Last Updated on October 21, 2025 by mcelik

Autoimmune hemolytic anemia (AIHA) is a rare condition. It happens when the immune system attacks and destroys red blood cells. This leads to anemia. Diagnosing AIHA is very important because it can greatly affect a person’s life.
We find out if someone has AIHA by looking at their symptoms and doing lab tests. These include hemolysis labs, which check if red blood cells are being destroyed and if there are autoantibodies against them.
Hemolysis labs are key in confirming AIHA and helping doctors decide how to treat it.
Red blood cell destruction, or hemolysis, is key in hemolytic anemia. This condition happens when red blood cells are destroyed faster than they can be made. It can be caused by immune or non-immune factors.
Hemolytic anemia is when red blood cells are destroyed too early. This can happen inside or outside the blood vessels, mainly in the spleen. It leads to an imbalance between red blood cell production and destruction, causing anemia.
Red blood cell destruction can come from many sources. This includes immune-mediated processes, infections, medications, and mechanical damage. Knowing these causes is important for diagnosing and treating hemolytic anemia.
Hemolytic anemias are divided into immune and non-immune causes. Immune hemolytic anemia happens when the immune system attacks red blood cells. This includes autoimmune hemolytic anemia (AIHA), where the body attacks its own red blood cells.
Non-immune hemolytic anemia comes from other causes. These include genetic conditions, infections, certain medications, and mechanical damage to red blood cells.
Autoimmune hemolytic anemia (AIHA) is a condition where the immune system attacks the body’s red blood cells. It can be divided into types based on the temperature at which the autoantibodies react. Knowing these types is key for diagnosis and treatment.
Warm AIHA is the most common type, making up 70-80% of cases. Autoantibodies bind to red blood cells at body temperature, marking them for destruction. It affects 1-4 people per 100,000 each year, with no age limit and more women than men.
The causes of warm AIHA include genetics, environmental factors, and immune system issues. Autoantibodies, mainly IgG, target red blood cells. These cells are then destroyed by macrophages in the spleen.
Cold AIHA happens when autoantibodies react with red blood cells at cooler temperatures. It’s often linked to infections like Mycoplasma pneumoniae or Epstein-Barr virus. It can also be caused by certain lymphoproliferative disorders or be idiopathic.
The autoantibodies in cold AIHA are usually IgM, known as cold agglutinins. They cause red blood cells to clump together in cooler areas. This leads to hemolysis when the cells warm up.
Mixed type AIHA has both warm and cold autoantibodies. This rare form makes diagnosis and treatment hard.
Paroxysmal cold hemoglobinuria (PCH) is rare and usually occurs in children after a viral infection. It’s caused by the Donath-Landsteiner antibody, an IgG autoantibody that binds to red blood cells in the cold and causes hemolysis when warmed.
| Type of AIHA | Autoantibody Characteristics | Clinical Features |
| Warm AIHA | IgG, reactive at 37 °C | Chronic anemia, splenomegaly |
| Cold AIHA | IgM, reactive at cold temperatures | Acrocyanosis, hemoglobinuria upon cold exposure |
| Mixed Type AIHA | Both IgG and IgM | Combination of warm and cold AIHA features |
| Paroxysmal Cold Hemoglobinuria | Donath-Landsteiner IgG antibody | Recurrent episodes of hemoglobinuria after cold exposure |
The symptoms of autoimmune hemolytic anemia can differ a lot from person to person. They often include signs of anemia and hemolysis. These symptoms come from having fewer red blood cells and how the body reacts to their breakdown.
People with this condition often feel fatigued, jaundiced, and short of breath. These symptoms happen because the blood can’t carry as much oxygen. Also, bilirubin builds up, which is a result of red blood cells being destroyed.
When doctors check patients, they might see pallor, jaundice, and sometimes splenomegaly. The spleen gets bigger because it’s working hard to remove damaged red blood cells.
