Last Updated on November 25, 2025 by Ugurkan Demir
At Liv Hospital, we know how important it is to tackle heart block disease. This condition happens when the heart’s electrical signals are delayed or blocked. It can cause serious health problems. So, it’s key to understand the types, symptoms, and treatments available.
Heart block disease is when the heart’s electrical system gets disrupted. This leads to slowed or blocked signals between the atria and ventricles. Knowing about this condition is essential for managing and treating it well.
Key Takeaways
- Heart block disease affects the heart’s electrical system.
- Delayed or blocked impulses can lead to serious health issues.
- Understanding the types and symptoms is vital for effective treatment.
- Liv Hospital offers complete care for heart block disease.
- Multidisciplinary expertise ensures patient-focused treatment plans.
Understanding the Heart’s Electrical System

The heart’s electrical system is complex. It controls the heartbeat, making sure blood flows well throughout the body. Knowing how it works is key to understanding heart block disease.
Normal Conduction Pathways
The heart’s electrical pathway starts with the sinoatrial (SA) node in the right atrium. This node is the heart’s natural pacemaker. It sends electrical impulses through the atria, making them contract.
These impulses then go to the atrioventricular (AV) node. This node delays the signal. This delay lets the ventricles fill with blood before they contract.
The signal then goes through the Bundle of His. It splits into the left and right bundle branches. Then, it reaches the Purkinje fibers, making the ventricles contract. This ensures the heart beats in sync, pumping blood well.
Key components of the heart’s electrical system include:
- The sinoatrial (SA) node
- The atrioventricular (AV) node
- The Bundle of His
- The bundle branches
- The Purkinje fibers
How Electrical Signals Control Heartbeats
Electrical signals are vital for controlling heartbeats. They determine the heart rate and rhythm. Normally, the SA node sends impulses at a rate for a resting heart rate of 60-100 beats per minute.
When the signal reaches the ventricles, it makes them contract. This pumps blood out of the heart. The timing of atrial and ventricular contractions is key for good blood flow.
“The heartbeat is the result of a highly coordinated electrical activity that involves multiple structures within the heart.”
| Component | Function |
| SA Node | Generates electrical impulses |
| AV Node | Delays electrical impulses |
| Bundle of His | Transmits impulses to ventricles |
Understanding the heart’s electrical system is essential for diagnosing and treating heart block disease. Problems in this system can cause irregular heartbeats and other issues.
What Is Heart Block Disease
Heart block disease happens when the heart’s electrical signals are delayed or blocked. This condition affects the heart’s electrical system. It leads to irregular heartbeats.
Definition and Basic Concepts
Heart block disease is when the electrical signals that control the heartbeat are disrupted. The heart’s electrical system is key for a regular rhythm. Any problem here can cause arrhythmias or other issues.
It can be caused by aging, heart disease, or certain medications. Knowing the basics of heart block disease is vital for diagnosis and treatment.
Disruption of Electrical Impulses
The heart’s electrical impulses are vital for controlling the heartbeat. When these impulses are disrupted, it can cause delayed or blocked signals. This can happen at different levels, such as:
- The sinoatrial (SA) node, where electrical impulses are generated
- The atrioventricular (AV) node, where impulses are delayed or blocked
- The bundle of His, where impulses are transmitted to the ventricles
Impact on Heart Function
Heart block disease can significantly affect heart function. The severity of the blockage determines the impact. It can lead to:
- Irregular heartbeats (arrhythmias)
- Reduced heart rate (bradycardia)
- Increased risk of heart failure
Understanding how heart block disease affects heart function is key for effective treatment plans.
Types of Heart Block Disease
Heart Block Disease is divided into three main types. These are based on how much the heart’s electrical system is blocked. The types are first-degree, second-degree, and third-degree heart block. Each type shows a different level of disruption in the heart’s electrical impulses.
First-Degree Heart Block
First-degree heart block means there’s a delay in the electrical signal from the atria to the ventricles. This delay shows up on an electrocardiogram (ECG) as a long PR interval. First-degree heart block usually doesn’t cause symptoms and might not need treatment, just watching it.
Second-Degree Heart Block
Second-degree heart block happens when the electrical signal sometimes can’t reach the ventricles. There are two kinds: Mobitz Type 1 (Wenckebach) and Mobitz Type 2. Mobitz Type 1 shows a PR interval getting longer until a beat is missed. Mobitz Type 2 just stops the impulse without warning.
