Heart failure is a big problem after cardiac surgery. It happens in about 20% of cases. It’s very important for patients and their families to know the signs and symptoms.
Medical Expert’s key to understand the challenges after surgery. “Every patient’s recovery is different. Quick action can really help.” At Liv Hospital, we focus on finding problems early and using proven treatments. This helps reduce complications and improves patient results.
Key Takeaways
- Heart failure is a significant complication after cardiac surgery.
- Approximately 20% of cardiac surgery cases experience heart failure.
- Timely intervention is key for better patient outcomes.
- Liv Hospital emphasizes early detection and evidence-based treatment.
- Understanding post-surgery challenges is vital for patients and caregivers.
Understanding Heart Failure After Open Heart Surgery
It’s important to know about heart failure after heart surgery. This condition can really affect a patient’s life and recovery. We’ll look into what heart failure is, how common it is, and how it impacts recovery.
Definition and Pathophysiology
Heart failure means the heart can’t pump enough blood. This can happen after heart surgery for many reasons. These include existing heart problems, the surgery’s complexity, and complications after surgery.
Prevalence Rates
About 20% of heart surgery patients develop heart failure. This shows we need to watch patients closely after surgery. The chance of heart failure depends on the surgery type, patient’s age, and health.
Type of Surgery | Prevalence of Heart Failure |
Coronary Artery Bypass Grafting (CABG) | 15% |
Valve Repair or Replacement | 25% |
Complex Cardiac Reconstructions | 30% |
Impact on Recovery and Quality of Life
Heart failure after surgery can really slow down recovery and lower quality of life. Patients might not be able to exercise as much, feel tired all the time, and have trouble doing daily tasks. It’s key to manage this condition well to help patients get better.
Understanding heart failure after surgery helps us support patients better. This way, we can improve their health and quality of life in the long run.
Risk Factors for Developing Post-Operative Heart Failure

Knowing the risk factors for heart failure after surgery is key to better patient care. It helps healthcare providers manage and lower the risk of heart failure after open heart surgery.
Pre-existing Cardiac Conditions
Heart conditions before surgery greatly affect the risk of heart failure afterward. Hypertension, coronary artery disease, and previous heart attacks can make it hard for the heart to bounce back from surgery.
Those with a history of heart failure or weak heart function are at higher risk. It’s important to manage these conditions before, during, and after surgery to reduce heart failure risk.
Age and Comorbidities
Age is a big factor in heart failure risk after surgery. Older patients face a higher risk because of less physical strength and more health problems like diabetes, kidney disease, and COPD.
Having many health problems can make surgery and recovery harder, raising heart failure risk. We need to think about these issues when deciding if someone should have surgery and how to handle them well.
Comorbidity | Impact on Heart Failure Risk |
Diabetes | Increases risk due to possible heart damage and makes recovery harder. |
Chronic Kidney Disease | Can make it tough to manage fluids and electrolytes, stressing the heart more. |
COPD | Can harm breathing, putting more strain on the heart. |
Surgical Factors and Complications
The type of surgery and any problems during or after it can also raise heart failure risk. Long cardiopulmonary bypass times, a lot of blood loss, and infections are examples.
Using careful surgical methods and good post-operative care can help lower these risks. By tackling these issues, we can cut down heart failure chances and better patient results.
Types of Open Heart Procedures and Their Heart Failure Risks
The risk of heart failure after open heart surgery depends on the procedure type. Open heart surgery treats various heart conditions. Knowing the risks helps manage expectations and improve outcomes.
Coronary Artery Bypass Grafting (CABG)
Coronary Artery Bypass Grafting, or CABG, is a common surgery. It uses a healthy blood vessel to bypass blocked arteries. This improves blood flow to the heart. CABG is effective but can lead to heart failure, mainly in those with pre-existing heart issues.
Heart failure after CABG can be due to several reasons. These include the patient’s heart function before surgery, the extent of artery disease, and complications like heart attacks. Managing these factors is key to reducing heart failure risk after CABG.
Valve Repair or Replacement Surgery
Valve repair or replacement is another common surgery. It fixes or replaces heart valves. The choice depends on the valve’s condition. Valve surgery improves heart function but also risks heart failure, mainly in severe cases.
Heart failure after valve surgery can stem from valve issues, complications, or worsening heart disease. Choosing the right patient, using the right technique, and post-operative care can reduce these risks.