Some patients might also notice dark urine and fatigue. These symptoms can really affect their daily life. How bad these symptoms are can change a lot, depending on how fast red blood cells are being destroyed and how well the body can handle it.
It’s very important to tell AIHA apart from other anemias. Key signs include hemolysis indicators like high LDH, low haptoglobin, and high indirect bilirubin. The direct antiglobulin test (DAT), or Coombs test, is usually positive in AIHA. This helps doctors know it’s not another type of anemia.
To diagnose AIHA correctly, doctors need to look at the patient’s medical history, do a physical exam, and run lab tests. This helps them figure out if it’s AIHA or another anemia like microangiopathic or hereditary hemolytic anemia.
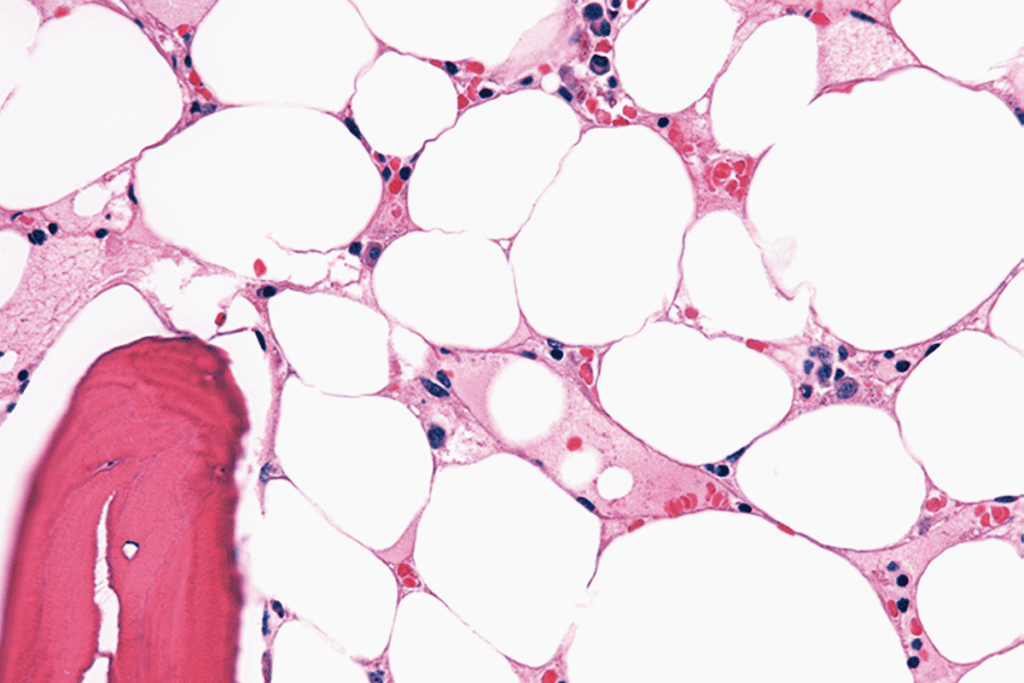
Diagnosing hemolytic anemia starts with detailed lab tests. These include a CBC and a peripheral blood smear. These tests help spot hemolysis and guide further checks.
A CBC is key for patients with suspected hemolytic anemia. It shows how severe the anemia is through hemoglobin (Hb) and hematocrit (Hct) levels. Low Hb and Hct levels mean more red blood cells are being destroyed.
The CBC also looks at red blood cell count (RBC), mean corpuscular volume (MCV), and red cell distribution width (RDW). These help understand the type of anemia and its cause.
| CBC Parameter | Typical Findings in Hemolytic Anemia |
| Hemoglobin (Hb) | Decreased |
| Hematocrit (Hct) | Decreased |
| Mean Corpuscular Volume (MCV) | Variable |
| Red Cell Distribution Width (RDW) | Often increased |
The peripheral blood smear is a vital part of the initial tests. It lets us see red blood cells directly. It can show signs of hemolytic anemia like spherocytes, schistocytes, or agglutination.
