Last Updated on November 25, 2025 by Ugurkan Demir
At Liv Hospital, we know heart block is complex and serious. It’s also called atrioventricular block. It happens when the heart’s electrical signals are delayed or blocked.Learn about heart block treatment, degrees, symptoms, and the most effective management approaches.
A normal heart rhythm is key for health. A healthy heartbeat is between 60 and 100 beats per minute. But, heart block can slow the heart rate, leading to bradycardia.
Knowing about heart block and its symptoms is important. We’ll look at the degrees of heart block and its treatment options. We’ll also cover the three levels of severity and symptoms like dizziness and fatigue.
Heart block, or atrioventricular block, is when the heart’s electrical signals are delayed or blocked. This makes it hard for the heart to beat right, leading to irregular rhythms or arrhythmias.
To get heart block, we must know how the heart’s electrical system works. The heart’s rhythm starts with electrical impulses from the sinoatrial (SA) node in the right atrium. These impulses then go to the atrioventricular (AV) node and then to the ventricles. This makes the ventricles contract and pump blood.
Atrioventricular block happens when there’s a problem with the electrical pathway between the atria and ventricles. This can occur at different levels, like the AV node or the bundle of His. It can cause electrical signals to be delayed or blocked.
The main issue is with the heart’s electrical system. Normally, the impulse moves smoothly from the atria to the ventricles. But with heart block, this impulse is delayed or blocked, making the heart work poorly.
In a normal heart, the electrical system makes sure the chambers contract together. The impulse from the SA node goes through the AV node to the ventricles, keeping the heartbeat regular.
But with heart block, the signals are delayed or blocked. This can cause irregular heartbeats or arrhythmias. The ventricles might not get the signal to contract on time.
It’s important to know the difference between heart block and heart blockage. Heart blockage is when the coronary arteries are blocked, often by plaque. Heart block, on the other hand, is about the disruption of electrical signals controlling the heartbeat.
| Condition | Description | Causes |
| Heart Block | Disruption in the electrical signals between the heart’s chambers | Problems with the AV node or bundle of His, age-related degeneration |
| Heart Blockage | Blockage in the coronary arteries | Plaque buildup, atherosclerosis |
Knowing the difference between these two conditions is key for the right diagnosis and treatment. Both affect the heart but need different care.
We know of three heart block levels, each affecting the heart differently. It’s key to understand these levels for accurate diagnosis and treatment.
First-degree heart block causes a delay in electrical signals from the atria to the ventricles. This is seen on an electrocardiogram (ECG) as a longer PR interval. Every atrial impulse is conducted to the ventricles, but it’s delayed.
This type of heart block might not show symptoms and is often found by chance during an ECG. It might not need treatment, but it’s wise to keep an eye on it. It could get worse.
Second-degree heart block means some electrical impulses don’t reach the ventricles. It’s split into two types: Mobitz Type I (Wenckebach) and Mobitz Type II.
Third-degree heart block means the atria and ventricles don’t work together. The ventricles beat on their own, with an escape pacemaker.
This can cause symptoms like dizziness, fainting, and shortness of breath. It’s a serious condition that needs quick action, often with a pacemaker.
Knowing the three heart block levels is vital for the right care and treatment. Each level affects patients differently.
It’s important to know the differences between Type 1 and Type 2 heart block. This knowledge helps doctors diagnose and treat patients better. Second-degree heart block is split into Mobitz Type I (Wenckebach) and Mobitz Type II. Both involve missed heart signals, but they have different signs and effects on health.
Mobitz Type I, or Wenckebach, shows a PR interval that gets longer with each beat until a beat is missed. This pattern means the time between heart signals gets longer until a beat is skipped. This type is often seen as less serious and can happen in athletes with high vagal tone.
The ECG for Mobitz Type I shows a PR interval that gets longer and then a missed beat. This pattern is key for doctors to diagnose.
Mobitz Type II has a constant PR interval but with missed beats. Unlike Type I, the PR interval doesn’t get longer before a beat is missed. This type is more serious because it often means a bigger problem with the heart’s electrical system and a higher chance of complete heart block.
The ECG for Mobitz Type II shows a steady PR interval with missed beats. The key sign is a missed beat without a longer PR interval first.
Looking at an ECG is key to telling Mobitz Type I and Type II apart. For Type I, the ECG shows a longer PR interval until a beat is missed. Type II has a steady PR interval and missed beats without a longer interval first.
Knowing these patterns well is vital for the right treatment and predicting how a patient will do. While Type I might be treated with less action, Type II might need more serious steps like a pacemaker because of its higher risk of serious heart problems.
