Hemolytic anemia is a condition that affects millions worldwide. It causes the premature destruction of red blood cells. This condition can lead to significant health issues, including fatigue, jaundice, and shortness of breath. It impacts the quality of life for those affected.
We will explore what hemolytic anemia is and its significance in the medical field. It is characterized by the accelerated destruction of red blood cells. This can be caused by various factors, including genetic disorders, infections, and certain medications.
Understanding this condition is key for providing the right care and support to patients.
Key Takeaways
- Hemolytic anemia involves the premature destruction of red blood cells.
- It can be caused by genetic disorders, infections, or certain medications.
- Symptoms include fatigue, jaundice, and shortness of breath.
- Understanding the condition is key to providing appropriate patient care.
- Early diagnosis and treatment can significantly improve patient outcomes.
Understanding Red Blood Cell Destruction

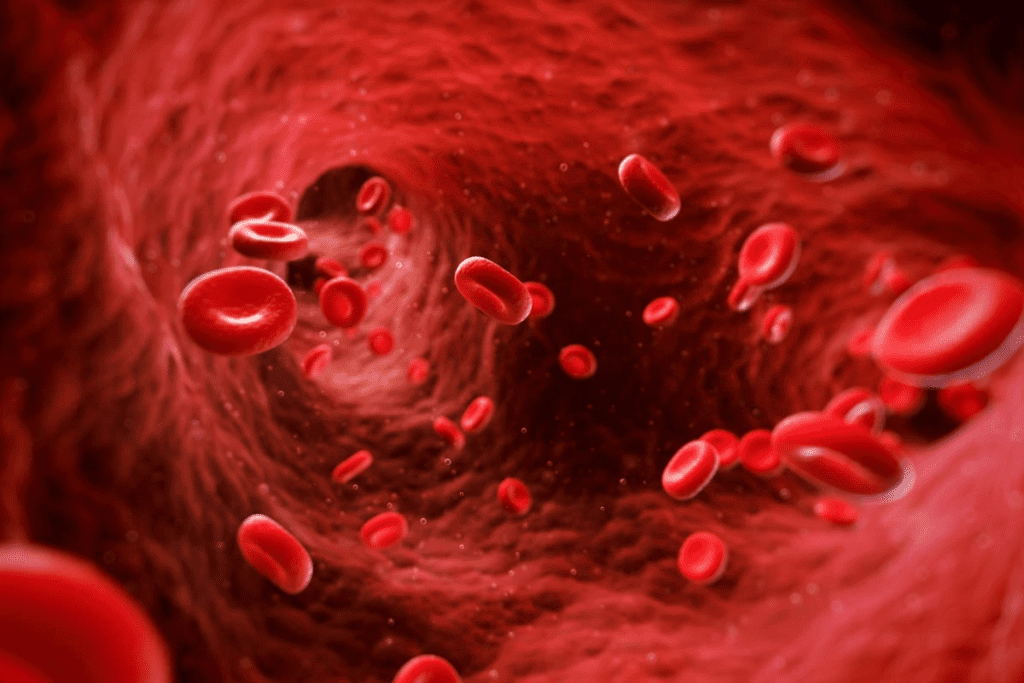
It’s important to know how red blood cells are destroyed to understand hemolytic anemia. These cells carry oxygen to all parts of the body. When they break down, it can harm our health.