Spherocytes are often seen in warm autoimmune hemolytic anemia. Agglutination is more common in cold autoimmune hemolytic anemia. The smear can also show polychromasia, which means the bone marrow is working hard to replace lost red blood cells.
By looking at the CBC and peripheral blood smear together, we get a full picture of the patient’s condition. This helps us decide on the next steps to confirm hemolytic anemia.
Laboratory tests are key in finding out if red blood cells are being destroyed. They help see how much damage is done and why. This information helps doctors decide on the best treatment.
The reticulocyte count shows how well the bone marrow is making new red blood cells. It’s a sign of how the bone marrow is reacting to anemia. If the count goes up, it means the bone marrow is working hard to replace lost red blood cells.
Reticulocyte Index Calculation: This index adjusts the reticulocyte count for anemia and early release from the bone marrow. It gives a clearer picture of how well the bone marrow is responding.
| Parameter | Normal Value | Interpretation in Hemolysis |
| Reticulocyte Count | 0.5-1.5% | Increased |
| Reticulocyte Index | 1-2 | Increased, indicating appropriate bone marrow response |
Serum bilirubin levels are important in diagnosing hemolytic anemia. The indirect (unconjugated) bilirubin goes up when red blood cells break down.
Direct vs. Indirect Bilirubin: Direct bilirubin is linked to liver and bile duct problems. Indirect bilirubin is a sign of hemolysis.
Lactate dehydrogenase (LDH) is found in many tissues, including red blood cells. High LDH levels mean cell destruction, making it a good marker for hemolysis.
LDH Isoenzymes: LDH has different forms, with LDH-1 being specific to red blood cells. High LDH-1 levels point to hemolysis.
| LDH Isoenzyme | Tissue Specificity |
| LDH-1 | Heart, Red Blood Cells |
| LDH-2 | Reticuloendothelial System |
| LDH-3 | Lungs |
In conclusion, tests like reticulocyte count, serum bilirubin, and LDH are key in diagnosing and managing hemolytic processes. They help understand the extent of red blood cell destruction and how the bone marrow is responding. This information guides doctors in treating patients.
Knowing about haptoglobin and hemopexin is key for diagnosing and treating hemolytic anemia. These proteins are important markers that help doctors see how much hemolysis is happening in patients.
Haptoglobin is a protein that grabs onto free hemoglobin from broken red blood cells. When red blood cells break down, haptoglobin levels go down because it binds to the hemoglobin. This makes a complex that is then taken out of the blood. So, low haptoglobin levels mean there’s hemolysis happening.
Haptoglobin testing is a useful tool for doctors. It checks the blood for haptoglobin levels. Low levels mean there’s hemolysis. But, it’s important to look at other signs and tests too. Some conditions, like liver disease, can also change haptoglobin levels.
| Haptoglobin Level | Interpretation |
| Low | Indicative of hemolysis |
| Normal | May not rule out hemolysis; consider other markers |
| Elevated | May indicate an acute phase response |
Hemopexin is a protein that grabs onto heme, the part of hemoglobin, very well. When there’s a lot of hemolysis, hemopexin gets used up because it binds to heme. This helps remove heme from the blood and reduces oxidative stress.
Hemopexin’s role in hemolysis is similar to haptoglobin’s. While haptoglobin grabs onto free hemoglobin, hemopexin grabs onto heme. Together, they help deal with the waste from broken red blood cells.
Other proteins that bind to hemoglobin might also play a part in hemolytic anemia. But, their use as markers for diagnosis might not be as clear.
In summary, haptoglobin and hemopexin are key markers for diagnosing and managing hemolytic anemia. Understanding their roles and how to read their levels is very helpful for doctors.
The Direct Antiglobulin Test (DAT), also known as the Coombs test, is key in diagnosing Autoimmune Hemolytic Anemia (AIHA). It helps find antibodies or complement attached to red blood cells. This is a key sign of AIHA.
The DAT starts with a sample of the patient’s red blood cells. These cells are washed to remove any free antibodies. Then, they are mixed with anti-human globulin (AHG).
