Last Updated on November 14, 2025 by
A dangerously low level of red blood cells (RBCs) is a serious condition that can lead to life-threatening complications. Low hemoglobin level for chemotherapy is often linked to this issue, making it crucial to understand the critical thresholds for timely medical intervention.
Hemoglobin is a protein in RBCs that carries oxygen. When the hemoglobin level for chemotherapy drops below 7“8 g/dL, severe anemia can occur. This underscores the need for early detection and high-quality care.
At Liv Hospital, we emphasize the importance of monitoring hemoglobin level for chemotherapy. This helps identify patients at risk and ensures they receive the appropriate medical care. By maintaining safe hemoglobin levels for chemotherapy, we can prevent severe anemia and achieve the best outcomes for our patients.
Key Takeaways
- A dangerously low RBC count is often defined by a hemoglobin concentration below 7“8 g/dL.
- Low hemoglobin levels can lead to life-threatening complications.
- Early detection and quality care are key to preventing severe anemia.
- Understanding critical thresholds is vital for timely medical interventions.
- Liv Hospital stresses the importance of identifying at-risk individuals and providing the right medical care.
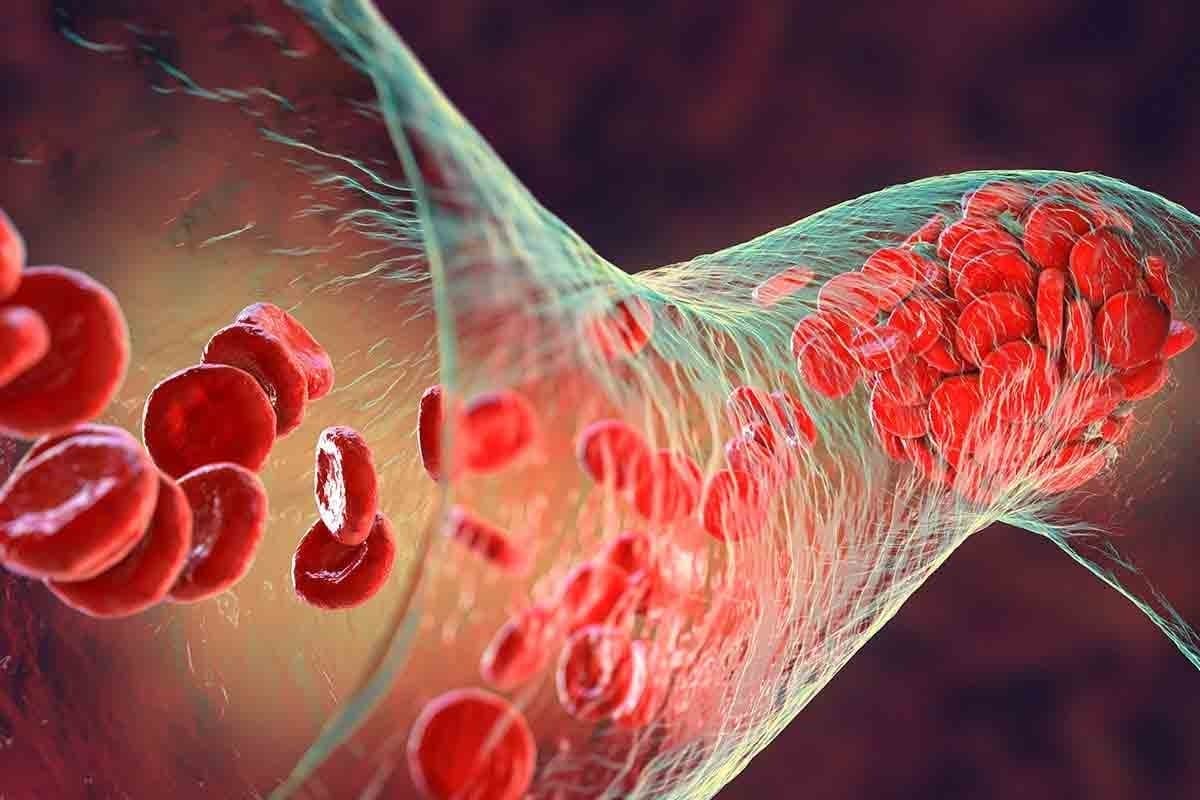
Understanding Red Blood Cells and Their Function
Red blood cells, or RBCs, are key for delivering oxygen to our body’s tissues. They carry oxygen from the lungs to our tissues and carbon dioxide back to the lungs. This is vital for our cells to survive and for our body to work right.