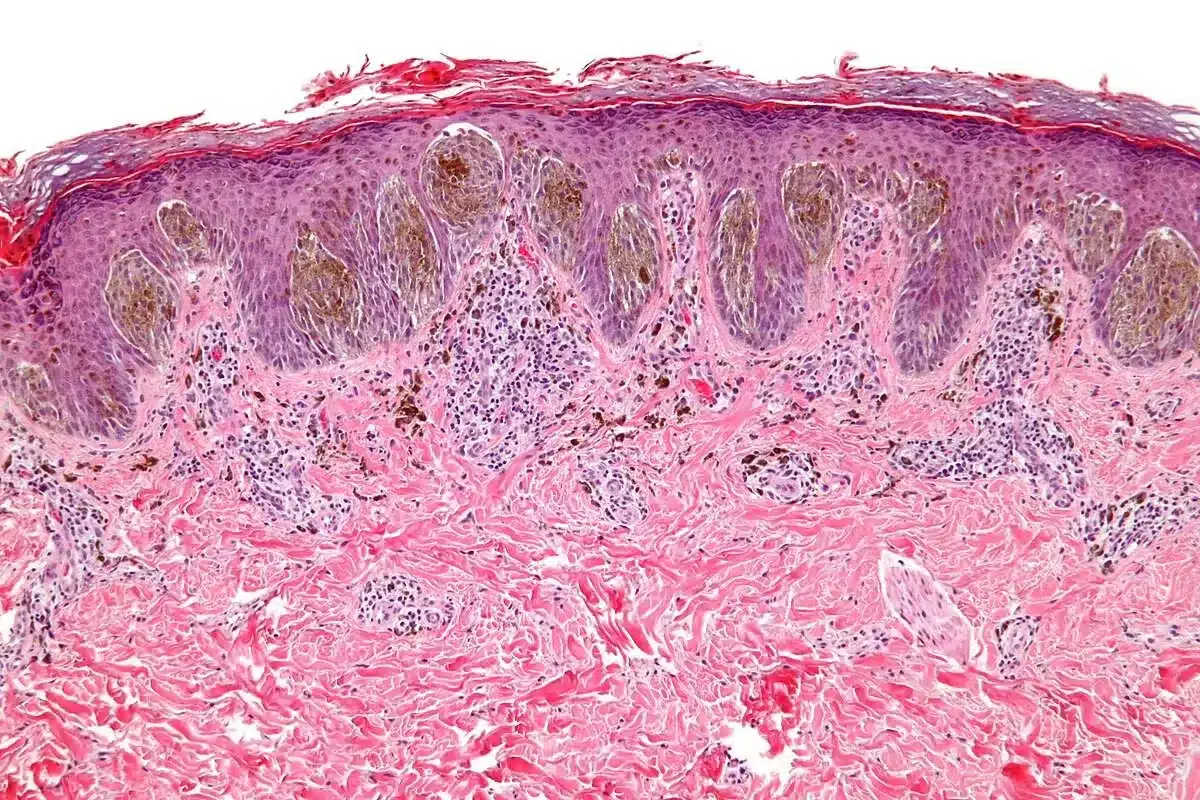
The Normal Lifecycle of Red Blood Cells
Red blood cells, or erythrocytes, start in the bone marrow. They live for about 120 days. During this time, they lose their nucleus and organelles to carry more oxygen.
Red blood cell production and destruction must stay in balance. The body makes 2 million new cells every second. This keeps oxygen levels healthy in our bodies.
Premature Destruction Process
Hemolysis happens when red blood cells break down too early. It can be due to problems inside the cells or outside factors like infections. When cells break down faster than they’re made, it causes anemia.
Acute hemolysis happens quickly and can be dangerous. Chronic hemolysis goes on for a long time and can cause serious health problems.
| Causes of Hemolysis | Description |
| Intrinsic Factors | Defects within the red blood cells, such as membrane disorders or enzyme deficiencies. |
| Extrinsic Factors | External factors, including infections, medications, or autoimmune disorders. |
Impact on Oxygen Transport
When red blood cells are destroyed, less oxygen is carried to our bodies. This can cause tiredness, shortness of breath, and dizziness.
The severity of these symptoms depends on how fast and much red blood cells are destroyed. In severe cases, hemolytic anemia can be very dangerous if not treated.
What is Hemolytic Anemia?
Hemolytic anemia is when red blood cells are destroyed too quickly. This can cause serious health problems if not treated.
Definition and Basic Mechanism
Hemolytic anemia happens when red blood cells are destroyed faster than they’re made. Normally, these cells last about 120 days. But in this condition, they don’t last as long.
