Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 1 in 5 adults in the United States will develop arrhythmias, irregular heartbeats. These can greatly affect their quality of life. For many, catheter ablation is a key treatment to get a normal heart rhythm back.
The procedure‘s complexity can change a lot. It depends on the type of arrhythmia and the patient’s health. Knowing these details is very important for those thinking about this treatment.
Key Takeaways
- Catheter ablation is used to treat irregular heartbeats.
- The procedure’s complexity varies based on the type of arrhythmia.
- Individual patient conditions play a significant role in the procedure’s complexity.
- Understanding the factors affecting complexity is key for patients.
- Catheter ablation can greatly improve life quality for those with arrhythmias.
Understanding Heart Ablation
Heart ablation is a key treatment for irregular heartbeats. It’s a minimally invasive method. It uses energy to destroy the heart’s abnormal electrical pathways.
This treatment can cure many types of arrhythmias. It greatly improves the life quality of patients.
Definition and Purpose
Heart ablation destroys faulty heart pathways with energy. Its main goal is to fix the heart’s rhythm. This helps reduce symptoms like palpitations and shortness of breath.
It’s used for conditions like atrial fibrillation and SVT. Ablation targets the heart areas causing arrhythmias. It stops the abnormal signals that disrupt the rhythm.
History and Development of Ablation Techniques
Heart ablation has a long history, with big tech and technique improvements. Early methods were surgical, but catheter-based ablation made it less invasive.
Key developments in ablation techniques include:
- The introduction of radiofrequency ablation, which uses high-frequency electrical energy to heat and destroy abnormal heart tissue.
- The development of cryoablation, which uses extreme cold to freeze and destroy the targeted tissue.
- Advances in mapping technologies that allow for more precise identification of the abnormal electrical pathways.
- Improvements in catheter design, enabling more effective and safer procedures.
These advancements have made heart ablation safer and more effective. Now, it’s a good option for many with arrhythmias.
When Is Heart Ablation Recommended?
Heart ablation is a treatment for heart rhythm disorders, or arrhythmias. It depends on the arrhythmia type, its severity, the patient’s health, and their response to other treatments.
Common Arrhythmias Treated with Ablation
Ablation therapy is used for many arrhythmias. This includes atrial fibrillation, a common condition with an irregular heart rhythm.
The table below lists common arrhythmias treated with ablation and their characteristics:
| Arrhythmia Type | Description | Treatment Approach |
| Atrial Fibrillation | Irregular and rapid heart rhythm | Ablation to isolate abnormal electrical pathways |
| Atrial Flutter | Rapid heart rhythm, often with a regular pattern | Ablation to disrupt the re-entrant circuit |
| Supraventricular Tachycardia (SVT) | Rapid heart rhythm originating above the ventricles | Ablation to target the specific area causing the arrhythmia |
When Medication Fails
Ablation is considered when medication doesn’t work or causes side effects. For atrial fibrillation, ablation is recommended if meds don’t help or can’t be taken.
In summary, heart ablation is a good option for certain arrhythmias, like atrial fibrillation, when meds don’t work. Knowing when to use ablation helps patients and doctors choose the best treatment.
The Complexity of Heart Ablation Procedures
Ablation for heart conditions is a complex procedure. It needs precision and knowledge of different techniques. Finding and treating the source of arrhythmias can vary a lot between patients.
Heart ablation uses different energy sources to fix heart rhythm problems. The choice of method depends on the arrhythmia type, the patient’s health, and the doctor’s preference.
Radiofrequency Ablation
Radiofrequency ablation is a common method. It uses high-frequency electrical energy to heat and destroy bad heart pathways. It’s good for treating many arrhythmias, like atrial fibrillation and supraventricular tachycardia.
To do this, a catheter is inserted through a leg vein and guided to the heart. The catheter then sends radiofrequency energy to make lesions that stop the bad signals.
Cryoablation
Cryoablation, or cryotherapy, freezes and destroys bad pathways. It’s great for treating arrhythmias in sensitive heart areas because it causes less damage than heat methods.
It’s often used for atrioventricular nodal reentrant tachycardia (AVNRT) and other arrhythmias near important structures.