Complex Cardiac Reconstructions
Complex cardiac reconstructions are for severe heart issues. These include repairs for congenital defects, tumor removals, and complex artery repairs. These surgeries are lifesaving but riskier due to their complexity.
Patients need thorough evaluation, skilled surgery, and detailed care after these surgeries. Advanced monitoring and support are used to manage these risks.
Sign #1: Shortness of Breath After Cardiac Surgery
After cardiac surgery, patients might notice changes in breathing. This can be a sign of heart failure. Shortness of breath, or dyspnea, is a common symptom after open heart surgery. It’s important to recognize these signs early for timely treatment.
Normal vs. Abnormal Breathing Patterns
It’s key to know the difference between normal and abnormal breathing after surgery. Some shortness of breath is okay during recovery. But, if it’s persistent or severe, it could mean a problem.
We should watch our breathing closely. If we notice anything off, we should tell our doctor.
The main differences are:
- Rate: Faster than normal breathing rate
- Depth: Shallower or labored breathing
- Effort: Increased effort to breathe, potentially accompanied by wheezing or coughing
Exertional Dyspnea vs. Rest Dyspnea
Dyspnea can happen during activity (exertional dyspnea) or at rest (rest dyspnea). Exertional dyspnea is common as the body recovers. But, rest dyspnea is more serious and needs quick medical attention.
Types of dyspnea and their implications:
- Exertional dyspnea: May indicate a need for adjustments in activity levels or rehabilitation strategies
- Rest dyspnea: May signify a more severe cardiac issue requiring immediate medical attention
Orthopnea and Paroxysmal Nocturnal Dyspnea
Orthopnea and paroxysmal nocturnal dyspnea (PND) are specific types of dyspnea. Orthopnea is shortness of breath when lying down, relieved by sitting up. PND is sudden, severe shortness of breath that wakes you up at night, usually goes away when sitting up or standing.
Both orthopnea and PND are serious signs that need quick doctor’s attention. They can mean heart failure or other serious heart problems.
Sign #2: Fluid Retention and Edema
Fluid retention is a key sign of heart failure after surgery. It shows up as swelling in different parts of the body. This swelling can be a sign of serious problems. We will look at how fluid retention and swelling can appear, like in the legs, belly, and lungs.
Peripheral Edema in Extremities
Peripheral edema is when your feet, ankles, legs, and arms swell up. This happens because your heart isn’t pumping well. It’s a sign that your heart might not be working right. If you notice swelling, tell your doctor right away.
Abdominal Swelling and Weight Gain
Fluid retention can also cause your belly to swell up. This is called ascites, and it can make you gain weight quickly. It means your body is holding onto too much fluid. Weighing yourself every day can help catch this early.
Pulmonary Edema Symptoms
Pulmonary edema is when fluid builds up in your lungs. It makes it hard to breathe, and you might cough up pink mucus. It’s a serious problem that needs quick help from a doctor.
Symptom | Description | Severity |
Peripheral Edema | Swelling in feet, ankles, legs, and arms | Mild to Moderate |
Abdominal Swelling | Fluid accumulation in the abdomen | Moderate |
Pulmonary Edema | Fluid in the lungs, shortness of breath | Severe |
It’s important to know the signs of fluid retention and swelling after heart surgery. Catching these problems early can help you get better faster and avoid serious issues.
Sign #3: Unusual Fatigue and Weakness
Feeling unusually tired and weak after open heart surgery is a sign that needs attention. Some tiredness is normal after surgery. But, if it lasts a long time, it could mean your heart is not working right.
Distinguishing Normal Recovery Fatigue from Heart Failure
It’s important to tell the difference between normal tiredness after surgery and heart failure. Normal tiredness gets better with rest and more activity. But, heart failure makes you very tired all the time and affects your daily life.
Key differences include:
- Duration: Heart failure fatigue doesn’t get better with rest.
- Severity: It’s much worse than normal tiredness after surgery.
- Impact: It really affects your daily life and how well you feel.
Decreased Exercise Tolerance
Being able to do less exercise is another sign of heart failure after surgery. Activities that were easy before now make you out of breath or very tired.
Signs of decreased exercise tolerance include:
- Needing to stop and rest during activities due to fatigue or shortness of breath.