The Role of RBCs in Oxygen Transport
Red blood cells have a protein called hemoglobin. It binds to oxygen in the lungs and releases it to our tissues. Hemoglobin keeps the balance of oxygen and carbon dioxide in our body. Medical experts say, “Hemoglobin is what makes red blood cells good at carrying oxygen.”
“The primary function of red blood cells is to transport oxygen from the lungs to the body’s tissues and to carry carbon dioxide, a waste product, away from the tissues and back to the lungs.”
How RBCs Are Produced in the Body
Red blood cells are made in the bone marrow through erythropoiesis. This complex process turns hematopoietic stem cells into mature red blood cells. The body carefully controls RBC production to keep a steady supply.
The Lifecycle of Red Blood Cells
Red blood cells live about 120 days. After that, they are broken down by the spleen. The parts of old RBCs are then recycled or thrown out. This cycle keeps our body’s red blood cell count healthy.
Hemoglobin: The Critical Component of RBCs
Hemoglobin is a key protein in red blood cells. It’s vital for carrying oxygen around the body. Without it, our health would suffer greatly.
What Hemoglobin Does in the Body
Hemoglobin picks up oxygen in the lungs and carries it to our tissues. It’s released there, helping our cells make energy. Hemoglobin levels are a critical indicator of anemia and other blood disorders, making it a key diagnostic tool.
Low hemoglobin means our tissues might not get enough oxygen. This can cause fatigue, weakness, and other symptoms of anemia. We’ll look into the effects of low hemoglobin levels later.
The Structure of Hemoglobin
Hemoglobin is made of four polypeptide chains and four heme groups, which contain iron. This lets it bind to oxygen, carrying it to our tissues. The heme group is key for oxygen binding, making it essential for red blood cells.

The Relationship Between RBC Count and Hemoglobin Levels
There’s a direct link between red blood cell count and hemoglobin levels. More RBCs usually mean more hemoglobin. But, the health of RBCs also affects overall hemoglobin levels.
Understanding this link is key for diagnosing and treating low RBC count or anemia. We’ll explore diagnostic methods and treatments in the next sections.
Normal Hemoglobin Ranges and Variations
Knowing what normal hemoglobin levels are is key for spotting and treating health issues. Hemoglobin is a protein in red blood cells that carries oxygen. Its levels change based on gender, age, and where you live.
Standard Ranges for Men
Men usually have hemoglobin levels between 13.5 and 17.5 g/dL. This range is for healthy adult males. If your levels are outside this, it might mean you have a health problem.
Standard Ranges for Women
Women’s hemoglobin levels are slightly different, ranging from 12.0 to 15.5 g/dL. This range is for healthy adult females. Remember, these levels can change due to things like your menstrual cycle or if you’re pregnant.
Variations by Age, Altitude, and Other Factors
Hemoglobin levels can change a lot because of age, altitude, and some health conditions. For example, people at high altitudes might have more hemoglobin to handle the lower oxygen. Age and some health issues can also affect hemoglobin levels.
Healthcare providers need to know about these changes to give the right care. By understanding these factors, doctors can make better diagnoses and treatment plans.
Dangerously Low Hemoglobin Thresholds
The critical threshold for hemoglobin levels is key for both patients and healthcare providers. Levels below 7-8 g/dL are considered dangerously low. They can lead to severe health complications.
The Critical Threshold: Below 7-8 g/dL
Hemoglobin levels below 7-8 g/dL are critically low. At this level, the body’s tissues and organs may not get enough oxygen. This can lead to life-threatening complications.
Medical guidelines say patients with these levels need immediate medical attention. This may include blood transfusions or other interventions to stabilize their condition.
Risk Assessment Framework
Assessing the risk of low hemoglobin levels involves several factors. These include the patient’s overall health, any underlying medical conditions, and how fast the hemoglobin level is dropping. A detailed risk assessment framework helps healthcare providers:
- Identify patients at highest risk for severe complications
- Determine the need for immediate intervention
- Develop a tailored treatment plan to address the underlying cause of low hemoglobin
Individual Factors That Influence Danger Levels
Individual factors like age, overall health status, and chronic conditions can affect the danger level of low hemoglobin. For example, older adults or those with heart disease may experience more severe symptoms at higher hemoglobin levels than younger, healthier individuals. Understanding these factors is key for personalized care and management.
The symptoms and risks of low hemoglobin can vary widely among individuals. While some may experience severe fatigue and shortness of breath, others might have more subtle symptoms that are easily overlooked. A thorough assessment by a healthcare provider is essential to determine the best course of action.
Signs and Symptoms of Critically Low RBC
It’s important to know the signs of a low red blood cell (RBC) count. A low RBC count means less hemoglobin, a key part of red blood cells.