Laser and Ultrasound Ablation
Laser ablation uses a laser to make precise lesions. Ultrasound ablation uses sound waves to do the same. These methods are less common but offer options for some patients.
Each method has its own benefits and challenges. This makes heart ablation procedures complex.
| Ablation Technique | Energy Source | Primary Use |
| Radiofrequency Ablation | High-frequency electrical energy | Atrial fibrillation, supraventricular tachycardia |
| Cryoablation | Extreme cold | AVNRT, arrhythmias near critical structures |
| Laser Ablation | Laser energy | Precise lesions in heart tissue |
| Ultrasound Ablation | High-frequency sound waves | Creating lesions with minimal damage |
Pre-Procedure Preparation
To make sure the heart ablation procedure goes well, it’s key to prepare thoroughly beforehand. This step is vital for improving patient health and the success of the treatment.
Medical Evaluations and Testing
Before heart ablation, patients get checked out to see how they’re doing and what their heart is like. These checks might include:
- Electrocardiogram (ECG): This records the heart’s electrical activity.
- Echocardiogram: An ultrasound that shows the heart’s structure and how it works.
- Blood Tests: To find out if there are any health issues that could impact the procedure or recovery.
- Stress Test: This test shows how the heart does under stress.
Medication Adjustments and Restrictions
Changing medications is a big part of getting ready for heart ablation. Some medicines might need to be stopped or changed before the procedure. This is to lower the risk of problems during and after the treatment. Common changes include:
- Blood Thinners: These might be stopped to lower the chance of bleeding.
- Anti-arrhythmic Medications: These could be adjusted or stopped to better see the heart’s rhythm during the procedure.
It’s very important for patients to listen to their doctor about changing medications. This helps keep them safe and makes the heart ablation more likely to succeed.
What Happens During Heart Ablation
The heart ablation process is complex. It involves anesthesia, precise catheter navigation, and detailed heart mapping. This method is used to treat arrhythmias by targeting the heart areas causing irregular beats.
Anesthesia Options and Administration
Anesthesia is key for patient comfort during heart ablation. Conscious sedation is often used, keeping patients awake but relaxed. Sometimes, general anesthesia is used for complex or long procedures.
The choice of anesthesia depends on several factors. These include the patient’s health, the arrhythmia type, and the doctor’s preference. A study in the Journal of Cardiovascular Electrophysiology found conscious sedation is safe and effective for most ablation procedures.
“Conscious sedation provides a comfortable experience for patients while allowing for real-time feedback during the procedure.”
Catheter Insertion and Navigation
Catheter insertion is a key step. Catheters are inserted through veins in the groin or arm. Advanced imaging guides them to the heart.
Fluoroscopy and 3D mapping systems help navigate the catheters. Precision is essential to reach the right areas for ablation. A leading electrophysiologist says, “The accuracy of catheter placement is key for ablation success.”