Third-Degree (Complete) Heart Block
Third-degree heart block, or complete heart block, means the atria and ventricles don’t work together. The ventricles beat slower than the atria. This can cause serious symptoms and often needs a pacemaker.
The table below shows the main features of each heart block type:
| Type of Heart Block | ECG Characteristics | Symptoms | Treatment |
| First-Degree | Prolonged PR interval | Often asymptomatic | Monitoring |
| Second-Degree Type 1 | Progressive PR prolongation until a beat is dropped | Variable symptoms | Monitoring, sometimes pacemaker |
| Second-Degree Type 2 | Sudden failure of impulse conduction | Often symptomatic | Pacemaker |
| Third-Degree | Complete dissociation between atria and ventricles | Significant symptoms | Pacemaker implantation |
First-Degree Heart Block in Detail
First-degree heart block is the mildest form of heart block. It’s often found during tests for other conditions. This condition causes a delay in electrical signals from the atria to the ventricles. Most people don’t notice symptoms, and it’s usually found by chance during an electrocardiogram (ECG).
Characteristics and ECG Findings
The main sign of first-degree heart block is a long PR interval on an ECG. The PR interval is the time from the start of atrial depolarization to the start of ventricular depolarization. In this condition, this interval is longer than 0.2 seconds.
ECG Findings:
- Prolonged PR interval (>0.2 seconds)
- Every P wave is followed by a QRS complex
- No dropped beats
To spot first-degree heart block, an ECG is key. It shows the heart’s electrical activity clearly. This helps doctors diagnose it accurately.
Prognosis and Management
People with first-degree heart block usually have a good outlook. It often doesn’t get worse. But, regular checks are needed to catch any changes.
Management Strategies:
- Regular check-ups with a healthcare provider
- Periodic ECGs to monitor the condition
- Addressing underlying conditions that may contribute to heart block
- Avoiding medications that can worsen the condition
Most of the time, first-degree heart block doesn’t need special treatment. But, it’s important to manage any heart disease or other conditions that might be causing it.
Knowing about first-degree heart block helps manage it well. By following the right steps, people with this condition can live healthy lives.
Second-Degree Heart Block: Type 1 vs Type 2
It’s important to know the difference between Mobitz type 1 and Mobitz type 2 second-degree heart block. This condition happens when the heart’s electrical signals don’t always reach the ventricles. It’s split into two types based on how the blockage occurs.
Distinguishing Features of Mobitz Type 1
Mobitz type 1, or Wenckebach block, shows a growing PR interval until a beat is missed. This means the heart’s electrical signals get longer and longer until a beat is skipped. Then, the pattern starts over. This “lengthening” of the PR interval is key to Mobitz type 1.
Distinguishing Features of Mobitz Type 2
Mobitz type 2, on the other hand, has a sudden failure of electrical impulses without a growing PR interval. Unlike Mobitz type 1, the PR interval stays the same before a beat is missed. This unpredictability makes Mobitz type 2 more dangerous, as it can lead to a complete block without warning.
Clinical Significance of Each Type
The difference between Mobitz type 1 and Mobitz type 2 affects how they are treated and what the future holds. Mobitz type 1 is usually seen as less serious, linked to vagal tone or medication. But Mobitz type 2 is linked to heart disease and has a higher risk of becoming complete heart block. So, Mobitz type 2 needs closer watch and possibly more treatment.
Knowing the difference between these types is key to the right treatment and understanding the risks. Accurate diagnosis through an electrocardiogram (ECG) is vital for making the right decisions.
Third-Degree Heart Block: A Critical Condition
Third-degree heart block severely affects the heart’s function. It happens when there’s no connection between the atria and ventricles. This disrupts the heart’s electrical signals, causing severe symptoms.
Complete Dissociation Between Atria and Ventricles
In third-degree heart block, the atria and ventricles beat on their own. This is because electrical signals from the atria can’t reach the ventricles. This leads to an abnormal heart rhythm.
Symptoms of Complete Heart Block:
- Fainting or collapse
- Light-headedness
- Dizziness
- Breathlessness
- Extreme tiredness
- Confusion
- Chest pain
Emergency Management Considerations
Third-degree heart block is a medical emergency. It needs immediate care. The goal is to stabilize the patient and restore a normal heart rhythm.
