Polycystic ovary syndrome (PCOS) is a hormonal disorder that affects many women worldwide. It disrupts menstrual health and overall well-being. PCOS is a complex condition that affects menstrual cycles and more. This is the ultimate guide to heavy menstrual bleeding PCOS. Learn the critical, surprising reasons why it happens and how to get powerful relief.
PCOS is a leading cause of female infertility, affecting 6% to 12% of women in the U.S. Women with PCOS often face painful periods and irregular menstrual cycles. These symptoms can greatly affect daily life.
Understanding the link between PCOS and menstrual health is key for managing the condition. By learning how PCOS causes these symptoms, we can help women better manage their condition.
Key Takeaways
- PCOS is a hormonal disorder affecting 6-12% of women of reproductive age in the U.S.
- Women with PCOS often experience painful periods and irregular menstrual cycles.
- Understanding PCOS and its symptoms is key for effective management.
- PCOS is a complex condition affecting not only menstrual health but also overall well-being.
- Effective management of PCOS requires a complete approach.
Understanding PCOS: A Common Hormonal Disorder

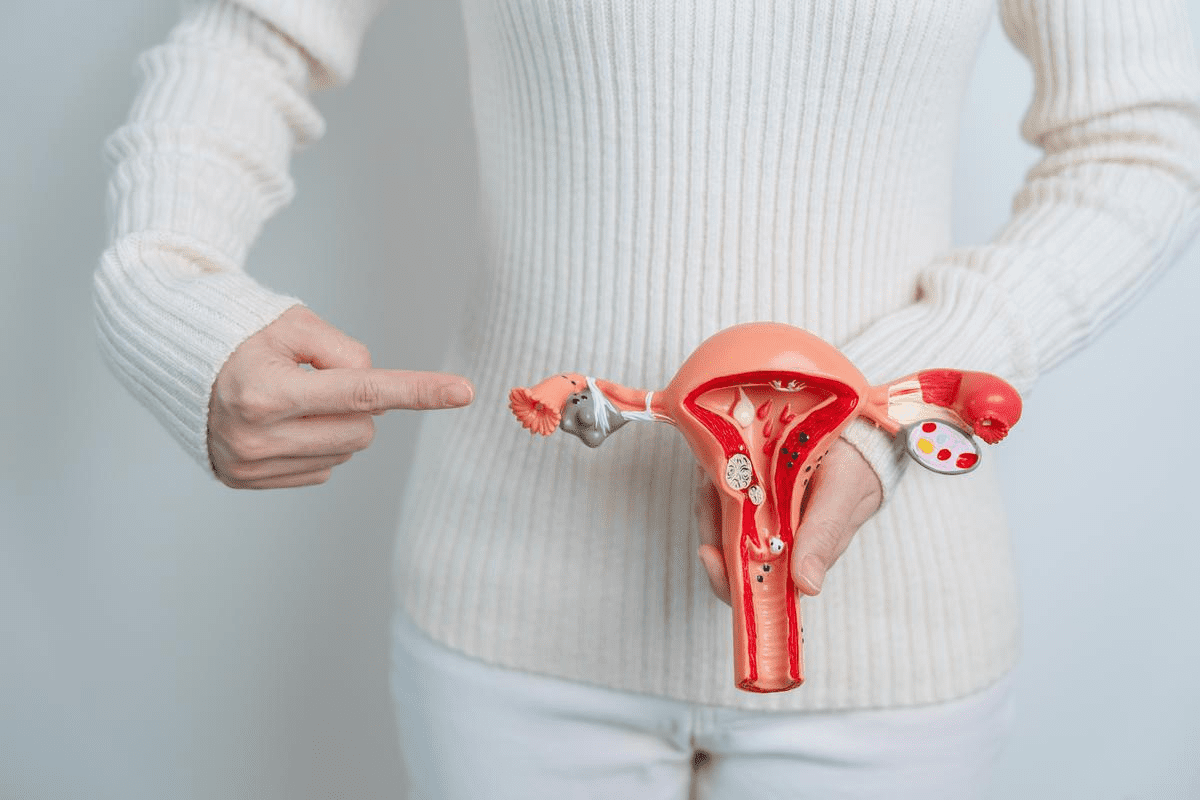
PCOS, or Polycystic Ovary Syndrome, is a hormonal disorder that affects women of reproductive age. It impacts their menstrual cycles and overall health. Knowing about PCOS is key to understanding its effects.