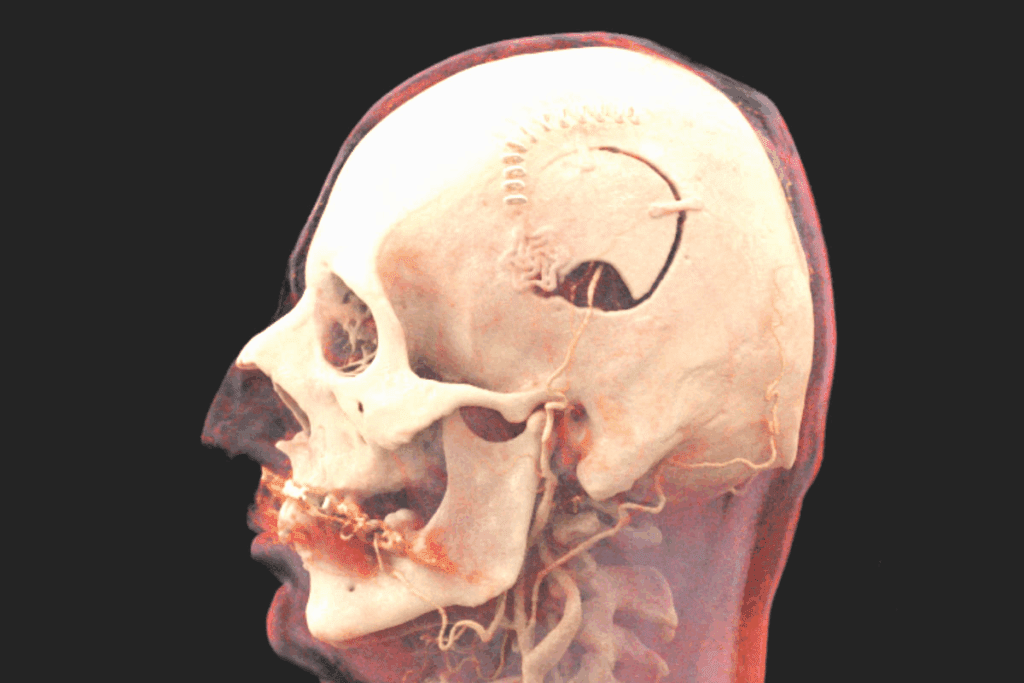
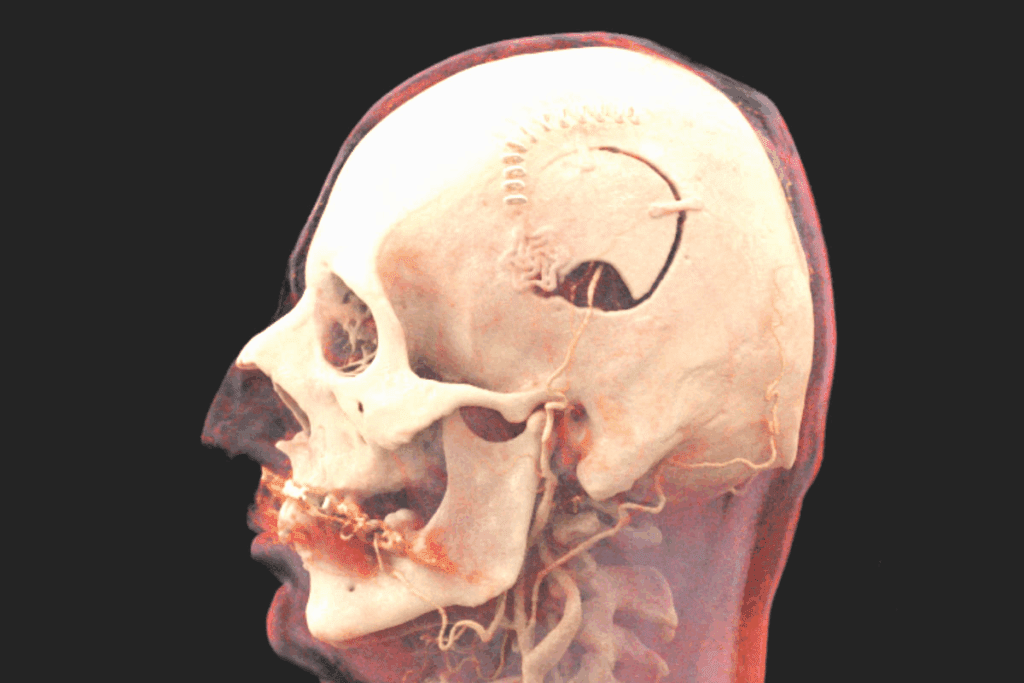
Mapping the Heart’s Electrical System
Before starting, the heart’s electrical system is mapped. Catheters record electrical signals from different heart parts. Electroanatomic mapping creates a 3D model of the heart’s electrical activity.
This mapping is vital for finding the arrhythmia source. It helps the electrophysiologist target the treatment areas. This approach increases the chance of a successful ablation.
The Ablation Process Itself
The heart ablation process is a detailed procedure aimed at fixing arrhythmias. It targets specific heart areas. The steps include finding the problem spots and using energy to fix them.
Identifying Problem Areas
Finding the arrhythmia source is key for ablation success. Electrophysiologists use advanced mapping to locate the heart’s problem spots. They create an electrical map of the heart to find these areas.
