Last Updated on December 2, 2025 by Bilal Hasdemir
Cardiac ablation is a procedure to treat irregular heartbeats. It’s generally safe but comes with risks, like stroke. A study found that the risk of stroke after cardiac ablation is a significant concern. This shows why patients need to know about possible complications. Learn what are the odds of having a stroke after an ablation. Understand the risks and the survival rates for the procedure clearly.
It’s important to understand the risks of cardiac ablation. This helps patients make better choices about their treatment. They should talk to their doctor about the risks and benefits to decide what’s best.
Key Takeaways
- Cardiac ablation carries a risk of stroke and other complications.
- Understanding the risks is key for making good choices.
- Patients should talk to their doctor about risks and benefits.
- The risk of stroke after cardiac ablation is a big worry.
- Making informed decisions can help lower risks.
Understanding Heart Ablation Procedures

For those with arrhythmias, cardiac ablation is a hopeful solution. It targets the irregular heartbeat’s source. This procedure is key in treating heart rhythm disorders.
Types of Cardiac Ablation Techniques
There are many cardiac ablation techniques. Each has its own method and use.
- Radiofrequency Ablation: This common method uses high-frequency energy to destroy heart pathways.
- Cryoablation: It freezes the area to stop abnormal heart rhythms.
- Laser Ablation: Though rare, it uses a laser to destroy tissue.
A study in the Journal of the American College of Cardiology shows the technique choice varies. It depends on the patient’s condition and the doctor’s preference.
Common Conditions Treated with Ablation
Cardiac ablation treats many heart rhythm disorders, including:
| Condition | Description | Success Rate |
| Atrial Fibrillation | Irregular heartbeat in the upper chambers of the heart | 60-80% |
| Supraventricular Tachycardia (SVT) | Rapid heartbeat originating above the ventricles | 90-95% |
| Ventricular Tachycardia | Rapid heartbeat originating in the lower chambers of the heart | 70-85% |
A top electrophysiologist says, “The success of cardiac ablation varies. It depends on the arrhythmia type and the patient’s heart health.”
“Cardiac ablation has changed how we treat arrhythmias. It gives patients a chance to live normally without irregular heartbeats.” -Electrophysiologist
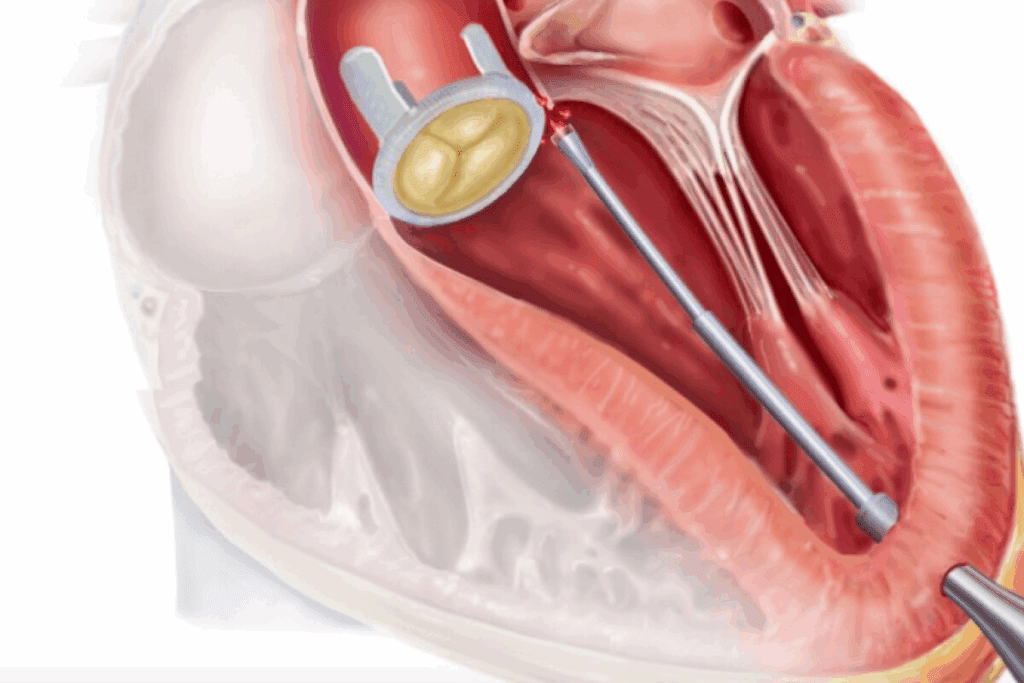
How the Procedure is Performed
The cardiac ablation procedure includes several steps:
- Preparation: The patient is sedated and given local anesthesia.