What is Polycystic Ovary Syndrome?
PCOS is a hormonal disorder with symptoms like irregular periods and acne. It also causes unwanted hair growth and hair loss. Insulin resistance is often linked to PCOS, raising the risk of type 2 diabetes.
A study found that about 79.4 percent of women with PCOS have irregular periods. This shows how common menstrual issues are in this group.
“The diagnosis of PCOS is often a complex process, involving a combination of clinical evaluation, medical history, and diagnostic tests to rule out other possible causes of symptoms.”
Prevalence and Demographics
PCOS is a common endocrine disorder, affecting 8-13% of women worldwide. It can affect any woman of reproductive age. But, it’s more common in younger women.
Age Group | Prevalence of PCOS |
15-24 years | Higher incidence due to hormonal fluctuations |
25-34 years | Commonly diagnosed due to fertility issues |
35-44 years | Symptoms may persist, with increased metabolic risks |
Key Hormonal Imbalances in PCOS
PCOS is marked by high levels of male hormones and insulin resistance. These imbalances cause symptoms like hirsutism and acne. They also affect ovulation, leading to irregular periods and fertility issues.
Understanding these hormonal imbalances is key to managing PCOS. Treatment aims to regulate hormones and improve insulin sensitivity. This helps reduce symptoms and long-term health risks.
How PCOS Affects the Menstrual Cycle
Understanding how PCOS affects the menstrual cycle is key to managing symptoms. PCOS, or Polycystic Ovary Syndrome, is a hormonal disorder that impacts women of reproductive age. It causes a variety of menstrual irregularities.
The menstrual cycle is regulated by hormones. But in women with PCOS, this balance is disrupted. This leads to irregularities. We will explore the differences between a normal menstrual cycle and one affected by PCOS.
Normal Menstrual Cycle vs. PCOS-Affected Cycle
A normal menstrual cycle lasts from 21 to 35 days. Ovulation happens around the midpoint. Women with PCOS often have longer or irregular cycles, sometimes without ovulation.
The hormonal imbalance in PCOS, with high androgens and insulin resistance, causes these irregularities. This can lead to oligomenorrhea, or infrequent periods, where cycles may be more than 35 days apart.
Common Menstrual Irregularities in PCOS
Menstrual irregularities are a hallmark of PCOS. These can include:
- Infrequent periods (oligomenorrhea)
- Prolonged or heavy menstrual bleeding (menorrhagia)
- Irregular spotting
Such irregularities can be distressing and impact a woman’s quality of life. The prevalence of menorrhagia in women with PCOS ranges from 10 to 30 percent. This highlights the need for effective management strategies.
Oligomenorrhea: When Periods Become Infrequent
Oligomenorrhea is a common issue in PCOS, where menstrual cycles become irregular and infrequent. This condition can lead to difficulties in conceiving. It also increases the risk of endometrial hyperplasia due to unopposed estrogen exposure.
Menstrual Cycle Characteristic | Normal Cycle | PCOS-Affected Cycle |
Cycle Length | 21-35 days | Variable, often >35 days |
Ovulation | Regular ovulation | Often anovulatory |
Bleeding Pattern | Regular, moderate flow | Irregular, may be heavy or light |
Understanding these differences is key to managing PCOS symptoms effectively. By recognizing the signs of menstrual irregularities, women with PCOS can seek appropriate medical care. This can help regulate their cycles and improve their overall health.