Mapping Techniques: Several mapping methods are used, including:
- Electroanatomic mapping
- Activation mapping
- Voltage mapping
These methods help pinpoint the arrhythmia source. This allows cardiologists to plan the best treatment.
Delivering Energy to Cardiac Tissue
After finding the problem spots, energy is sent to the heart tissue. This energy is used to destroy the abnormal pathways. Radiofrequency ablation and cryoablation are the methods used.
Ablation Techniques:
| Ablation Method | Description | Advantages |
| Radiofrequency Ablation | Uses heat from high-frequency electrical energy to destroy tissue. | Works well for many arrhythmias, precise control. |
| Cryoablation | Uses extreme cold to freeze and destroy pathways. | Less risk of blood clots, safe near coronary arteries. |
The ablation method chosen depends on the arrhythmia type, pathway location, and patient health.
Duration and Hospital Stay for Heart Ablation
Knowing how long heart ablation takes and how long you’ll stay in the hospital is key. The time needed for the procedure and how long you’ll stay can change a lot. This depends on many things.
Factors Affecting Procedure Length
The procedure duration for heart ablation can last from 2 to 6 hours. This depends on how complex the arrhythmia is and the method used. Cases that are more complicated or need extra steps can take longer.
- Type of arrhythmia being treated
- Technique used (radiofrequency, cryoablation, etc.)
- Patient’s overall health and presence of other medical conditions
- Experience of the electrophysiologist performing the procedure
Inpatient vs. Outpatient Procedures
Whether you’ll be treated as an inpatient or outpatient depends on a few things. This includes how complex the procedure is and your health. Some patients go home the same day, while others need to stay longer.
More patients are now treated as outpatients for heart ablation. This is thanks to better technology and techniques. But, some cases might need you to stay in the hospital for a night or longer.
Immediate Post-Procedure Care
After heart ablation, patients start a key recovery phase. This phase is vital for checking treatment success and handling any complications. It’s a time when careful monitoring and care are essential.
Recovery Room Monitoring
In the recovery room, patients’ vital signs are watched closely. This includes heart rate, blood pressure, and oxygen levels. The team looks for signs of trouble like bleeding or heart rhythm problems. Continuous ECG monitoring tracks the heart’s rhythm for any issues.
The staff also manages pain, giving medicines as needed. They check the patient’s condition and act quickly if needed.
First 24 Hours After Ablation
In the first 24 hours, patients are watched for any late complications. They get advice on activity, medication, and follow-up visits. They’re told to avoid hard work and heavy lifting.
- Watch for infection or other issues at the catheter site.
- Take the medicines as directed to manage pain and prevent heart rhythm problems.
- Go to follow-up appointments as planned to check the procedure’s success and discuss any worries.
By managing the post-procedure period well, healthcare teams can reduce risks and improve outcomes for heart ablation patients.
Recovery Timeline After Cardiac Ablation
The path to full recovery after cardiac ablation varies for everyone. Knowing the general timeline helps patients get ready for what comes next.
Short-term Recovery (1-2 Weeks)
In the first couple of weeks, patients might feel a few things. These include:
- Fatigue
- Mild discomfort or pain at the catheter site
- Palpitations or irregular heartbeats
Most people can start doing normal things again in a few days to a week. But, they should avoid hard activities for longer.
Long-term Recovery (1-3 Months)
Over the next few months, things get better. The long-term phase includes:
- Slowly getting back into physical activities
- Lessening of arrhythmia symptoms
- Regular check-ups with doctors to track progress
It’s key for patients to stick to their doctor’s advice on meds, follow-ups, and lifestyle changes for the best results.
Knowing the recovery timeline helps patients manage the post-ablation period. This way, they can get the most out of their treatment.
Potential Risks and Complications
Heart ablation is generally safe but comes with risks and complications. It’s important for patients to know these risks before deciding on this treatment.
Common Minor Complications
Minor issues after heart ablation include temporary discomfort at the catheter site, mild bruising, and swelling. Some might see minor bleeding or temporary arrhythmias. These problems usually go away quickly without needing much help.