- Catheter Insertion: A catheter is inserted through a vein in the groin and guided to the heart.
- Mapping: The doctor maps the heart’s electrical activity to find the arrhythmia source.
- Ablation: The abnormal pathways are destroyed using the chosen technique.
- Monitoring: The patient’s heart rhythm is checked after the procedure to ensure success.
Knowing about cardiac ablation helps patients make better treatment choices.
Stroke as a Possible Complication of Ablation

It’s important to know about the risk of stroke after cardiac ablation. This treatment aims to fix heart rhythm problems by destroying bad electrical paths in the heart.
Mechanism of Stroke During and After Ablation
Strokes can happen during and after ablation because of blood clots. The procedure might damage the heart, leading to clots. Anticoagulation therapy helps lower this risk.
Other things can also affect stroke risk. These include the type of heart rhythm problem, any heart disease, and the patient’s health.
Statistical Risk of Stroke: The Real Numbers
Research shows the stroke risk after cardiac ablation is low but serious. Recent studies found stroke rates from 0.5% to 2% right after the procedure.
- Atrial fibrillation ablation: 0.5% to 1.5% stroke risk
- Other arrhythmia ablations: Lower risk compared to atrial fibrillation
Comparison of Stroke Risk Across Different Ablation Types
The stroke risk varies with the ablation type. For example, atrial fibrillation ablation has a higher risk than other arrhythmia treatments. This is because of the procedure’s complexity and the patient’s condition.
| Ablation Type | Stroke Risk |
| Atrial Fibrillation | 0.5% to 1.5% |
| Supraventricular Tachycardia (SVT) | Less than 0.5% |
| Ventricular Tachycardia | Variable, often higher than SVT |
Knowing these risks helps patients and doctors decide if cardiac ablation is right.
Overall Safety Profile of Cardiac Ablation
Cardiac ablation is a key treatment for heart rhythm disorders. Its safety is a big concern for both patients and doctors. Knowing about its safety helps in deciding if it’s right for you.
Success Rates of Different Ablation Types
Cardiac ablation’s success varies by type and condition. For example, atrial fibrillation ablation works for 60% to 80% of people after one try. Some studies show better results with more procedures.
Supraventricular tachycardia (SVT) ablation often succeeds more than 90% of the time. But, ventricular tachycardia ablation can have mixed results. This is because it deals with complex heart issues.
Common Side Effects and Minor Complications
Cardiac ablation is mostly safe but can have side effects. These include:
- Discomfort or pain at the catheter site
- Bruising or swelling where the catheters were inserted
- Temporary heart rhythm disturbances
- Infection at the catheter site (rare)
Most of these issues are minor and go away quickly.
Recovery Timeline and Expectations
Recovery time after cardiac ablation varies. It depends on your health and the procedure. Here’s what you might expect:
- Rest for 1-2 days after the procedure
- Start normal activities in 3-7 days
- Feel tired for up to a week
- Have check-ups to watch your heart rhythm
Knowing what to expect can make your recovery easier.
Has Anyone Died From Heart Ablation? Examining Mortality Data
It’s important to know about the risks of heart ablation. This treatment is for heart rhythm problems but can have serious side effects, including death.
Documented Cases of Ablation-Related Deaths
Even though rare, some people have died from heart ablation. These deaths are usually due to severe problems like cardiac tamponade, stroke, or pulmonary vein stenosis.
Catheter Ablation Death Rate Statistics
Looking at the death rates from catheter ablation shows they are low. The death risk is between 0.1% and 0.5%. This depends on the type of procedure and the patient’s health.
- Low-risk patients: Mortality rates are usually under 0.1%.
- High-risk patients: Those with health issues may face a higher risk, sometimes over 1%.
Comparison to Mortality Risks of Untreated Arrhythmias
It’s key to compare the risks of heart ablation to untreated arrhythmias. Untreated arrhythmias, like atrial fibrillation, raise the risk of stroke and death a lot.
| Condition | Mortality Risk |
| Untreated Atrial Fibrillation | Higher risk of stroke and mortality |
| Treated Atrial Fibrillation (with ablation) | Lower risk compared to untreated, but with procedural risks |
In summary, heart ablation does carry a risk of death, but it’s relatively low. This is compared to the risks of not treating arrhythmias.