- Feeling unusually tired after performing tasks that were previously manageable.
- Experiencing a significant reduction in the ability to engage in physical activities.
Impact on Daily Activities
Unusual fatigue and weakness can really affect your daily life. Even simple tasks like bathing or cooking can be hard. This can make you feel less independent and affect your quality of life.
“The fatigue was overwhelming. Even simple tasks like making breakfast felt like a marathon. It was a struggle to maintain my independence.” – A patient recovering from open heart surgery.
Understanding and addressing these symptoms early can help manage heart failure and improve recovery outcomes.
Sign #4: Irregular Heartbeat and Palpitations
Irregular heartbeats and palpitations are key signs of heart failure after open heart surgery. These symptoms can be scary and show that the heart’s rhythm might be off.
Common Arrhythmias Associated with Heart Failure
After open heart surgery, patients might get different arrhythmias. Atrial fibrillation is common, causing a fast and irregular heartbeat. Other arrhythmias like ventricular tachycardia and bradycardia can also affect the heart’s function.
A study in the Journal of the American College of Cardiology found arrhythmias are a big problem after cardiac surgery. They can make patients’ stays in the hospital longer and affect their health.
Arrhythmia Type | Characteristics | Potential Impact |
Atrial Fibrillation | Rapid, irregular heartbeat | Increased risk of stroke, heart failure |
Ventricular Tachycardia | Fast heart rate originating in ventricles | Can lead to ventricular fibrillation, cardiac arrest |
Bradycardia | Slow heart rate | Reduced cardiac output, fatigue, dizziness |
Symptoms of Concerning Heart Rhythm Changes
It’s important for patients to know about symptoms of heart rhythm changes. These include:
- Palpitations or a feeling of skipped beats
- Dizziness or lightheadedness
- Shortness of breath
- Chest pain or discomfort
- Fainting or near-fainting spells
Early detection and management of arrhythmias are key to avoiding bad outcomes in post-cardiac surgery patients.
“The management of arrhythmias post-cardiac surgery requires a complete approach. This includes medication, lifestyle changes, and sometimes invasive procedures.”
When to Seek Emergency Care
If you have severe chest pain, trouble breathing, dizziness, or a fast or irregular heartbeat, get help right away.
While some irregular heartbeats are not serious, others can be deadly. It’s vital to get checked by a doctor to find out what’s wrong and how to fix it.
Sign #5: Persistent Cough or Wheezing
A persistent cough or wheezing after open heart surgery might mean heart failure. This is because it could point to fluid in the lungs, a heart failure complication.
A cardiac cough is different from a regular cough. It doesn’t go away and gets worse when you lie down. Knowing this cough is key to catching heart failure early.
Characteristics of Cardiac Cough
A cardiac cough is dry or brings up frothy, sometimes pink-tinged sputum. This pink color means there’s blood. It’s a sign of fluid in the lungs because the heart can’t pump well.
Pink-tinged sputum is a big warning. It means there’s a lot of fluid and possibly bleeding in the lungs. You need to see a doctor right away.
Pink-Tinged Sputum Warning Signs
Seeing pink-tinged sputum means watch for other signs too. Look for harder breathing, feeling very tired, and swelling in your legs. These signs together could mean heart failure is getting worse.
Symptom | Description | Action Required |
Cardiac Cough | Persistent, dry, or frothy sputum | Monitor and report to healthcare provider |
Pink-Tinged Sputum | Presence of blood in sputum | Seek immediate medical attention |
Nighttime Coughing | Coughing that worsens when lying down | Adjust sleeping position, consult healthcare provider |
Nighttime Coughing Patterns
Coughing that gets worse at night could be heart failure. It happens because fluid moves around more when you lie down. Raising your bed can help.
If you keep coughing or wheezing, see your doctor. Catching heart failure early can make a big difference.
Diagnostic Approaches for Heart Failure After Open Heart Surgery
Diagnosing heart failure after surgery is key for good care. It involves clinical checks, lab tests, and imaging. These steps help find and treat heart failure.
Physical Examination Findings
A detailed physical check is the first step. Doctors look for signs like peripheral edema, jugular venous distension, and pulmonary congestion. These signs show fluid buildup and heart problems.
For example, a patient might have orthopnea, or trouble breathing when lying down. This is a big sign of heart trouble.