A study found that up to 20% of patients face minor complications after catheter ablation for atrial fibrillation.
“Most of these issues are short-lived and don’t cause much trouble.”
Serious Complications
Though rare, serious problems can happen. These include cardiac tamponade, where fluid builds up around the heart, and stroke. Other serious issues are pulmonary vein stenosis and atrioventricular block, which might need a pacemaker.
- Cardiac tamponade
- Stroke
- Pulmonary vein stenosis
- Atrioventricular block
Having an experienced electrophysiologist perform the procedure is key to avoiding these serious complications.
Risk Factors That Increase Complication Rates
Some factors can raise the risk of complications during and after heart ablation. These include older age, multiple comorbidities like diabetes and hypertension, and a history of cardiac surgeries. Knowing these risk factors helps both patients and doctors make better choices.
| Risk Factor | Description |
| Older Age | Increased risk due to comorbidities and decreased physiological reserve. |
| Multiple Comorbidities | Conditions like diabetes, hypertension, and heart disease can make the procedure harder. |
| Previous Cardiac Surgeries | Scarring and changed cardiac anatomy can make the procedure more complex. |
Understanding these risk factors helps healthcare providers manage patient expectations and reduce some risks of heart ablation.
Success Rates and Effectiveness
Heart ablation is a top choice for treating many arrhythmias. Its success depends on several factors. Both patients and doctors look at how well it works when choosing treatments.
The success of heart ablation changes with each arrhythmia type. Studies show its effectiveness varies by the type of arrhythmia.
First-Time Success Rates by Arrhythmia Type
Different arrhythmias react differently to ablation. For example, atrial fibrillation has mixed success rates. For some, it works well, with up to 80% success in the first try. But for others, it might need to be done again.
Other arrhythmias like supraventricular tachycardia (SVT) and atrial flutter often see success rates over 90%. But ventricular tachycardia can have a wide range of success, depending on the heart’s condition.
| Arrhythmia Type | Success Rate Range |
| Paroxysmal Atrial Fibrillation | 70-80% |
| Persistent Atrial Fibrillation | 40-60% |
| Supraventricular Tachycardia (SVT) | 90-95% |
| Atrial Flutter | 90-95% |
| Ventricular Tachycardia | 50-80% |
Repeat Procedures: How Common and Why
Some patients need more than one ablation procedure, often for atrial fibrillation. Reasons include the arrhythmia coming back, not enough ablation the first time, or new arrhythmia issues.
A study found 20-30% of patients might need another procedure within a year. The exact number depends on the arrhythmia, patient health, and the doctor’s skill.
“The decision to proceed with a repeat ablation procedure is typically based on the severity of symptoms, the impact on quality of life, and the presence of any complications from the initial procedure.” -Electrophysiologist
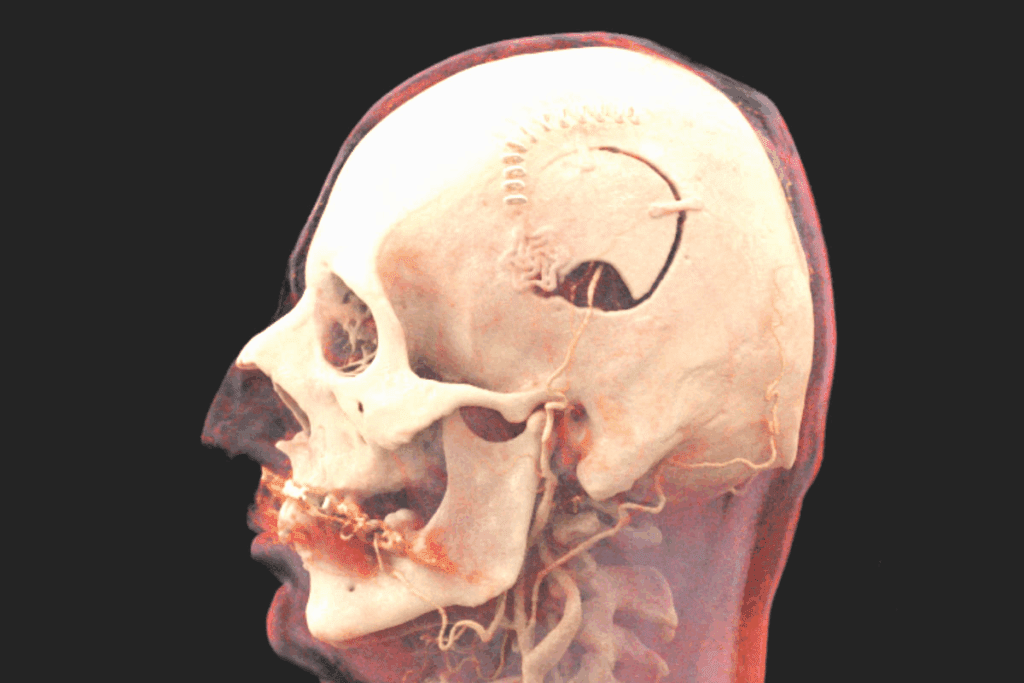
To understand heart ablation success better, look at this image:
In summary, heart ablation is very effective for many arrhythmias. But knowing the success rates and the chance of needing more procedures is key for patient care.
