bleeding. This can lead to bleeding that lasts too long or is too much.
Easy bruising is a common sign of bleeding disorders. People with these conditions bruise more easily, even from small bumps. Also, cuts or injuries might bleed for a long time.
Bleeding into joints is a sign of some bleeding disorders, like hemophilia. This can cause unexplained joint pain and swelling. It can really hurt your ability to move and enjoy life.
Women with bleeding disorders might have heavy menstrual bleeding. This means bleeding that lasts over 7 days or needs constant pad changes. It can cause anemia and other problems if not treated.
Excessive bleeding after injury or surgery is another warning sign. People with bleeding disorders might bleed a lot after surgery or injuries. This can be very dangerous if not treated right away.
Spotting these symptoms early is very important. If you or someone you know shows these signs, see a doctor right away. They can help figure out what’s wrong and how to treat it.
Diagnosing bleeding disorders needs a detailed approach. It involves many tests and evaluations. This is key to find the cause of uncontrollable bleeding and choose the right treatment.
First, tests check a patient’s coagulation status. These include a complete blood count (CBC), prothrombin time (PT), and activated partial thromboplastin time (aPTT). If these show odd results, it might mean a bleeding disorder.
After odd initial tests, more detailed studies follow. These might include tests to measure clotting factors, von Willebrand factor, and platelet function tests.
Genetic testing is key for inherited bleeding disorders. It looks at clotting factor genes for mutations that cause the disorder.
Diagnosing mild bleeding disorders is tough. Symptoms are often subtle, and some tests have limits. A careful clinical evaluation and patient history are vital.
Getting a correct diagnosis is essential. By using lab tests and clinical checks, doctors can make good treatment plans.
Managing haemostatic disorders well is key to avoiding bleeding problems. It also helps improve life quality for those with these conditions. A good plan includes ongoing care, teaching patients, and sometimes using treatments before problems start.
For those living with haemostatic disorders, constant monitoring is essential. Knowing the signs and understanding how it’s diagnosed helps manage the condition. This way, people can lower the chance of bleeding issues.
Handling bleeding disorders needs a team effort. This includes doctors, patients, and their families. Together, they can help people with haemostatic disorders live full and happy lives. This way, the disorder doesn’t stop them from doing daily things.
Putting a focus on teaching patients and using treatments early on helps. It lets people with haemostatic disorders control their condition. This reduces bleeding risks and boosts their health overall.
Haemostatic disorders are conditions that affect how the body makes blood clots. This can lead to bleeding that lasts too long or is too much.
Von Willebrand disease is the most common bleeding disorder. It happens when there’s not enough or not working right of von Willebrand factor. This protein is key for blood clotting.
Symptoms include easy bruising and bleeding that doesn’t stop. You might also have joint pain, heavy periods, and bleeding a lot after injuries or surgery.
Doctors use many tests to find bleeding disorders. These include initial tests, special coagulation studies, and genetic tests for inherited ones.
Hemophilia A and B are caused by not having enough factor VIII and factor IX. This makes it hard for blood to clot properly.
Rare factor deficiencies include conditions like factor XI, VII, X, and V deficiencies. These can cause bleeding problems.
Platelet-related disorders include immune thrombocytopenia (ITP), Bernard-Soulier syndrome, and Glanzmann thrombasthenia. These affect how platelets work or their count.
Acquired bleeding conditions include liver disease, vitamin K deficiency, and bleeding caused by medicines. Disseminated intravascular coagulation (DIC) is also one.
Managing bleeding disorders involves educating patients, using prophylactic treatments, and monitoring them. This helps prevent bleeding and improves life quality.
Desmopressin helps with von Willebrand disease and mild hemophilia A. It boosts the release of von Willebrand factor and factor VIII.
Factor replacement therapy adds the missing clotting factor. It helps prevent or treat bleeding in people with these disorders.
Centers for Disease Control and Prevention. (n.d.). Diagnosing hemophilia. U.S. Department of Health and Human Services. https://www.cdc.gov/hemophilia/testing/index.html
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!