Early Warning Signs
In the early stages, the body might show small signs that are easy to miss. Knowing these signs can help you get medical help early. Look out for fatigue, weakness, and shortness of breath, which can really affect your day.
As the condition gets worse, these symptoms will get stronger. Watch for any changes in your body and see a doctor if something seems off.
Symptoms at Moderate Levels (8-10 g/dL)
When hemoglobin levels are between 8-10 g/dL, symptoms get worse. People might feel dizzy, have pale skin, and a fast heartbeat. This is because the body’s tissues aren’t getting enough oxygen, leading to problems.
Getting a hemoglobin blood test is key to figuring out how bad the condition is. This test helps doctors treat low RBC count right.
Severe Symptoms (Below 7 g/dL)
Below 7 g/dL, symptoms can be very serious and even life-threatening. People might feel confused, have chest pain, and severe shortness of breath. These need quick medical help to avoid serious issues.
Severe anemia can cause serious problems like hypoxia and tissue damage. So, if you have these severe symptoms, get medical help fast.
“Anemia is a condition that can have serious consequences if left untreated. Recognizing the signs and symptoms early is critical for effective management and treatment.”
Life-Threatening Complications of Severe Anemia
Severe anemia can have serious effects on the body. When hemoglobin levels drop, the body’s tissues and organs don’t get enough oxygen. This can lead to serious complications.
Hypoxia and Tissue Damage
Hypoxia is a big problem with severe anemia. It means the body’s tissues don’t get enough oxygen. This can damage tissues and make vital organs work poorly. The brain, heart, and kidneys are most at risk.
Cardiovascular Complications
Severe anemia makes the heart work harder. This can lead to cardiovascular complications. Heart failure, arrhythmias, and other heart problems can occur. People with heart issues are at even greater risk.
Multiorgan Dysfunction
As anemia gets worse, it can harm many organs. The kidneys, liver, and other vital organs may not work right. This can make it harder for the body to survive.
Long-term Health Impacts
Even if someone survives severe anemia, they may face long-term health issues. These can include ongoing fatigue, brain problems, and a higher chance of getting sick. It’s important to understand these risks to care for patients well.
We need to take anemia seriously because it can be deadly. Finding and treating it early can help prevent these serious problems. This can improve how well patients do.
Common Causes of Dangerously Low RBC
Many things can cause a dangerously low RBC count. This includes medical conditions and not getting enough nutrients. Knowing what causes it helps doctors find and fix the problem.
Acute Blood Loss
Acute blood loss means losing blood quickly. It can happen from injuries, surgery, or bleeding inside the body. Quick medical help is key to stop the bleeding and get the blood back.
Chronic Conditions
Long-term health issues like kidney disease and cancer can harm RBC production. Kidney disease lowers the hormone that helps make RBCs. Cancer can also cause anemia by affecting the bone marrow and causing inflammation.
Nutritional Deficiencies
Lacking iron, vitamin B12, or folate can stop RBCs from being made. Eating right is vital for healthy RBCs. Sometimes, we need to change our diet or take supplements.
Bone Marrow Disorders
Problems with the bone marrow, like aplastic anemia and myelodysplastic syndromes, can lower RBC counts. These issues need special treatment.
Finding out why someone has a low RBC count is very important. We will work with doctors to figure out the cause. Then, we’ll create a plan to help.
Diagnosis and Testing for Low Hemoglobin
The first step in finding out if you have low hemoglobin is a simple blood test. It’s called the Complete Blood Count (CBC). This test shows the levels of different parts in your blood, like hemoglobin.
Complete Blood Count (CBC)
A CBC checks many things in your blood. It looks at hemoglobin (Hgb) levels, red and white blood cells, and platelets. The hemoglobin test is key because it measures how much hemoglobin you have.
If your doctor thinks you might have low hemoglobin or anemia, they’ll start with a CBC. This test gives important info about your red blood cells. It helps figure out if you have low hemoglobin.
Additional Diagnostic Tests
Even with a CBC, more tests might be needed to find why your hemoglobin is low. These tests include:
- Iron studies to check for iron deficiency.
- Vitamin B12 and folate levels to see if you’re lacking these vitamins.
- Reticulocyte count to see how new red blood cells are being made.
- Bone marrow biopsy in some cases to look at how blood cells are made.
Interpreting Your Blood Test Results
It’s important to understand your blood test results. Your doctor will look at your CBC and other tests. They’ll see if your hemoglobin is normal or if it’s low.
For adults, normal hemoglobin is between 13.5-17.5 g/dL for men and 12.0-15.5 g/dL for women. If your levels are below these, you might have low hemoglobin or anemia.