Risk Factors That Increase Ablation Complications
Understanding the risks of heart ablation is key to avoiding complications. This procedure treats heart rhythm disorders but comes with risks. These risks are higher for some patients.
Pre-existing Conditions That Elevate Risk
Pre-existing conditions greatly affect a patient’s risk during heart ablation. Conditions like heart failure, diabetes, and kidney disease can make the procedure and recovery harder. These patients need special care before, during, and after the treatment.
- Heart failure can increase the risk of complications due to reduced cardiac reserve.
- Diabetes may affect healing and increase the risk of infection.
- Kidney disease can impact the body’s ability to handle the contrast dye used in some ablation procedures.
Age and Frailty Considerations
Age and frailty also play big roles in heart ablation risks. Older patients or those who are frail face higher risks. This is because they have less physical strength and often have other health issues.
Healthcare providers must carefully check the health of older patients. They should think about other treatments or changes to the ablation procedure to lower risks.
Procedural Complexity and Risk Correlation
The complexity of the ablation procedure is linked to the risk of complications. Longer or more complex procedures, like atrial fibrillation ablation, carry higher risks. This is compared to simpler procedures.
- Complex arrhythmias require more extensive ablation, increasing procedural time and risk.
- The use of advanced mapping technologies can help reduce risks by improving procedural accuracy.
- Experienced operators can minimize complications by optimizing procedural techniques.
Knowing these risk factors helps healthcare providers advise patients better. They can take steps to reduce complications from heart ablation.
Post-Ablation Complications Beyond Stroke
Cardiac ablation is usually safe but can cause other problems. It’s important for patients and doctors to know about these risks. This helps make better choices about the procedure.
Cardiac Tamponade and Perforation
Cardiac tamponade is a serious issue where fluid builds up around the heart. This can press on the heart and stop it from pumping well. Heart perforation during the procedure can cause this.
Risk factors for cardiac tamponade include the type of ablation, the doctor’s experience, and the patient’s heart health.
Pulmonary Vein Stenosis
Pulmonary vein stenosis is when the pulmonary veins narrow. This can cause shortness of breath and cough. It often happens after treatments for atrial fibrillation.
Vascular Access Complications
Problems can happen where catheters are inserted. These include bleeding, hematoma, and pseudoaneurysm. The size of the catheters and the patient’s blood vessels play a role in the risk.
Phrenic Nerve Injury and Esophageal Damage
Phrenic nerve injury can cause breathing problems. Esophageal damage can lead to a serious condition called atrio-esophageal fistula. Both can happen during ablation.
| Complication | Description | Risk Factors |
| Cardiac Tamponade | Fluid accumulation in the pericardial sac compressing the heart. | Type of ablation, operator experience, patient heart conditions. |
| Pulmonary Vein Stenosis | Narrowing of the pulmonary veins. | Ablation targeting atrial fibrillation. |
| Vascular Access Complications | Bleeding, hematoma, pseudoaneurysm at catheter insertion site. | Catheter size, patient vascular health. |
| Phrenic Nerve Injury | Diaphragmatic paralysis or weakness. | Ablation near the phrenic nerve. |
| Esophageal Damage | Potential for atrio-esophageal fistula. | Ablation near the esophagus. |
High Heart Rate After Catheter Ablation: Causes and Concerns
Feeling a rapid heartbeat after catheter ablation is common. It’s important to know why it happens. This procedure treats irregular heartbeats by destroying bad electrical pathways in the heart. Even though it’s safe, some people might have a fast heart rate afterward.
Normal vs. Abnormal Heart Rhythms Post-Procedure
After the procedure, the heart needs time to adjust. It’s normal for it to take some time. But, it’s key to tell if the heart rhythm is normal or not.
Tachycardia, or a fast heart rate, is a worry if it lasts or comes with other symptoms. Normal rhythms might be a bit off while the heart heals. But, if the rhythm is really off, it could mean a problem that needs doctor help.
When Tachycardia Indicates a Complication
Tachycardia might mean a problem if it’s lasting, very fast, or with symptoms like dizziness or chest pain. It could mean the ablation didn’t work fully or a new rhythm is starting.
It’s important for patients to watch their heart rate and tell their doctor about any worries. Catching problems early can make treatment work better.
Management Strategies for Post-Ablation Arrhythmias
Handling arrhythmias after ablation needs medicine, lifestyle changes, and sometimes more procedures. Anti-arrhythmic medications can help control heart rhythms. Also, avoiding stimulants and managing stress can help.