This AHG reacts with any antibodies or complement proteins on the red blood cells. If these proteins are there, agglutination happens.
Key steps in the DAT process include:
A positive DAT means there are antibodies or complement on the red blood cells. This supports an AIHA diagnosis. But, a negative result doesn’t mean AIHA is ruled out.
It’s important to look at DAT results with other clinical and lab findings.
“The DAT is a cornerstone in the diagnosis of AIHA, providing direct evidence of immune-mediated red blood cell destruction.”
The DAT is a valuable tool but has its limits. False positives can happen due to recent blood transfusions or certain drugs. False negatives might be due to low antibody levels or test issues.
Knowing these limitations helps in accurately diagnosing and managing AIHA.
The indirect antiglobulin test is key in finding antibodies against red blood cell antigens in patient serum. It’s essential for diagnosing and managing Autoimmune Hemolytic Anemia (AIHA).
The indirect Coombs test, or indirect antiglobulin test, finds antibodies or complement proteins bound to red blood cells. It mixes the patient’s serum with donor red blood cells. If antibodies are present, they bind to the red blood cells.
Then, antiglobulin reagent is added. This causes the red blood cells to clump if antibodies are there.
Key steps in the indirect Coombs test include:
The indirect antiglobulin test is key in AIHA diagnosis. It finds autoantibodies against red blood cell antigens. This info is vital for choosing the right blood for transfusions.
The indirect Coombs test is also used for monitoring and managing AIHA. It helps assess the risk of hemolytic transfusion reactions. This makes blood transfusion decisions safer.
In summary, the indirect antiglobulin test is a vital tool in AIHA management. It gives important info on red blood cell antibodies. This helps in better patient care and disease management.
Cold agglutinin testing is key for finding cold-reactive antibodies in autoimmune hemolytic anemia (AIHA). It helps diagnose cold AIHA, where the immune system attacks red blood cells at cold temperatures.
The cold agglutinin titer shows how much cold-reactive antibodies are in the blood. High levels mean cold AIHA. We check this to see how bad the condition is and if treatment is working.
A high titer means lots of antibody activity, which can cause red blood cells to break down. We test at different temperatures to see how wide the antibody range is.
| Cold Agglutinin Titer | Interpretation |
| Normal | No evidence of cold AIHA |
| Elevated | Suggestive of cold AIHA |
| Significantly Elevated | High likelihood of cold AIHA |
Thermal amplitude testing shows when cold-reactive antibodies react with red blood cells. It’s important for understanding the cold agglutinin titer’s meaning.
Antibodies that react at higher temperatures can cause more damage. We match the test results with symptoms to decide on treatment.
Knowing the cold agglutinin titer and thermal amplitude helps us manage cold AIHA better. These tests tell us about the antibodies’ presence and activity, helping us choose the right treatment.
To diagnose hemolytic anemia, we use many specialized tests. These tests help find the cause and guide treatment.
Flow cytometry is a key tool for finding paroxysmal nocturnal hemoglobinuria (PNH). PNH is a rare disorder that causes hemolytic anemia. It checks the proteins on red blood cells for certain missing proteins, like CD55 and CD59.
Flow cytometry offers:
The osmotic fragility test helps diagnose membrane disorders. Hereditary spherocytosis is one such condition. It causes red blood cells to break down easily. The test checks how well red blood cells handle different salt solutions.
The test involves:
Hemoglobin electrophoresis and genetic testing are key for diagnosing hemoglobinopathies. These include sickle cell disease and thalassemia. They check the types of hemoglobin and look for specific gene mutations.
These tests offer:
Using these tests, we can accurately find the causes of hemolytic anemia. Then, we can create treatment plans that meet each patient’s needs.
To manage hemolytic anemia well, we must tell AIHA apart from other disorders. This means using precise lab tests to find out what’s causing the problem. We look at AIHA, alloimmune hemolytic anemia, drug-induced immune hemolytic anemia, and non-immune hemolytic anemias.