Who Is a Good Candidate for Heart Ablation?
Choosing to have heart ablation depends on several factors. These include the type of arrhythmia and the patient’s overall health. It’s for those with arrhythmias that don’t respond well to medication or other treatments.
Ideal Patient Profiles
Good candidates for heart ablation have symptomatic arrhythmias that really affect their life. These can be atrial fibrillation, supraventricular tachycardia (SVT), and ventricular tachycardia. They’ve tried other treatments but haven’t seen good results.
| Arrhythmia Type | Success Rate with Ablation | Typical Candidate Profile |
| Atrial Fibrillation | 60-70% | Symptomatic, failed medication |
| Supraventricular Tachycardia (SVT) | 80-90% | Frequent episodes, medication intolerant |
| Ventricular Tachycardia | 50-60% | Life-threatening episodes, structural heart disease |
Contraindications and High-Risk Factors
Heart ablation is effective for many, but there are risks. Those with severe heart failure, active infections, or significant renal impairment face higher risks. Also, pregnant women or those with certain metal implants might not be good candidates for some ablation types.
It’s key for those thinking about ablation to see a cardiologist or electrophysiologist. They’ll check the patient’s medical history, current health, and arrhythmia details. This helps decide if the procedure is right for them.
Choosing the Right Electrophysiologist
Finding the right electrophysiologist is key for a successful heart ablation. An electrophysiologist is a cardiologist with extra training in heart rhythm disorders. They will guide you from the start to after the procedure.
Qualifications to Look For
When looking for an electrophysiologist, consider these qualifications:
- Board Certification: Make sure they are certified in cardiology and electrophysiology.
- Experience: Choose someone with lots of experience in heart ablation.
- Specialized Training: Some may have extra training in certain techniques.
- Hospital Affiliation: Check the quality of the hospital they work at.
Questions to Ask Your Doctor
Ask the right questions during your first meeting. This will help you understand their expertise and care approach. Here are some important questions:
- What experience do you have with heart ablation procedures?
- What are the possible risks and complications for my condition?
- What kind of care and follow-up can I expect after the procedure?
- Are there other treatments or procedures that might be better for me?
By choosing the right electrophysiologist and discussing your treatment, you can greatly improve your heart ablation’s success.
Alternatives to Cardiac Ablation
Cardiac ablation is not the only way to treat arrhythmias. Other good options include medication management and interventional procedures. Some patients might find these alternatives better than ablation.
Medication Management Strategies
Medication is key in treating arrhythmias. Doctors use different drugs to keep the heart rhythm right. These include beta-blockers, anti-arrhythmic drugs, and calcium channel blockers. The right drug depends on the arrhythmia type, the patient’s health, and more.
- Beta-blockers: Good for managing heart rate in atrial fibrillation.
- Anti-arrhythmic drugs: Keep the heart rhythm normal.
- Calcium channel blockers: Used when beta-blockers don’t work well.