Heavy Menstrual Bleeding PCOS: Causes and Mechanisms
Women with PCOS often face heavy menstrual bleeding, known as menorrhagia. This can be very distressing and debilitating. It’s closely tied to the hormonal imbalances found in PCOS.
Defining Menorrhagia in PCOS Patients
Menorrhagia means having very heavy or long menstrual periods. For women with PCOS, this is a big problem. It’s linked to other hormonal and metabolic issues. Heavy menstrual bleeding can cause serious health problems, like anemia and lower quality of life.
“Heavy menstrual bleeding is a big challenge for women with PCOS,” says a leading expert. “It affects their physical and emotional health.”
Prevalence Rates Among Women with PCOS
Research shows women with PCOS are more likely to have menorrhagia. The rate of heavy menstrual bleeding in PCOS patients varies. But it’s seen as a common symptom.
- Menstrual irregularities are common in PCOS.
- Hormonal imbalances play a significant role in heavy bleeding.
- Menorrhagia can lead to additional health complications.
Hormonal Imbalances Leading to Excessive Bleeding
The hormonal imbalances in PCOS, like high estrogen and androgens, can mess up menstrual cycles. This leads to heavy or irregular bleeding. Hormonal contraceptives are often used to help manage these symptoms.
Understanding the causes of heavy menstrual bleeding in PCOS helps doctors find better treatments. These might include hormonal therapies and other interventions to reduce bleeding and improve health.
PCOS and Painful Periods: Understanding the Connection
Women with Polycystic Ovary Syndrome (PCOS) often face severe menstrual cramps and pelvic pain. This can really impact their daily life. It’s important to understand how PCOS and painful periods are connected to manage the condition better.
Why PCOS Can Intensify Menstrual Cramps
PCOS can make menstrual cramps worse due to hormonal imbalances and inflammation. Women with PCOS might have higher androgens and insulin resistance. These factors can lead to more severe cramps.
Hormonal Imbalance and Menstrual Cramps
- Higher levels of prostaglandins, hormone-like substances that cause the uterus to contract, are associated with more severe menstrual cramps.
- Increased androgen levels can exacerbate inflammation, contributing to pain.
- Insulin resistance, common in PCOS, can lead to increased inflammation and pain.
Inflammatory Processes in PCOS-Related Pain
Inflammation is a big part of the pain women with PCOS experience. Chronic low-grade inflammation is a key feature of PCOS. It can cause more severe menstrual cramps and pelvic pain.
The Role of Inflammation
- C-reactive protein (CRP) levels are often elevated in women with PCOS, indicating chronic inflammation.
- Inflammatory cytokines can disrupt normal ovarian function, leading to irregular periods and pain.
- Anti-inflammatory treatments may help alleviate some of the pain associated with PCOS.
Distinguishing PCOS Pain from Other Causes
It’s important to tell the difference between PCOS pain and other causes. While PCOS is linked to menstrual cramps and pelvic pain, other conditions like endometriosis and ovarian cysts can also cause similar symptoms.
Condition | Common Symptoms | Distinguishing Features |
PCOS | Irregular periods, hirsutism, acne, pelvic pain | Hormonal imbalance, insulin resistance, polycystic ovaries on ultrasound |
Endometriosis | Pelvic pain, heavy bleeding, infertility | Presence of endometrial tissue outside the uterus, often diagnosed via laparoscopy |
Ovarian Cysts | Pelvic pain, bloating, irregular periods | Presence of cysts on the ovaries, often detected by ultrasound |
Understanding the link between PCOS and painful periods is key to managing it. By knowing what causes pain and distinguishing PCOS pain from others, healthcare providers can create better treatment plans. This can greatly improve the lives of women with PCOS.
Endometrial Changes in PCOS
Women with Polycystic Ovary Syndrome (PCOS) often see big changes in their uterus lining. These changes can cause irregular periods and health issues.