Alloimmune hemolytic anemia is when the body attacks red blood cells it sees as foreign. This can happen in transfusion reactions and hemolytic disease of the newborn (HDN). Transfusion reactions occur when the blood types don’t match, causing red blood cells to break down. HDN happens when mom’s antibodies attack the baby’s red blood cells.
Tests like the direct antiglobulin test (DAT) can spot these problems. They find antibodies or complement on red blood cells.
Some medicines can make the body attack its own red blood cells. Finding out which drug is causing this is key. Tests like the DAT and drug-dependent antibody testing help figure this out. Knowing which drug is the problem is important for treatment.
Non-immune hemolytic anemias come from problems with red blood cell enzymes or membranes. For example, G6PD deficiency and hereditary spherocytosis. To diagnose these, we use tests like osmotic fragility testing and enzymatic assays.
Getting the right diagnosis is key to treating these conditions properly.
Diagnosing hemolytic anemia in dogs involves various tests. These tests are similar to those used in humans but have some key differences. Knowing these differences is vital for vets to treat dogs with hemolytic anemia well.
Immune-mediated hemolytic anemia (IMHA) is a common issue in dogs. It happens when the immune system attacks and destroys red blood cells. To diagnose IMHA in dogs, specific tests are used:
These tests help vets figure out if a dog has IMHA and what’s causing the anemia.
Even though some tests for hemolytic anemia are the same for humans and dogs, there are big differences. For example, the Direct Antiglobulin Test is used in both but might mean different things because of different antibodies.
| Test | Human Application | Canine Application |
| Direct Antiglobulin Test (DAT) | Diagnoses autoimmune hemolytic anemia | Diagnoses immune-mediated hemolytic anemia |
| Complete Blood Count (CBC) | Checks for anemia and blood health | Looks for anemia and spherocytes |
| Peripheral Blood Smear | Looks at red blood cell shape | Finds spherocytes and other shape changes |
It’s important for vets to know these differences. This knowledge helps them make accurate diagnoses and treatment plans for dogs.
Hemolysis in lab samples is a big problem. It makes many tests less accurate. When red blood cells break down, they spill their contents into the plasma or serum. This messes up lab tests.
We must know how hemolysis changes lab results. It can mess with tests for liver health, electrolytes, and heart markers.
Hemolysis can change lab test results in many ways. For example, it can:
The table below shows how hemolysis can affect lab tests:
| Laboratory Parameter | Effect of Hemolysis |
| Potassium (K+) | Increased |
| Lactate Dehydrogenase (LDH) | Increased |
| Aspartate Aminotransferase (AST) | Increased |
| Bilirubin | Variable effect |
To cut down on hemolysis, we need to handle samples right. Here are some tips:
By following these steps, we can lower hemolysis in lab samples. This means our test results will be more reliable.
To understand hemolysis labs, we need a detailed approach. This means looking at lab values, matching them with clinical signs, and considering the patient’s history.
Spotting patterns in lab results is key for diagnosing hemolytic anemia. We search for signs like high lactate dehydrogenase (LDH) and indirect bilirubin levels. These show that hemolysis is happening. A complete blood count (CBC) gives us vital info on the severity of anemia and other issues.
Linking lab results with symptoms and medical history is vital for correct diagnosis and treatment. We look at signs like jaundice, fatigue, and shortness of breath. We also consider the patient’s past health, including any past hemolysis or underlying conditions.
“The diagnosis of hemolytic anemia requires a complete approach, combining lab results with clinical findings and medical history.”
” Expert Opinion
By mixing lab results with clinical knowledge, we can create a treatment plan that fits each patient’s needs.
Managing autoimmune hemolytic anemia (AIHA) well means watching how treatment works through lab tests. This helps doctors see if the treatment is working and make changes if needed.
For AIHA, some lab tests are very important. They help doctors see if treatment is working. These include:
Watching these tests helps doctors know if treatment is working. It also helps them decide what to do next.