Emergency management steps may include:
| Management Step | Description |
| Initial Assessment | Quick evaluation of the patient’s condition and symptoms. |
| Pacemaker Implantation | Insertion of a pacemaker to regulate the heart’s rhythm. |
| Medication | Administration of drugs to manage symptoms and stabilize the heart. |
Third-degree heart block can be either born with or develop later in life. It’s important to recognize symptoms and understand emergency care. This helps in treating the condition effectively and improving patient outcomes.
Recognizing Symptoms of Heart Block
Heart block symptoms can vary a lot. Some people might not notice anything, while others might feel very different. These changes can affect their daily life.
Common Symptoms Across All Types
There are some symptoms that are common across all types of heart block. These include:
- Fatigue
- Dizziness or lightheadedness
- Fainting or near-fainting spells
- Shortness of breath
- Chest pain or discomfort
Symptoms Specific to First-Degree Heart Block
First-degree heart block often doesn’t show symptoms. But sometimes, people might feel:
- Mild fatigue
- Occasional dizziness
This type of heart block is often found by chance during an ECG test.
Symptoms Specific to Second-Degree Heart Block
Second-degree heart block can cause more noticeable symptoms. These include:
- Intermittent dizziness or fainting
- Fatigue that worsens with activity
- Shortness of breath during exertion
These symptoms happen because the heart’s electrical signals are blocked. This leads to irregular heartbeats.
Symptoms of Complete Heart Block
Complete or third-degree heart block is a serious condition. It can cause symptoms like:
- Severe fatigue
- Frequent fainting spells
- Shortness of breath even at rest
- Chest pain or palpitations
This condition needs immediate medical help because of the risk of serious problems.
Here’s a quick summary of symptoms for different types of heart block:
| Type of Heart Block | Common Symptoms |
| First-Degree | Mild fatigue, occasional dizziness |
| Second-Degree | Intermittent dizziness, fatigue, shortness of breath |
| Complete (Third-Degree) | Severe fatigue, frequent fainting, shortness of breath, chest pain |
Causes and Risk Factors
Heart block disease can come from many sources. It can be present at birth or develop later. Knowing the causes helps doctors diagnose and treat it better.
Congenital Causes
Some people are born with heart block, known as congenital heart block. This happens when the heart’s electrical system doesn’t form right in the womb. Congenital heart block is often linked to autoimmune disorders in the mother, like lupus, which can harm the fetus’s heart.
Acquired Causes
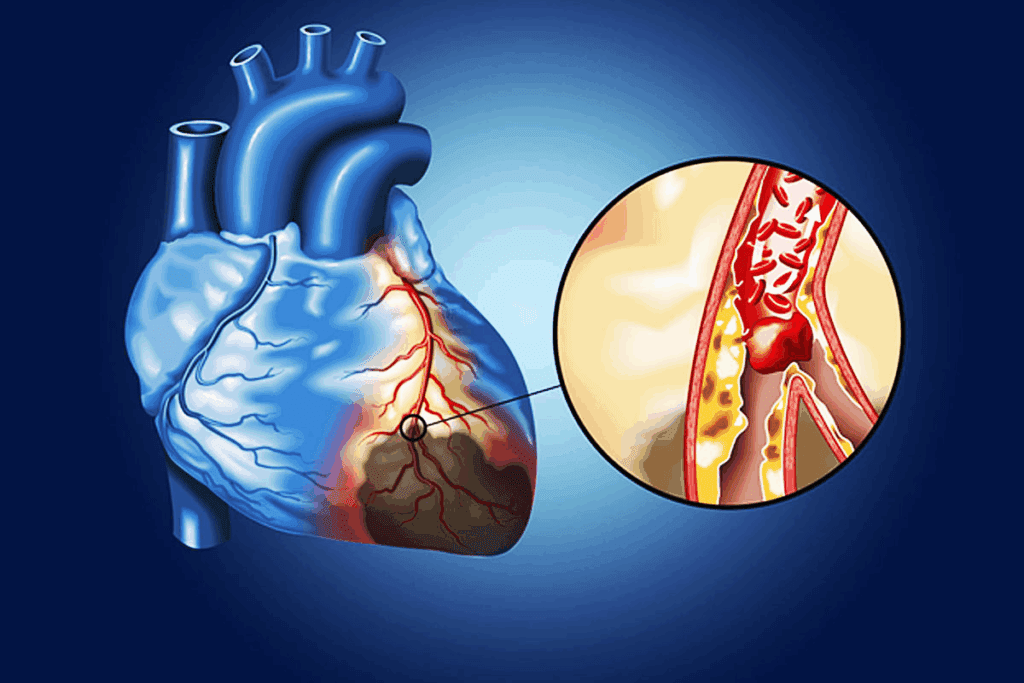
Acquired heart block comes from damage to the heart’s electrical system. This damage can be caused by:
- Coronary artery disease, which can damage the heart’s conduction system during a heart attack.