Endometrial Thickening and Irregular Shedding
In PCOS, the uterus lining gets thicker because of unopposed estrogen exposure. This leads to irregular shedding. As a result, menstrual bleeding becomes heavier and less predictable. Without enough progesterone, the lining sheds irregularly, causing menstrual flow variations.
Risk of Endometrial Hyperplasia
The risk of endometrial hyperplasia is high in PCOS. If not treated, it can cause serious health problems, including endometrial cancer. It’s vital to watch it closely and manage it well to avoid these risks.
Long-term Endometrial Health Concerns
PCOS can lead to serious long-term health issues, like endometrial cancer. If left untreated, endometrial hyperplasia can turn into cancer. Regular check-ups and screenings are key to keeping an eye on endometrial health and catching any problems early.
Diagnosing PCOS-Related Menstrual Problems
Getting a correct diagnosis is key to handling PCOS-related menstrual issues well. We know diagnosing PCOS means looking at symptoms, medical history, physical checks, and tests.
When to Consult a Healthcare Provider
If you have irregular periods, heavy bleeding, or constant pelvic pain, see a doctor. Look for these signs:
- Irregular or infrequent periods
- Excessive hair growth or acne
- Unusual or heavy bleeding
- Pelvic pain or cramping
Essential Diagnostic Tests and Procedures
Doctors may run several tests to find the cause of PCOS-related menstrual issues. These include:
Diagnostic Test | Purpose |
Pelvic Ultrasound | To check the ovaries for cysts or issues |
Blood Tests | To measure hormone levels, like androgens and insulin |
Endometrial Biopsy | To look at the uterus lining for any changes |
Differential Diagnosis: Other Causes of Abnormal Bleeding
It’s important to check for other reasons of abnormal bleeding, like uterine fibroids or thyroid issues. We help find the real cause of symptoms and plan the best treatment.
Understanding PCOS and its menstrual issues helps us give accurate diagnoses. This way, we can manage PCOS effectively for women.
Medical Treatments for Heavy Bleeding and Pain in PCOS
PCOS can cause heavy bleeding and pain. These symptoms can make life hard. But, there are treatments that can help.
Hormonal Therapy Options
Hormonal therapies are a common treatment for PCOS. They can make menstrual cycles regular, reduce bleeding, and ease pain.
- Birth Control Pills: These pills help control menstrual cycles and lessen bleeding.
- Progesterone Therapy: It balances hormones and lowers the risk of certain conditions.
These treatments can really help with PCOS symptoms. But, it’s important to talk to a doctor about the good and bad sides.
Non-Hormonal Medications for Symptom Relief
There are also non-hormonal meds for PCOS symptoms.
Medication | Use | Benefits |
Tranexamic Acid | Reduces heavy menstrual bleeding | Helps cut down on blood loss |
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) | Relieves menstrual pain and cramps | Lessens inflammation and pain |
These meds can be used alone or with hormonal treatments. They help manage PCOS symptoms well.
Surgical Interventions When Conservative Treatments Fail
Sometimes, surgery is needed when other treatments don’t work.
- Endometrial Ablation: This procedure removes the uterine lining to stop heavy bleeding.
- Hysterectomy: Removing the uterus is considered when all else fails.
These surgeries are usually for women who have finished having children and haven’t found relief with other treatments.
Lifestyle Management Strategies for PCOS Symptoms
Making lifestyle changes is key to easing PCOS symptoms. Women with PCOS can manage their condition and feel better by making smart choices.
Dietary Approaches to Regulate Hormones
Eating a balanced diet is vital for hormone regulation and PCOS symptom management. Foods like salmon and walnuts, rich in omega-3 fatty acids, can reduce inflammation. Foods high in fiber, such as fruits, vegetables, and whole grains, also improve insulin sensitivity.