- Monitoring heart rate and rhythm
- Adhering to prescribed medication
- Making necessary lifestyle adjustments
- Follow-up appointments with the healthcare provider
In summary, a fast heart rate after catheter ablation can be scary, but knowing why it happens and when it’s a problem is key. Working with doctors can help manage arrhythmias and get the best results.
Reducing Stroke Risk During and After Ablation
Keeping stroke risk low is key during heart ablation. A mix of strategies is used before, during, and after the procedure.
Pre-Procedure Anticoagulation Protocols
Before heart ablation, patients follow special anticoagulation plans. Anticoagulation therapy uses drugs like warfarin to stop blood clots. The right drug and how long to take it depend on the patient’s risk factors.
The CHADS2-VASc score helps decide who needs more anticoagulation. Those with a higher score are at higher risk and need stronger anticoagulation before, during, and after the procedure.
Intra-Procedural Heparin Management
During the procedure, heparin is given to stop clots. The goal is to keep the activated clotting time (ACT) between 300-400 seconds. This ensures enough anticoagulation without too much bleeding risk.
Monitoring the ACT is key during the procedure. It changes based on how the patient reacts to heparin and the procedure. Adjustments to heparin are made to keep the ACT in range.
Post-Procedure Anticoagulation Guidelines
After the procedure, anticoagulation therapy continues based on risk factors. Post-procedure anticoagulation guidelines suggest using anticoagulants for weeks to months, depending on the patient’s risk.
Deciding on long-term anticoagulation depends on the patient’s condition and stroke risk. Some may stop anticoagulation if they stay in sinus rhythm. Others may need it forever.
Patient Selection: Who Should Avoid Ablation Procedures
Choosing the right patients for ablation is key. It’s about finding who can benefit the most without risks.
Absolute Contraindications
Some conditions make ablation too risky. Absolute contraindications include active infections, severe heart failure, and pregnancy. These patients should avoid ablation to prevent complications.
Active infections can cause serious problems during and after the procedure. Severe heart failure also raises the risk too high. And, pregnancy is a time when the risks of ablation are usually too great.
Relative Contraindications
Relative contraindications are conditions that increase the risk but don’t rule out ablation. These include bleeding disorders, renal failure, and significant vascular disease. The choice to do ablation depends on weighing the benefits against the risks.
For example, patients with bleeding disorders might need special care to avoid bleeding. Those with renal failure might need to adjust their blood thinners.
Risk-Benefit Analysis for High-Risk Patients
For high-risk patients, a risk-benefit analysis is critical. It compares the benefits of ablation to the possible risks and complications. The severity of symptoms, comorbidities, and overall health are considered.
A detailed assessment helps doctors decide if ablation is right. It also lets them explain the risks and benefits to patients. This ensures patients are well-informed.
Comparing Ablation Risks Across Different Heart Conditions
Different heart conditions have unique risks with ablation procedures. This makes it important to understand each condition well. Ablation treats many arrhythmias, like atrial fibrillation and ventricular tachycardia. But, the risks and side effects can change a lot based on the condition.
Atrial Fibrillation Ablation Risks
Atrial fibrillation (AFib) is a common arrhythmia treated with ablation. The goal is to block abnormal signals by isolating the pulmonary veins. While safe, risks include pulmonary vein stenosis, cardiac tamponade, and stroke.
A study in the Journal of the American College of Cardiology showed a 5% risk of major complications. The most common issues were vascular access problems and cardiac tamponade.
Ventricular Tachycardia Ablation Risks
Ventricular tachycardia (VT) ablation is for those with heart disease or cardiomyopathy. It’s considered more challenging and risky than AFib ablation. Risks include cardiac perforation and heart failure exacerbation.
| Complication | Risk Percentage |
| Cardiac Perforation | 2-3% |
| Heart Failure Exacerbation | 5-7% |
| Stroke | 1-2% |
Supraventricular Tachycardia Ablation Risks
Supraventricular tachycardia (SVT) ablation has a better risk profile than VT or AFib. It targets electrical pathways in the heart and often cures the condition.
Risks include vascular complications and AV block, but they’re rare. A study found a success rate over 95% with major complications under 1%.
The Role of Hospital Volume and Physician Experience in Outcomes
Hospital volume and physician experience are key to the success of cardiac ablation procedures. These procedures need a lot of skill and teamwork. High-volume centers often have the expertise and teamwork needed.