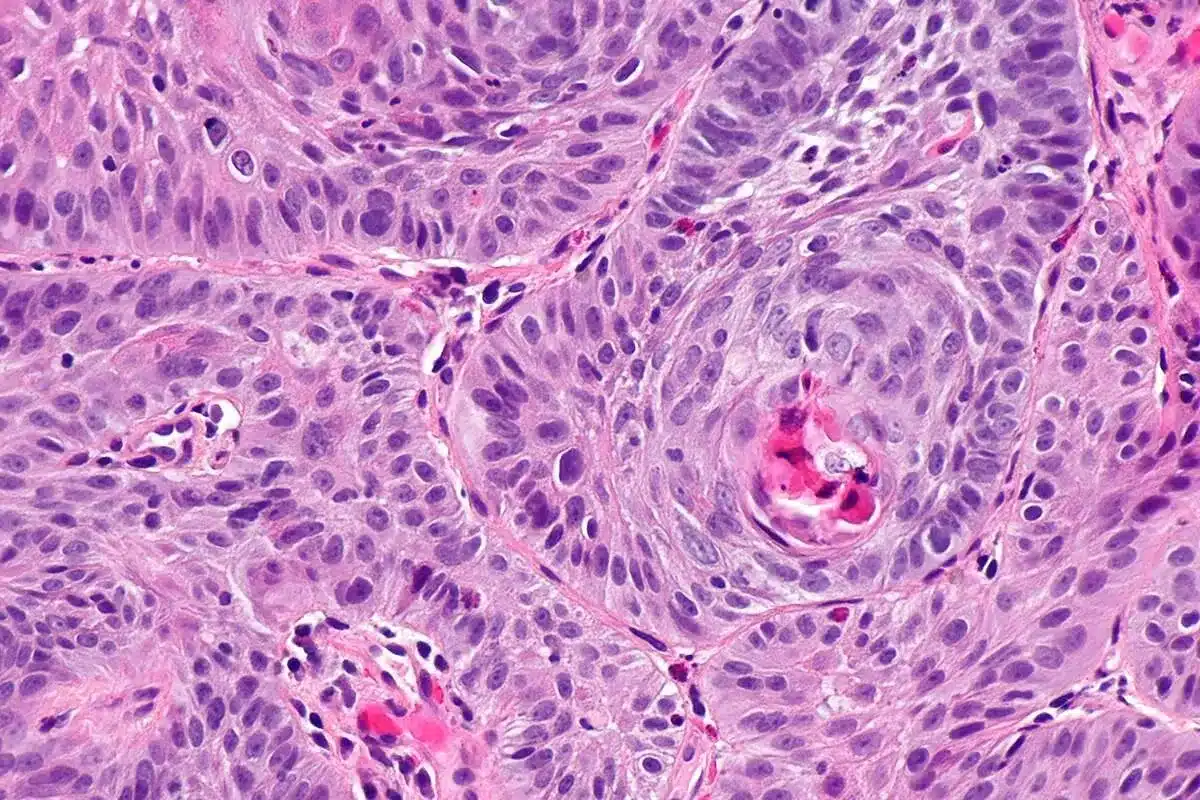
Hemolysis Explained
Hemolysis is when red blood cells are destroyed. This can happen inside or outside blood vessels. Inside, it’s often due to fragile red blood cells.
Difference Between Hemolytic and Other Types of Anemia
Anemia is a general term for low red blood cells or hemoglobin. Hemolytic anemia is different. It’s caused by red blood cells being destroyed too fast, unlike iron-deficiency anemia, which is due to a lack of iron.
Types of Hemolytic Anemia

Hemolytic anemia can be divided into inherited and acquired types. Knowing the type helps doctors understand the cause and choose the right treatment.
Inherited Hemolytic Anemias
Inherited hemolytic anemias come from genetic mutations. These affect how red blood cells are made or work. They are present from birth and can be mild or severe.