Laboratory Tests and Biomarkers
Labs are very important for diagnosing heart failure. Key tests include:
- B-type natriuretic peptide (BNP) or N-terminal pro b-type natriuretic peptide (NT-proBNP) levels
- Complete blood count (CBC) to check for anemia or infection
- Serum electrolytes to check for imbalances
- Renal function tests to see how the kidneys are doing
BNP and NT-proBNP are great because they go up in heart failure. They help doctors know if someone has heart failure.
Laboratory Test | Significance in Heart Failure Diagnosis |
BNP/NT-proBNP | Elevated levels indicate heart failure |
CBC | Helps rule out anemia or infection |
Serum Electrolytes | Assesses for electrolyte imbalances |
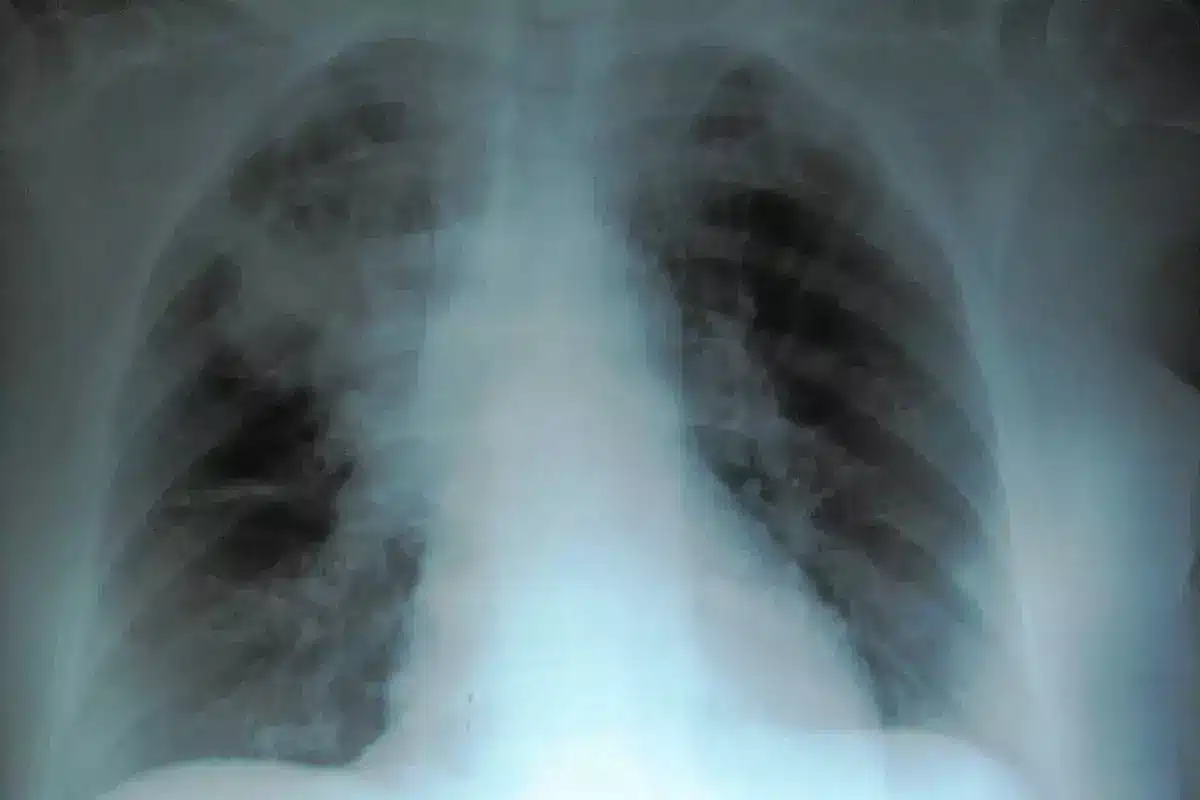
Imaging Studies and Cardiac Function Assessment
Imaging studies are key for checking the heart’s function and shape. Common ones are:
- Echocardiography to check ventricular function and valve health
- Chest X-ray to see if there’s lung congestion
- Cardiac MRI or CT scans for detailed heart anatomy
These studies help doctors find out why someone has heart failure. They also help decide the best treatment.