A sample meal plan could be:
- Oatmeal with berries and almonds for breakfast
- Grilled chicken salad with mixed greens and whole grain crackers for lunch
- Quinoa and vegetable stir-fry with lean beef for dinner
Exercise Benefits for PCOS Management
Regular exercise is essential for PCOS symptom management. Exercise boosts insulin sensitivity, lowers androgen levels, and aids in weight loss. Good options include brisk walking, cycling, and swimming.
Exercise Type | Benefits | Frequency |
Aerobic Exercise | Improves insulin sensitivity, reduces androgen levels | At least 150 minutes per week |
Resistance Training | Enhances muscle mass, improves metabolic rate | 2-3 times per week |
Stress Reduction and Sleep Optimization
Stress can worsen PCOS symptoms, making stress management critical. Yoga, meditation, and deep breathing can help. Getting enough sleep is also key, as poor sleep can upset hormone balances.
Supplements and Complementary Therapies
Supplements like omega-3 fatty acids, vitamin D, and probiotics may help with PCOS symptoms. But, always talk to a healthcare provider before starting any supplements.
By adopting these lifestyle strategies, women with PCOS can manage their symptoms better and enhance their quality of life.
Conclusion: Taking Control of PCOS and Menstrual Health
Women can understand and manage PCOS and its impact on menstrual health. This knowledge helps improve their quality of life. Effective management includes both medical treatments and lifestyle changes.
PCOS can cause heavy bleeding and painful periods. Hormonal therapy and non-hormonal medications can help. Also, making healthy lifestyle choices is important.
Managing PCOS and menstrual health requires a full approach. Women can reduce symptoms by using medical treatments and making lifestyle changes. We suggest talking to healthcare providers to create a personal plan for better health.
FAQ
Does PCOS cause heavy menstrual bleeding?
Yes, PCOS can lead to heavy menstrual bleeding, or menorrhagia. This happens because of hormonal imbalances, like too much estrogen. This imbalance causes the lining of the uterus to thicken, leading to too much bleeding.
Can PCOS cause painful periods?
Yes, women with PCOS often have painful periods, or dysmenorrhea. This pain is due to inflammation and changes in hormones. These changes make menstrual cramps worse.
How does PCOS affect the menstrual cycle?
PCOS disrupts the menstrual cycle, causing irregularities. This includes infrequent periods and heavy bleeding. Hormonal imbalances and insulin resistance are key factors in these irregularities.
What are the common menstrual irregularities in PCOS?
In PCOS, common menstrual issues include infrequent periods, heavy bleeding, and irregular shedding of the uterine lining. These issues can cause heavy bleeding, painful periods, and other problems.
Can lifestyle changes help manage PCOS symptoms?
Yes, making lifestyle changes can help manage PCOS symptoms. This includes dietary changes, exercise, reducing stress, and getting enough sleep. These changes can help with heavy bleeding and painful periods.
What are the treatment options for heavy bleeding and pain in PCOS?
Treatment for heavy bleeding and pain in PCOS includes hormonal therapies and non-hormonal medications. Sometimes, surgery is needed. The best treatment depends on how severe the symptoms are and what the patient needs.
How is PCOS-related menstrual problems diagnosed?
Diagnosing PCOS-related menstrual issues involves a thorough evaluation. This includes looking at medical history, doing a physical exam, and running tests like ultrasound and hormonal assays.
Can PCOS cause endometrial hyperplasia?
Yes, PCOS can increase the risk of endometrial hyperplasia. This is due to unbalanced estrogen levels and irregular shedding of the uterine lining. Managing PCOS symptoms can help reduce this risk.
Does PCOS make cramps worse?
Yes, PCOS can make menstrual cramps worse. This is because of hormonal changes and inflammation. Treating PCOS symptoms can help lessen cramping.
Is PCOS associated with heavy periods?
Yes, PCOS is often linked to heavy periods, or menorrhagia. Hormonal imbalances and thickening of the uterine lining contribute to excessive bleeding.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1479713/