Sickle Cell Disease is a well-known inherited anemia. It happens when a gene for hemoglobin is mutated. This causes red blood cells to be misshapen and easily broken down.
Thalassemia is another inherited condition. It leads to less hemoglobin being made. This causes anemia and other health issues.
Acquired Hemolytic Anemias
Acquired hemolytic anemias start later in life. They can be caused by autoimmune disorders, infections, some medicines, and toxins.
Autoimmune Hemolytic Anemia (AIHA) happens when the immune system attacks its own red blood cells. This marks them for destruction.
Other causes include infections like malaria and some medicines that can cause red blood cells to break down.
It’s important to know if someone has inherited or acquired hemolytic anemia. This helps doctors pick the best treatment.
Causes of Hemolytic Anemia
To understand hemolytic anemia, we need to look at red blood cells and what happens to them. This condition means red blood cells break down too early. Knowing why this happens is key to treating it.
Intrinsic Causes (Within the Red Blood Cell)
Intrinsic causes come from inside the red blood cells. These can be genetic problems that affect how red blood cells work. For example, sickle cell disease and thalassemia are inherited and cause hemolytic anemia.
Genetic mutations can also cause problems. Hereditary spherocytosis makes red blood cells more likely to break down. Glucose-6-phosphate dehydrogenase (G6PD) deficiency makes them more vulnerable to damage.
Extrinsic Causes (Outside the Red Blood Cell)
Extrinsic causes come from outside the red blood cells. Autoimmune disorders can attack red blood cells, marking them for destruction. Infections, some medicines, and toxins can also harm red blood cells.
Another cause is mechanical damage. This can happen with mechanical heart valves or in microangiopathic hemolytic anemia. Here, red blood cells get damaged by shear stress.
Common Symptoms of Hemolytic Anemia
Hemolytic anemia is when red blood cells break down too early. This leads to symptoms that can really affect a person’s life.
General Symptoms
People with hemolytic anemia often feel tired, weak, and have trouble breathing. This is because they don’t have enough red blood cells. These cells are key for carrying oxygen to the body’s tissues.
Specific Symptoms
Some people may also see their skin and eyes turn yellow. This is called jaundice and happens when red blood cells break down. An enlarged spleen is another symptom, as it tries to filter out damaged cells.
Symptom Severity and Progression
The severity of symptoms can vary a lot. It depends on the cause, how fast red blood cells are destroyed, and how well the body can cope. Some people might only have mild symptoms, while others face more serious issues.
Diagnosing Hemolytic Anemia
To find out if someone has hemolytic anemia, doctors use several steps. They do physical exams and blood tests. It’s important to get this diagnosis right to treat the condition well.
Physical Examination
The first thing doctors do is a physical exam. They look for signs like pale skin, jaundice, or an enlarged spleen. These signs might show if someone has hemolytic anemia.
- Pale skin means there are fewer red blood cells.
- Jaundice is when there’s too much bilirubin.
- An enlarged spleen can be linked to hemolytic anemia.
Blood Tests
Blood tests are key to diagnosing hemolytic anemia. They check for anemia and if it’s caused by hemolysis. Important tests include:
- Complete Blood Count (CBC): Checks the levels of different blood cells.
- Reticulocyte Count: Looks at young red blood cells to see if the bone marrow is making more.
- Bilirubin Levels: High levels can mean hemolysis.
- Lactate Dehydrogenase (LDH): High LDH means red blood cells are being destroyed.
Specialized Tests
For some cases, doctors need special tests to find the cause of hemolytic anemia. These include:
- Osmotic Fragility Test: Helps find hereditary spherocytosis, a red blood cell problem.
- Direct Antiglobulin Test (DAT): Finds antibodies or proteins on red blood cells that can cause hemolytic anemia.
- Genetic Testing: Finds inherited hemolytic anemia, like sickle cell disease or thalassemia.
Doctors use physical exams, blood tests, and special tests together. This way, they can accurately diagnose hemolytic anemia and find the cause.