How often to test AIHA patients depends on how bad the condition is and the treatment. At first, tests need to be done more often to see how treatment is going and make changes if needed.
| Parameter | Initial Testing Frequency | Expected Change |
| Hemoglobin | Weekly or biweekly | Increase |
| Reticulocyte Count | Weekly or biweekly | Decrease |
| LDH | Weekly or biweekly | Decrease |
| Bilirubin | Weekly or biweekly | Decrease |
As the patient gets better, tests might not need to be done as often. But, it’s important to keep testing to manage AIHA long-term.
Hemolytic anemia diagnosis is changing fast with new technologies. These changes help us get better at finding what’s wrong and why. They also give us new ways to understand this condition.
Advanced serological techniques are key in diagnosing hemolytic anemia. They use special tests to find and understand antibodies against red blood cells.
One big step is making tests more sensitive and accurate. For example, new methods like gel-based technologies and column agglutination tests help spot weak antibodies better. This cuts down on false negatives.
Automation has also made testing faster and more reliable. This is great for labs that do a lot of tests. It means they can work more efficiently and accurately.
Molecular and genetic tests are becoming more common for diagnosing hemolytic anemia. They help us understand the genetic causes of some disorders. This lets us tailor treatments better.
Genetic tests can find specific mutations in hereditary hemolytic anemias. This is important for counseling families and making treatment plans that fit each patient.
| Technology | Description | Clinical Application |
| Advanced Serological Tests | Improved detection of autoantibodies against red blood cells | Diagnosis of autoimmune hemolytic anemia |
| Molecular Testing | Genetic analysis to identify mutations associated with hemolytic anemia | Diagnosis of hereditary hemolytic anemias, genetic counseling |
| Genetic Testing | Identification of specific genetic mutations | Targeted therapeutic interventions, personalized medicine |
In conclusion, new technologies are changing how we diagnose and treat hemolytic anemia. By using advanced serological and genetic tests, we can diagnose more accurately. This leads to better treatments for patients.
Laboratory testing is key in diagnosing and managing Autoimmune Hemolytic Anemia (AIHA). We’ve talked about the tests used to find AIHA, check how well treatments work, and help doctors make decisions.
For the best AIHA care, doctors need to look at lab results, the patient’s symptoms, and medical history together. This helps them make better choices for their patients.
In our final thoughts, we stress how important lab tests are in managing AIHA. By using these tests well, doctors can accurately diagnose AIHA, track treatment success, and change plans as needed. This approach helps ensure patients get the best care possible.
AIHA is a condition where the immune system attacks the body’s red blood cells. This leads to their early destruction.
Symptoms include pale skin, jaundice, an enlarged spleen, and feeling very tired. These are due to the anemia.
Doctors use a few tests to diagnose AIHA. These include a complete blood count, a blood smear, and a reticulocyte count. They also do a Direct Antiglobulin Test (DAT/Coombs test).
The DAT test finds antibodies or complement on red blood cells. It helps confirm AIHA by showing autoantibodies.
Warm AIHA happens when autoantibodies attack red blood cells at body temperature. Cold AIHA occurs when autoantibodies attack at cooler temperatures.
Tests like the reticulocyte count and serum bilirubin levels check for hemolysis. They also look at LDH, haptoglobin, and hemopexin levels.
Haptoglobin binds to free hemoglobin. Low levels of haptoglobin mean there’s hemolysis. It’s a key marker for diagnosing hemolytic conditions.
Yes, AIHA can be identified through specific tests. These include the DAT and certain features on the blood smear.
Doctors track how well treatment is working with lab tests. They look at hemoglobin levels, reticulocyte count, and markers of hemolysis.
New technologies include advanced serological tests and molecular and genetic testing. They help improve diagnosis and give new insights into hemolytic anemia.
Hemolysis can make some lab results wrong. It’s important to handle and process samples correctly to get accurate results.
Yes, there are differences in diagnosing hemolytic anemia in humans and dogs. The specific tests used vary between species.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!