Knowing the signs of heart block is key to getting help fast. The symptoms change based on how bad the blockage is. We’ll look at what each degree of heart block might feel like, from mild to severe.
First-degree heart block usually doesn’t show symptoms. “Many people with first-degree heart block don’t feel anything different,” a heart doctor notes. The heart’s electrical delay is small, so it doesn’t cause noticeable problems. But, some might feel tired or have heart beats that feel off, even if it’s not the heart block’s fault.
Second-degree heart block shows more signs than first-degree. People might feel dizzy or lightheaded if the block is bad. Fatigue is common too, because the heart works less efficiently. Sometimes, it can cause syncope, or fainting, if it gets worse. If you have these symptoms, see a doctor right away.
Complete heart block, or third-degree, is very serious. It can cause severe dizziness, fainting, or even heart failure if not treated quickly. Other signs include shortness of breath, chest pain, and extreme tiredness. Seeing a doctor fast is vital to avoid serious problems. “Quick diagnosis and treatment can greatly help those with complete heart block,” a top cardiologist stresses.
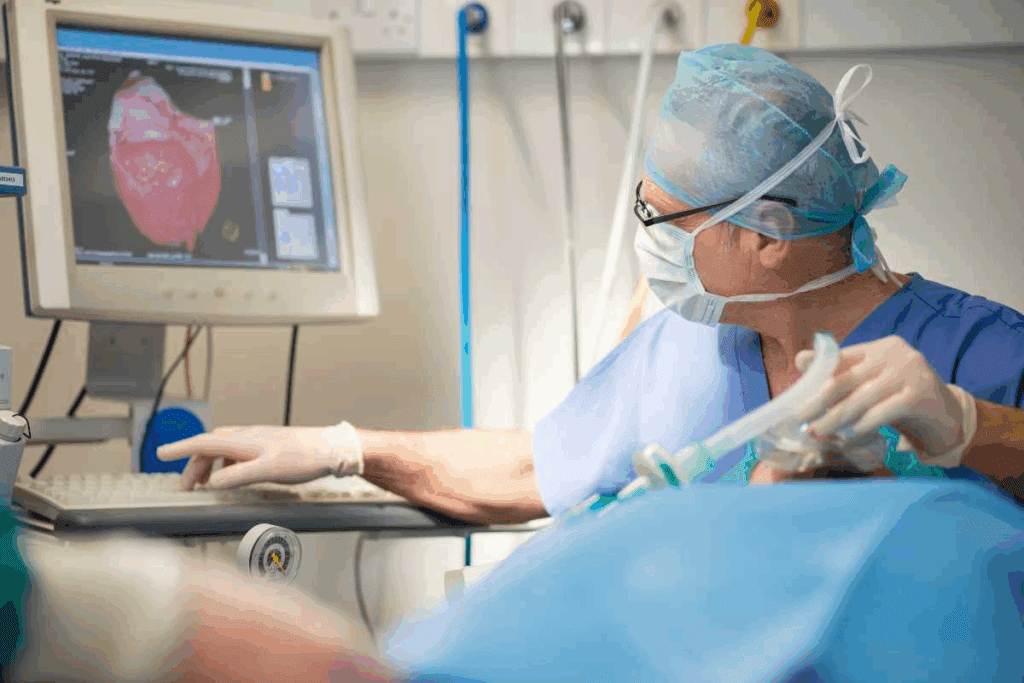
Healthcare experts use many ways to find heart block. They need to check the heart in detail. This helps them know if there’s a block and how bad it is.
The electrocardiogram (ECG) is key for finding heart block. It shows the heart’s electrical signals. This helps see if there are any problems with how the heart beats.
ECG Interpretation: Doctors look at the ECG to spot heart block signs. They check the PR interval and the heart’s rhythm. They also look at the QRS complex.
For people with symptoms that come and go, more tests are needed. Holter monitors and event recorders track the heart for a longer time.
There are more tests to check for heart block. These include:
| Diagnostic Method | Description | Use in Heart Block Detection |
| Electrophysiology Study (EPS) | An invasive test that checks the heart’s electrical signals. | It finds where and how bad the heart block is. |
| Echocardiogram | An ultrasound test that looks at the heart’s structure and function. | It checks how well the heart works and if there are any block causes. |
| Stress Test | A test that watches how the heart acts during exercise. | It sees how the heart handles stress and finds conduction problems. |
By using these tests together, doctors can find heart block and plan the best treatment.
It’s important to know what causes heart block to manage it well. Heart block happens when the heart’s electrical signals get disrupted. This can be due to several factors that harm the heart’s electrical system.