“The diagnosis of heart failure after open heart surgery requires a complete and team-based approach. It includes clinical findings, lab results, and imaging studies.”— Expert in Cardiology
By using all these methods, doctors can accurately find and treat heart failure. This improves patients’ lives and outcomes.
Treatment Strategies and Management Options
After open heart surgery, treatment for heart failure includes medicine, lifestyle changes, and new therapies. We know that the right treatment can greatly improve heart failure results. This can make patients’ lives better.
Medication Protocols
Medicine is key in managing heart failure after surgery. We give a mix of medicines to ease symptoms and slow the disease.
- ACE Inhibitors: These relax blood vessels, easing the heart’s work.
- Beta-Blockers: Beta-blockers slow the heart rate, making it work better.
- Diuretics: Diuretics remove extra fluid, reducing swelling and breathlessness.
It’s important to take the medicine as directed and watch for side effects. We work with patients to adjust the medicine as needed for the best results.
Lifestyle Modifications
Changing your lifestyle is also vital in managing heart failure. We suggest the following to help your heart:
- Dietary Changes: Eat less salt and more fruits, veggies, and whole grains.
- Exercise: Regular, gentle exercise boosts heart health.
- Smoking Cessation: Quitting smoking lowers heart stress.
- Weight Management: Keep a healthy weight to ease heart strain.
These lifestyle changes help your heart and overall health.
Advanced Therapies for Refractory Cases
For severe heart failure, advanced treatments might be needed. We look at options like:
- Cardiac Resynchronization Therapy (CRT): Helps the heart’s chambers beat together.
- Implantable Cardioverter-Defibrillators (ICDs): Watches heart rhythm and shocks for dangerous arrhythmias.
- Left Ventricular Assist Devices (LVADs): Mechanical pumps help the heart pump.
- Heart Transplantation: In extreme cases, a new heart might be needed.
These advanced treatments are chosen based on each patient’s needs. They offer hope and better outcomes for those with severe heart failure.
Conclusion: Long-Term Prognosis and Preventive Measures
Understanding the long-term outlook for heart failure after open heart surgery is key. It helps manage patient hopes and improve results. Heart failure can greatly affect recovery and life quality. So, finding ways to prevent it is very important.
Preventive steps, like eating well and exercising often, are critical in lowering heart failure risk. By choosing healthy habits, patients can boost their heart health. This improves their long-term outlook.
Managing heart failure well means regular check-ups and sticking to medication plans. We stress the need for ongoing care to get the best results. By focusing on heart health, patients can lower the chance of problems. This helps them live better lives.
FAQ
What are the signs of heart failure after open heart surgery?
Signs include shortness of breath and fluid buildup. You might also feel unusually tired or weak. Other signs are an irregular heartbeat and a persistent cough.
How common is heart failure after open heart surgery?
Heart failure happens in about 20% of cardiac surgery cases. It can greatly affect recovery and quality of life.
What are the risk factors for developing heart failure after open heart surgery?
Risk factors include heart problems before surgery, age, and other health issues. The type of surgery and any complications also play a role.
What types of open heart procedures are associated with a higher risk of heart failure?
CABG, valve repair or replacement, and complex reconstructions are riskier. Each procedure has its own risk level.
How is heart failure diagnosed after open heart surgery?
Doctors use physical exams, lab tests, and biomarkers. They also do imaging studies to check the heart’s function.
What are the treatment strategies for managing heart failure after open heart surgery?
Treatment includes medicines and lifestyle changes. This includes diet and exercise. Advanced therapies are used for severe cases, tailored to each patient.
Can heart failure after open heart surgery be prevented?
Some risks can’t be changed, but preventive steps are possible. Managing heart conditions, optimizing health, and following post-op care can help.
What is the long-term prognosis for patients with heart failure after open heart surgery?
Prognosis depends on heart failure severity, treatment response, and other health issues. Ongoing management and follow-up care are key.
How does congestive heart failure after CABG affect patient outcomes?
It can greatly impact recovery, quality of life, and survival. Close monitoring and management are essential.
What are the symptoms of heart failure after bypass surgery?
Symptoms include shortness of breath, fatigue, swelling, irregular heartbeats, and a persistent cough. These need immediate medical attention.
Is surgery for congestive heart failure a viable treatment option?
Surgery might be an option for some cases of congestive heart failure. This includes heart transplantation or assist device implantation, based on the cause and severity.