Frequency of Monitoring
How often you need to check your hemoglobin depends on your health. If you have anemia or conditions that affect hemoglobin, your doctor might want to check it often.
People with chronic conditions or getting treatments that affect hemoglobin might need to be checked more often.
Treatment Approaches for Critically Low RBC
Treating critically low RBC levels requires a detailed plan to raise normal hemoglobin levels. When red blood cell counts drop severely, doctors must act quickly to prevent serious problems.
Blood Transfusion Protocols
When hemoglobin levels drop below 7 g/dL, blood transfusions are often needed. This level is key because it shows a high risk of severe anemia. Blood transfusion protocols aim to quickly boost the red blood cell count. This helps vital organs get enough oxygen.
Doctors decide on blood transfusions based on several factors. These include the patient’s health, symptoms, and the reason for low RBC count. We carefully choose the best transfusion plan for each patient.
Medical Interventions and Medications
Along with blood transfusions, medical interventions and medications are used to treat low RBC counts. Erythropoiesis-stimulating agents (ESAs) help the bone marrow make more red blood cells. ESAs are helpful for patients with chronic kidney disease or certain anemias.
Other treatments aim to fix the root cause of low RBC count. This might include treating nutritional deficiencies or managing chronic conditions that lead to anemia.
Addressing Underlying Causes
To effectively treat low RBC counts, it’s important to tackle the underlying causes. This might involve diagnosing and managing chronic diseases, fixing nutritional deficiencies, or treating bone marrow disorders.
- Diagnosing and managing chronic diseases like kidney disease or cancer.
- Correcting nutritional deficiencies, such as iron, vitamin B12, or folate deficiency.
- Treating bone marrow disorders that affect red blood cell production.
Special Considerations for Different Patient Groups
When treating low RBC counts, different patient groups need special care. For example, pregnant women, children, and patients with certain chronic conditions may need unique treatment plans.
We tailor our approach to meet the specific needs of each patient group. This personalized care helps ensure the best results for those with critically low RBC counts.
Conclusion
Low red blood cell (RBC) counts can seriously harm your health. It’s key to know the dangers of low hemoglobin levels. Hemoglobin is vital for carrying oxygen to the body’s tissues and organs.
When hemoglobin levels fall, the body’s tissues and organs might not get enough oxygen. This can lead to many health problems. At Liv Hospital, we stress the need for early detection and quality care for anemia.
We are dedicated to top-notch healthcare for anemia patients. We offer advanced treatments and support to international patients. Understanding hemoglobin and its role in RBCs helps patients manage their condition better.
If RBC levels are very low, quick medical help is needed. We work with patients to create custom treatment plans. Our goal is to fix the underlying issues and boost RBC counts to avoid more health problems.
FAQ
What is considered a dangerously low RBC level?
A dangerously low RBC level is when hemoglobin is below 7-8 g/dL. This can cause severe anemia and serious health risks.
What are the normal hemoglobin ranges for adults?
For adults, normal hemoglobin levels differ by gender. Men usually have 13.5-17.5 g/dL, while women have 12.0-15.5 g/dL.
What are the symptoms of critically low RBC count?
Symptoms range from mild to severe. Early signs include fatigue and weakness. Severe symptoms include shortness of breath, chest pain, and confusion.
What causes low hemoglobin levels?
Low hemoglobin can be caused by acute blood loss, chronic diseases like kidney disease or cancer, nutritional deficiencies, and bone marrow disorders.
How is low hemoglobin diagnosed?
Diagnosis involves a Complete Blood Count (CBC) test. This measures hemoglobin levels. Additional tests help find the cause.
What are the treatment options for critically low RBC count?
Treatment may include blood transfusions for severe cases. It also includes medical interventions and nutritional supplements for deficiencies.
What are the risks associated with severely low hemoglobin?
Risks include hypoxia, cardiovascular problems, multiorgan dysfunction, and long-term health issues if not treated or managed well.
How often should hemoglobin levels be monitored?
Monitoring frequency depends on health status, underlying conditions, and treatment plans. More frequent checks are needed for those with anemia or at risk.
Can nutritional deficiencies cause low hemoglobin?
Yes, iron, vitamin B12, and folate deficiencies are common causes of low hemoglobin. These nutrients are key for RBC production.
Are there special considerations for treating low RBC count in different patient groups?
Yes, treatment plans vary based on age, health conditions, and anemia causes. Personalized care is needed.
References
- National Heart, Lung, and Blood Institute. (2022). What Is Anemia? Retrieved from https://www.nhlbi.nih.gov/health-topics/anemia