As we get older, our heart’s electrical pathways can wear out. This can cause heart block. Aging naturally speeds up this wear and tear, but other issues like high blood pressure and diabetes can make it worse.
Ischemic heart disease is another big reason for heart block. It happens when the heart muscle doesn’t get enough oxygen. Heart attacks, caused by blocked arteries, can also damage the heart’s electrical system. People with heart disease or who have had heart attacks are more likely to get heart block.
Some medicines can cause heart block. Drugs that control heart rate or the electrical system, like beta-blockers and certain anti-arrhythmics, can lead to heart block. This is more likely in people who are already at risk.
Heart defects at birth and genetic conditions can also cause heart block. Some people are born with heart electrical system problems. Others have genetic conditions that affect the heart’s electrical system, raising their risk of heart block.
Knowing the causes and risk factors of heart block is key to preventing and managing it. Healthcare providers can then tailor treatments to meet each patient’s needs.
The treatment for heart block depends on its degree and type. Knowing how severe and what type it is helps pick the best treatment.
For first-degree heart block, treatment is usually simple. It involves watching the condition closely but not acting right away. This is because it often doesn’t cause symptoms.
Key Considerations:
Type 1 second-degree heart block, or Mobitz Type I, might not need strong treatment. But if symptoms show up or it gets worse, more action might be needed. This could include watching it closely or getting a pacemaker.
Management Strategies:
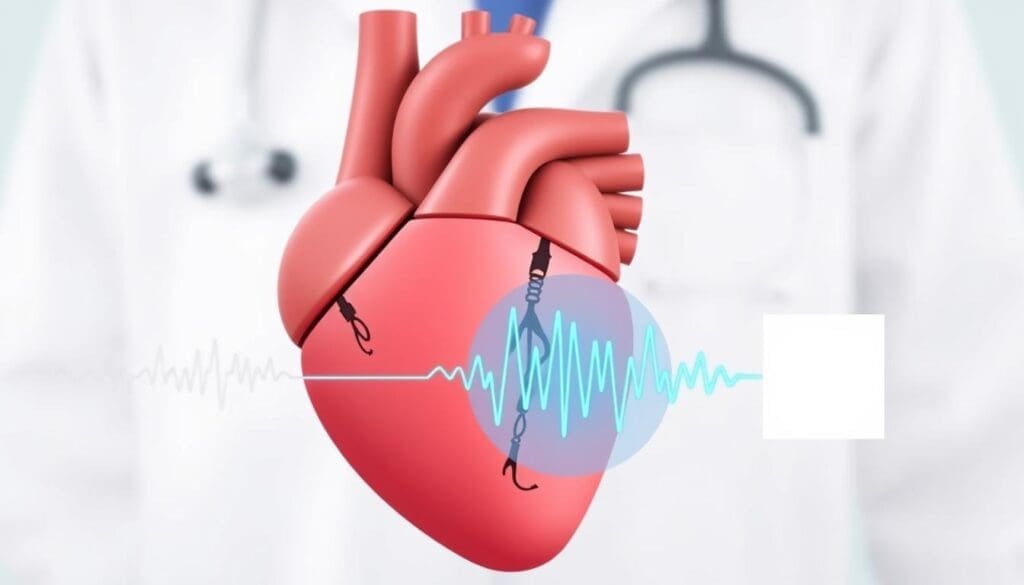
Type 2 second-degree heart block and complete heart block need more serious treatment. This usually means getting a pacemaker. It helps the heart beat right and relieves symptoms.
Treatment Highlights:
| Condition | Primary Treatment | Additional Considerations |
| Type 2 Second-Degree Heart Block | Pacemaker Implantation | Monitoring for possible problems |
| Complete Heart Block | Pacemaker Implantation | Adjusting device settings as needed |
Pacemakers are key in treating serious heart block. They greatly improve life quality for those affected.
Knowing how to treat heart block in emergencies is key to saving lives. Heart block emergencies need quick and effective care to avoid serious problems or death. We’ll cover the essential steps and considerations for emergency heart block management.
Spotting the signs of a heart block emergency is the first step in care. Look out for severe symptoms like syncope, chest pain, or bradycardia. These signs mean you need to get medical help fast to figure out how bad the heart block is and what to do next.
Immediate medical interventions for heart block emergencies might include atropine or a temporary pacemaker to fix the heart rhythm. Atropine can help if the heart rate is too slow. But, it might not work for everyone, and more steps might be needed.
Temporary measures like a transcutaneous pacemaker might be used before a permanent pacemaker is put in. These temporary fixes help keep the patient stable until a lasting solution is found.