- Heart failure, where the heart can’t pump blood well, affecting its electrical signals.
- Myocarditis, or inflammation of the heart muscle, which can disrupt electrical signals.
- Cardiac surgery, as complications from surgery can sometimes cause heart block.
- Certain medications, like those for high blood pressure, abnormal heart rhythms, or depression, which can affect the heart’s electrical system.
Also, idiopathic fibrosis of the cardiac conduction system, where tissue around the electrical pathways becomes scarred, can cause acquired heart block.
Risk Factors
Several factors can raise the risk of getting heart block disease. These include:
- Age: The risk goes up with age, more so after 50.
- Family history: A family history of heart conditions can make you more likely to get heart block.
- Pre-existing heart conditions: Conditions like coronary artery disease, heart failure, or previous heart attacks can increase the risk.
- Autoimmune diseases: Diseases like lupus or rheumatoid arthritis can raise the risk of heart block.
Knowing these causes and risk factors is key for early diagnosis and treatment of heart block disease.
Diagnosing Heart Block Disease
Diagnosing heart block disease requires ECG findings, more tests, and a detailed clinical check-up. Getting the diagnosis right is key to choosing the right treatment.
Electrocardiogram (ECG) Findings
The electrocardiogram (ECG) is a key tool in diagnosing heart block disease. It shows the heart’s electrical activity, helping spot any problems in how the heart beats. ECG findings help figure out the type and how bad the heart block is, which guides treatment.
Additional Diagnostic Tests
Though an ECG is essential, more tests might be needed to confirm the diagnosis or learn more about the heart. These tests include:
- Holter monitoring: A 24- to 48-hour ECG recording that helps detect intermittent heart block.
- Event monitoring: A longer-term recording that can be used to capture infrequent symptoms.
- Echocardiogram: An ultrasound test that evaluates heart function and structure.
- Stress test: Assesses the heart’s function under stress, typically through exercise.
Clinical Evaluation
A detailed clinical evaluation is also important in diagnosing heart block disease. This includes a full medical history, physical exam, and symptom check. Clinical evaluation helps understand how the heart block affects the patient’s health and finds any underlying issues.
By using ECG findings, more tests, and clinical evaluation, doctors can accurately diagnose heart block disease. They can then create a treatment plan that meets the patient’s specific needs.
Treatment Approaches for Heart Block
Finding the right treatment for heart block can greatly improve life quality. The type and severity of heart block determine the treatment. We aim to give a detailed look at the available options.
When Treatment Is Necessary
Not every heart block needs immediate treatment. The need for treatment depends on the blockage’s degree and its health impact. For example, first-degree heart block often doesn’t need treatment. But second- and third-degree heart blocks might need more serious actions.
Medication Options
Medications can’t cure heart block but can manage symptoms. They can control heart rate, reduce dizziness or fainting, or treat underlying conditions. This helps manage heart block symptoms.
Pacemaker Implantation
Pacemaker implantation is a key treatment for second- or third-degree heart block. It involves putting a small device in the chest to regulate heartbeat. This is a minor surgery, done while the patient is sedated. A pacemaker ensures the heart beats normally.
Surgical Interventions
Surgical treatments are needed for some heart block cases. This is when the block is caused by a condition that surgery can fix. This could be repairing or replacing damaged heart valves or fixing structural heart defects.
It’s important to know the different treatments for heart block. Tailoring treatment to each person’s needs can greatly improve outcomes and life quality.
Living with Heart Block Disease
Living with heart block disease means making lifestyle changes and keeping an eye on your health. It’s important to know how to manage this condition. This includes many strategies to lessen its effects.