Treatment Approaches for Hemolytic Anemia
Treating hemolytic anemia requires a detailed plan. It focuses on both symptoms and the root cause. Knowing the type and severity of the condition is key.
Treating Underlying Causes
Fixing the underlying cause is essential. This might mean treating autoimmune diseases, stopping certain drugs, or fighting off infections.
For inherited conditions like sickle cell disease, special treatments help. They aim to lessen pain and manage complications.
Blood Transfusions
Blood transfusions are often needed. They boost the number of healthy red blood cells. This is critical in severe cases or during crises.
Transfusions improve oxygen delivery to tissues. They also lower the risk of serious problems.
Medications
Medicines play a big role in treating hemolytic anemia. Corticosteroids, like prednisone, slow down hemolysis.
Immunosuppressive drugs are used for autoimmune causes. They help control the immune system.
Surgical Interventions
Surgery is sometimes needed. For example, removing the spleen (splenectomy) helps some patients.
The right treatment depends on the cause, anemia severity, and the patient’s health.
| Treatment Approach | Description | Indications |
| Treating Underlying Causes | Addressing the root cause of hemolysis | Autoimmune hemolytic anemia, drug-induced hemolysis |
| Blood Transfusions | Increasing healthy red blood cell count | Severe anemia, crisis situations |
| Medications | Corticosteroids, immunosuppressives | Reducing hemolysis, managing autoimmune reactions |
| Surgical Interventions | Splenectomy | Certain cases of hereditary spherocytosis, autoimmune hemolytic anemia |
Complications of Untreated Hemolytic Anemia
Untreated hemolytic anemia can lead to serious health issues. Acute and chronic complications can arise if left unmanaged.
Acute Complications
One of the immediate risks is aplastic crisis, often triggered by viral infections. This condition severely reduces red blood cell production.
Chronic Complications
Chronic issues include gallstones and heart problems due to prolonged hemolysis. Managing hemolytic anemia effectively is key to prevent these outcomes.
FAQ
What is hemolytic anemia?
Hemolytic anemia is when red blood cells break down too early. This leads to a lack of red blood cells. It makes it hard for the body to get enough oxygen.
What causes hemolytic anemia?
It can be caused by problems inside the red blood cells or outside factors. These include infections, medicines, or autoimmune diseases that harm red blood cells.
What are the symptoms of hemolytic anemia?
Symptoms include feeling tired, weak, and pale. You might also have shortness of breath and jaundice. How bad these symptoms are depends on the cause and how fast red blood cells are destroyed.
How is hemolytic anemia diagnosed?
Doctors use a physical exam and blood tests to diagnose it. They check the red blood cell count and look for signs of hemolysis. They might also do special tests to find the cause.
What are the treatment options for hemolytic anemia?
Treatment depends on the cause. It might include blood transfusions, medicines to stop hemolysis, or surgery in some cases.
What is hemolysis?
Hemolysis is when red blood cells are destroyed. It can happen normally or because of disease, like hemolytic anemia.
How does hemolytic anemia affect oxygen transport in the body?
It reduces the number of red blood cells. This makes it harder for oxygen to reach the body’s tissues. It can cause tissue hypoxia and symptoms.
Can hemolytic anemia be inherited?
Yes, some types are inherited. This includes sickle cell disease and other genetic disorders that affect red blood cells.
What are the complications of untreated hemolytic anemia?
Without treatment, it can cause severe anemia and organ failure. It can also lead to iron overload and a higher risk of infections.
How can hemolytic anemia be managed?
Managing it involves treating the cause, monitoring red blood cell count, and managing symptoms. It’s important to address complications as they happen.
References
- Pastori, D., & Cattaneo, M. (2024). Factor V Leiden thrombophilia. GeneReviews ®. https://www.ncbi.nlm.nih.gov/books/NBK1368/
- Hager, J., & Kujovich, J. L. (2011). Genetest review: Factor V Leiden thrombophilia. American Journal of Hematology, 86(6), 479“484. https://www.sciencedirect.com/science/article/pii/S1098360021040430