Impact of Operator Experience on Complication Rates
The skill of the electrophysiologist doing the ablation greatly affects the risk of complications. Studies show that doctors with more experience have fewer complications. This is because they are more skilled and know how to handle different patients and situations.
Operator experience is very important in keeping complications low during and after cardiac ablation. Experienced doctors can better predict and handle problems. This leads to better results for patients.
High-Volume vs. Low-Volume Centers
The number of cardiac ablation procedures done at a hospital also matters a lot. High-volume centers have better processes, facilities, and teams. They are more skilled at handling all kinds of cases.
| Characteristics | High-Volume Centers | Low-Volume Centers |
| Complication Rates | Lower | Higher |
| Success Rates | Higher | Lower |
| Team Expertise | More Experienced | Less Experienced |
Questions to Ask Your Electrophysiologist Before Proceeding
It’s important to talk to your electrophysiologist before cardiac ablation. Ask them these questions:
- What is your experience with performing cardiac ablation procedures?
- How many procedures do you perform annually?
- What are the complication rates for your patients?
- What measures are in place to minimize risks during and after the procedure?
These questions help you understand the risks and benefits. This way, you can make a better choice for your procedure.
Making an Informed Decision: Consent and Risk Communication
Getting informed consent for ablation means knowing your personal risks and possible complications. It’s key for patients to grasp the risks of heart ablation. This knowledge helps them make a smart choice about their treatment.
Understanding Your Personal Risk Profile
To grasp your personal risk, think about your age, health, and any existing conditions. Your doctor will look at these to figure out your risk level.
Key factors influencing your risk profile include:
- Age and frailty
- Pre-existing heart conditions
- Other health issues, such as diabetes or kidney disease
Questions to Ask Before Consenting
Before agreeing to heart ablation, ask important questions. These might be:
- What are the possible risks and complications of the procedure?
- How will my condition be managed during and after the procedure?
- What are the alternatives to ablation, and how do they compare in terms of risk and benefit?
Getting answers to these questions helps you make a better-informed choice.
Second Opinion Considerations
Getting a second opinion can give you more insight into your condition and treatment options. It’s a key step in making sure you’re making a well-informed decision.
| Consideration | Why It Matters |
| Confirming Diagnosis | Ensures that your condition is accurately diagnosed, which is vital for effective treatment. |
| Alternative Treatments | A second opinion can show you treatments you might not have thought of. |
| Procedure Details | Knowing the specifics of the procedure, including risks and benefits, helps you prepare and make informed decisions. |
By understanding your personal risk, asking the right questions, and considering a second opinion, you can make a well-informed choice about heart ablation.
Long-Term Survival Rates After Cardiac Ablation
Long-term survival after cardiac ablation is key to judging its success. This medical procedure treats heart rhythm disorders. Its success is seen in how long patients live after it.
5-Year Survival Statistics
Research shows good 5-year survival rates after cardiac ablation. For example, a study found patients with atrial fibrillation had survival rates like the general population’s.
Many factors affect these rates. These include the patient’s health, the type of arrhythmia, and the ablation technique. Patients with fewer health issues and those with supraventricular tachycardia tend to live longer.
- Atrial fibrillation ablation: 85-90% 5-year survival rate
- Supraventricular tachycardia ablation: 90-95% 5-year survival rate
- Ventricular tachycardia ablation: 70-85% 5-year survival rate
10-Year Outcomes Data
Looking at data beyond 5 years shows cardiac ablation’s long-term benefits. The 10-year survival rates are encouraging, though slightly lower than the 5-year rates.
A study over a decade found most patients kept enjoying better quality of life. Many felt relief from arrhythmia symptoms for a long time.
| Condition | 5-Year Survival Rate | 10-Year Survival Rate |
| Atrial Fibrillation | 85-90% | 75-85% |
| Supraventricular Tachycardia | 90-95% | 85-90% |
| Ventricular Tachycardia | 70-85% | 60-75% |
Quality of Life Improvements Despite Risks
Many patients see big improvements in their quality of life after cardiac ablation. The procedure can lessen symptoms and reduce medication needs.
Choosing the right patients is key to getting the most benefits while avoiding risks. Age, health, and the arrhythmia type are important in determining success.
In summary, the long-term survival and quality of life after cardiac ablation are good. It’s important to know the risks and benefits before deciding on the procedure.
Advances in Ablation Safety: New Technologies and Techniques
Medical technology has improved a lot, making cardiac ablation safer. New tools and methods are always coming out. They make these procedures safer and more effective.