In summary, treating heart block emergencies needs quick action and the right medical steps. By knowing the treatment options, doctors can greatly improve patient outcomes in these critical situations.
Getting a pacemaker after heart block changes your life. It’s a small device that keeps your heart beating right. For those with heart block, it’s a lifesaver.
There are many pacemakers, each for different heart needs. Here are the main types:
Getting a pacemaker means making some changes. It’s important for your device to work right and stay safe.
Long-term care for your pacemaker is key. You’ll need regular check-ups to keep an eye on the battery and how it’s working. Modern pacemakers can last 5 to 15 years, depending on the type and how you use it.
Know when to call your doctor. Reach out if you feel dizzy, faint, or have trouble breathing. Also, if you notice any infection signs or changes in your heart rhythm.
Understanding your pacemaker and making lifestyle changes can help you live well. Regular check-ups and care are vital to keep your pacemaker working for your heart.
To prevent heart block, we need to tackle it from many angles. This includes managing heart conditions and living a heart-healthy lifestyle. By controlling risk factors, we can lower our chance of getting heart block.
It’s key to manage heart conditions to avoid heart block. Issues like hypertension and diabetes can harm the heart. By keeping these conditions in check, we can lower heart block risk.
For example, keeping blood pressure normal helps the heart’s electrical system. Also, managing diabetes well can prevent nerve damage that might cause heart block.
Some medicines can mess with heart rhythm and up the risk of heart block. It’s important to talk to a doctor about any medicines you’re taking. Beta-blockers, calcium channel blockers, and some anti-arrhythmic drugs can slow the heart and sometimes cause heart block.
By working with a doctor, we can adjust our meds to lower risks. This might mean changing doses, switching meds, or closely watching heart function.
Living a heart-healthy lifestyle is key to preventing heart block. This means eating a balanced diet full of fruits, veggies, and whole grains. It also means staying active and avoiding smoking and too much alcohol.
Exercise like walking, cycling, or swimming keeps the heart healthy. A good diet supports heart health. And not smoking and drinking in moderation prevent heart damage.
Regular heart check-ups are essential for catching heart problems early. These visits help doctors keep an eye on heart health and spot issues before they get worse.
Doctors might do tests like electrocardiograms (ECGs) during these visits. These tests check heart function and electrical activity. Early treatment can greatly improve outcomes for those at risk of heart block.
Managing heart block means knowing about the condition, its treatments, and making lifestyle changes. Heart block shows up in different ways, each with its own symptoms and treatments. By spotting the signs and understanding how doctors diagnose it, people can handle their condition better.
Living with heart block needs a full plan, including sticking to treatment and eating right. For those with pacemakers, keeping them in good shape is key. It’s also important to manage heart problems, check medicines, and change lifestyle habits to keep the heart healthy.
We’ve covered the main points to help people manage heart block and live better. With the right steps, people can deal with heart block well. This leads to a healthier life and better outcomes.
Heart block is when the heart’s electrical signals get stuck. This can make heartbeats slow down or stop. It can cause mild to severe symptoms.
There are three types of heart block. First-degree means signals are delayed. Second-degree means some signals are blocked. Third-degree means no signals get through, causing a complete block.
Type 1 second-degree heart block makes the PR interval longer until a beat is missed. Type 2 second-degree heart block suddenly stops the impulse from reaching the ventricles without a long PR interval.
Symptoms can range from none in first-degree to dizziness, fatigue, and fainting in second-degree. Third-degree can be life-threatening.
Doctors use electrocardiogram (ECG), Holter monitors, and event recorders to diagnose heart block.
Heart block can be caused by age, heart disease, medication, and genetics.
Treatment varies by severity. First-degree might just need monitoring. Type 2 and complete heart block might need a pacemaker.
Pacemakers help regulate heartbeats in type 2 and complete heart block. They send electrical impulses to the heart.
Preventing heart block means managing risk factors, controlling heart conditions, and making lifestyle changes. Regular check-ups are also important.
Emergency signs include severe dizziness, fainting, and life-threatening symptoms. They need immediate medical attention and may require temporary treatments.
Living with a pacemaker means understanding the device and making lifestyle adjustments. Regular doctor visits are also key.
Heart block is about electrical signal problems. Heart blockage is about blood flow blockages, often due to plaque.
Sometimes, heart block can be managed without a pacemaker. This is true for first-degree and type 1 second-degree heart block.
To manage heart block, eat healthy, exercise, don’t smoke, and manage stress. These steps help prevent heart disease.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!