Other Interventional Procedures
There are other ways to treat arrhythmias, aside from cardiac ablation. These include:
- Pacemaker implantation: Controls heartbeat with electrical impulses.
- Implantable cardioverter-defibrillators (ICDs): Prevent sudden death from dangerous arrhythmias with an electric shock.
- Cardiac resynchronization therapy (CRT): Treats heart failure by coordinating heart contractions.
These options give patients different ways to manage arrhythmias. It’s important to talk to a healthcare provider to find the best treatment.
Cost and Insurance Considerations
Knowing the financial side of heart ablation is key for those thinking about it. The cost can change a lot. This depends on the procedure’s complexity, where it’s done, and your insurance.
Average Costs in the United States
This price includes the procedure, hospital stay, and aftercare. It’s important for patients to ask their healthcare provider for a detailed cost breakdown.
Insurance Coverage and Requirements
Insurance for heart ablation varies by provider and policy. Most plans cover it when it’s medically needed, but you might have to pay out-of-pocket for things like deductibles and copays. It’s vital to check your insurance before the procedure.
To make sure you’re covered, see if your insurance needs pre-approval or has special rules for this procedure. Knowing this can help you avoid surprise medical bills.
Conclusion
Heart ablation is a complex medical procedure that needs careful thought and preparation. We’ve looked at its definition, purpose, and the different techniques used in this article.
Understanding heart ablation well is key for patients to make good treatment choices. By summarizing the main points, we see that it’s a good option for some heart rhythm disorders. It can greatly improve a person’s quality of life.
In conclusion, heart ablation is a detailed procedure that requires a deep understanding of its complexities, risks, and benefits. Patients should talk to their healthcare providers to find the best treatment. This ensures they get the most effective care for their condition.
FAQ
What is heart ablation?
Heart ablation, also known as catheter ablation, is a procedure to treat arrhythmias. It destroys the abnormal electrical pathways in the heart.
What is the purpose of heart ablation?
Heart ablation aims to restore a normal heart rhythm. It eliminates the source of arrhythmia, improving symptoms and reducing complications.
How is heart ablation performed?
To perform heart ablation, catheters are inserted through a vein in the leg. They are guided to the heart to destroy the abnormal pathways.
What are the different types of energy used in heart ablation?
Heart ablation uses various energies like radiofrequency, cryoablation, laser, and ultrasound.
What is radiofrequency ablation?
Radiofrequency ablation uses heat from high-frequency electrical energy. It destroys abnormal electrical pathways in the heart.
How long does a heart ablation procedure take?
The procedure’s length varies based on the case’s complexity and the technique. It usually takes 2 to 4 hours.
What kind of anesthesia is used during heart ablation?
Anesthesia options include conscious sedation or general anesthesia. They ensure patient comfort during the procedure.
What are the possible risks and complications of heart ablation?
Risks include minor complications like bruising and bleeding. Serious complications like cardiac tamponade, stroke, and pulmonary vein stenosis are also possible.
How successful is heart ablation?
Success rates vary by arrhythmia type. Studies show success rates from 60% to 90% for conditions like atrial fibrillation.
Can heart ablation be repeated if it is not successful the first time?
Yes, heart ablation can be repeated if needed. The decision depends on the patient’s condition and the electrophysiologist’s advice.
How do I choose the right electrophysiologist for heart ablation?
Look for a board-certified electrophysiologist. Ask about their experience and success rates with heart ablation procedures.
Are there alternatives to heart ablation?
Yes, alternatives include medication management and other interventional procedures. They depend on the patient’s condition and arrhythmia severity.
How much does heart ablation cost?
Costs vary by location, hospital fees, and insurance. In the U.S., costs range from $20,000 to $50,000 or more.
Is heart ablation covered by insurance?
Coverage varies by insurance provider and policy. It’s important to check with your insurance to understand coverage and any out-of-pocket costs.
What is the recovery time after heart ablation?
Recovery time varies, but most patients recover within a few weeks. Some may see gradual improvement over several months.
References
National Institutes of Health. Evidence-Based Medical Insight. Retrieved from https://www.nhlbi.nih.gov/health-topics/catheter-ablation