Lifestyle Modifications
Changing your lifestyle can greatly improve life with heart block disease. Eating a heart-healthy diet is key. This means lots of fruits, veggies, whole grains, and lean proteins. Also, regular exercise like walking or swimming is good, but talk to a doctor first.
Stress reduction is also important. Try meditation or deep breathing. Avoid smoking and limit alcohol to prevent complications.
Regular Monitoring and Follow-up
Regular check-ups with your doctor are essential. They help track your condition and adjust treatments as needed. If you have a pacemaker, get it checked often to make sure it’s working right.
Keeping a symptom journal is helpful. It lets you track changes and talk about them with your doctor.
Managing Associated Conditions
Many people with heart block disease also have other health issues. Managing these conditions, like high blood pressure or diabetes, is key. It helps your overall health and reduces heart block’s impact.
Working with your healthcare team to create a comprehensive care plan is important. It can greatly improve your health if you have heart block disease.
When to Seek Emergency Care
Knowing when to go to the emergency room is vital. Severe dizziness, fainting, or chest pain need immediate help. Also, watch for signs of pacemaker problems or other device issues.
Having an emergency plan ready is important. Know the nearest emergency services and have emergency contact numbers handy. This ensures you get the right care quickly.
Conclusion
Understanding heart block disease is key to managing it well. We’ve looked at the different types, like first-degree, second-degree, and third-degree. We’ve also talked about their symptoms and how to treat them.
Heart block disease can really affect someone’s life. But, with the right diagnosis and treatment, many people can live active lives. It’s important to watch for heart warning signs and get help if symptoms don’t go away or get worse.
Early detection of heart block disease is vital. With treatments like medicine, pacemakers, and lifestyle changes, symptoms can be eased. Regular check-ups are also important to keep heart block disease under control.
In short, heart block disease needs careful attention and management. We hope this info helps people understand the condition better. This way, they can take steps to keep their heart healthy.
FAQ
What is heart block disease?
Heart block disease happens when the heart’s electrical signals are delayed or blocked. This disrupts the heart’s normal rhythm.
What are the different types of heart block disease?
There are three main types: first-degree, second-degree, and third-degree heart block. Each has its own characteristics and effects on the heart.
What is the difference between Mobitz type 1 and Mobitz type 2 second-degree heart block?
Mobitz type 1 shows a gradual increase in the PR interval before a beat is missed. Mobitz type 2 has a sudden missed beat without any increase in the PR interval. Mobitz type 2 is more serious.
What are the symptoms of complete heart block?
Symptoms include dizziness, fainting, fatigue, and shortness of breath. These happen because the atria and ventricles beat on their own, leading to poor blood flow.
How is heart block disease diagnosed?
Doctors use an electrocardiogram (ECG) to diagnose heart block disease. They might also do Holter monitoring and clinical tests to check the heart’s electrical activity and function.
What are the treatment options for heart block disease?
Treatment can include medication, pacemaker implantation, or surgery. The choice depends on the type and severity of the heart block.
Can lifestyle modifications help manage heart block disease?
Yes, a healthy diet, regular exercise, and stress management can help manage heart block disease and related conditions.
What are the causes and risk factors of heart block disease?
Heart block disease can be caused by genetics or acquired factors like aging and heart disease. High blood pressure and diabetes are also risk factors.
How can I recognize the symptoms of heart block disease?
Look out for symptoms like dizziness and fatigue. Also, be aware of symptoms specific to each type of heart block.
When should I seek emergency care for heart block disease?
Seek emergency care for severe symptoms like chest pain, severe dizziness, or fainting. These could be signs of a serious complication.
What is a heart blockage?
A heart blockage is when electrical impulses controlling the heartbeat are blocked. It’s different from a blockage in the coronary arteries.
How do you treat a heart block?
Treatment varies by type and severity. It can range from monitoring for mild cases to pacemaker implantation for more severe ones.
What is the etiology of heart block?
Heart block can be caused by genetics or acquired factors. Causes include degenerative changes, ischemic heart disease, and certain medications.
References
- O’Rourke, M. F. (2018). Structure and function of systemic arteries: reflections on the vascular wall and blood flow. Vascular Medicine, 23(4), 316-323. https://pubmed.ncbi.nlm.nih.gov/30016416/