Contact Force Sensing Catheters
Contact force sensing catheters are a big step forward. They let doctors control the ablation better, cutting down on risks. They give feedback on how hard the tissue is being touched, helping avoid damage.
3D Mapping Systems and Stroke Prevention
3D mapping systems are also key. They show the heart’s inside in detail, helping place ablation spots accurately. This can lower stroke risk by reducing heart catheter movement.
Combining 3D mapping with echocardiography makes the procedure safer. It lets doctors watch the heart in real-time.
Cryoablation vs. Radiofrequency Safety Profiles
Cryoablation and radiofrequency ablation are two methods used in cardiac ablation. Cryoablation uses cold, while radiofrequency uses heat. Cryoablation might be safer for some arrhythmias because it lowers the risk of blood clots.
- Cryoablation Advantages: Less chance of blood clots, less damage to the heart lining.
- Radiofrequency Ablation Advantages: It’s a proven method, works for many arrhythmias.
Robotic Ablation Systems and Precision
Robotic ablation systems are another big leap. They make procedures more precise and stable. This lets doctors treat harder cases safely.
The future of cardiac ablation looks bright. With new tech, we’ll see even better safety and results for patients.
Conclusion: Weighing the Benefits Against the Risks
Heart ablation is a complex procedure that helps many patients with cardiac arrhythmias. But, it also has risks. It’s important to know both sides to make a good choice.
The risk of stroke is a big concern. But, there are ways to lower this risk. These include using anticoagulation before the procedure and managing heparin during it. Patients need to think about these risks and the benefits of ablation, like a better quality of life and fewer symptoms.
Deciding on ablation means looking at your own risk, how bad your arrhythmias are, and possible complications. Talking to a healthcare provider about these can help you make a smart choice.
Heart ablation can be a great option for many. Knowing the risks and benefits helps you make a choice that fits your health goals and what you prefer.
FAQ
What are the odds of having a stroke after an ablation?
The chance of having a stroke after ablation depends on the type of procedure and the patient’s health. Studies show that the risk is low, between 0.5% and 1.5%. But, some patients might face a higher risk.
What is heart ablation, and how is it performed?
Heart ablation is a procedure that stops abnormal heart rhythms. It uses energy to damage a small part of the heart tissue. A catheter is inserted through a leg vein and guided to the heart to apply the energy.
What are the risks associated with heart ablation?
Heart ablation can lead to several risks, like stroke and cardiac tamponade. The risk varies based on the procedure type and patient health.
Has anyone died from heart ablation?
Yes, deaths have been linked to heart ablation. The death rate is low, between 0.1% and 0.5%. But, it’s higher for those with heart disease.
What are the risk factors that increase ablation complications?
Several factors can raise the risk of complications during ablation. These include heart disease, age, and frailty. The complexity of the procedure also plays a role.
What is the risk of cardiac tamponade during heart ablation?
Cardiac tamponade is a serious risk during ablation. It happens when fluid builds up around the heart, pressing it and affecting its function. Though rare, it’s life-threatening if not treated quickly.
How can stroke risk be reduced during and after ablation?
To lower stroke risk, several steps can be taken. These include using anticoagulation before and after the procedure, managing heparin during it, and following post-procedure guidelines.
Who should avoid ablation procedures?
Some patients should not have ablation due to health risks. This includes those with severe heart disease, pregnant women, or those with bleeding disorders. A careful evaluation is needed to decide if ablation is safe for them.
What are the long-term survival rates after cardiac ablation?
Survival rates after cardiac ablation vary. They depend on the heart condition and the patient’s health. Studies show that ablation can improve survival and quality of life for some patients.
What advances have been made in ablation safety?
New technologies and techniques have improved ablation safety. These include contact force sensing catheters, 3D mapping systems, cryoablation, and robotic systems. These advancements make ablation safer and more effective.
What is the success rate of heart ablation?
Success rates for heart ablation vary. They depend on the heart condition and the patient’s health. Studies show that ablation can be effective, with success rates between 50% and 80% for some conditions.
What are the common side effects of heart ablation?
Minor side effects of heart ablation include bruising, bleeding, and pain at the catheter site. Serious complications like stroke and cardiac tamponade can also occur.
How long does it take to recover from heart ablation?
Recovery time after heart ablation varies. It depends on the patient’s health and the type of ablation. Generally, patients recover within a few days to a week.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7486083/