Last Updated on December 1, 2025 by Bilal Hasdemir
Diagnosing liver cancer in children is complex. A biopsy is key to figuring out the disease’s type and stage. Is a Hepatoblastoma biopsy performed? Learn the key reasons why this test is absolutely needed for accurate diagnosis.
Hepatoblastoma is a rare liver cancer mainly found in kids. Getting the diagnosis right is vital for treatment.
We know how important quick and accurate diagnosis is. A biopsy is a big step. It helps doctors create a good treatment plan.
Key Takeaways
- Liver cancer diagnosis in children requires a thorough approach.
- A biopsy is essential for identifying the type and stage of liver cancer.
- Hepatoblastoma is a rare and complex disease that requires specialized care.
- Accurate diagnosis is critical for developing an effective treatment plan.
- Pediatric liver tumor diagnosis involves a range of tests and procedures.
Understanding Hepatoblastoma: A Rare Pediatric Liver Cancer
Learning about hepatoblastoma is key to catching it early and treating it well. This rare liver cancer in kids needs a detailed plan for diagnosis and treatment.
Definition and Epidemiology
Hepatoblastoma is a serious liver tumor that mainly hits kids under 3. It’s the top liver cancer in kids, making up about 1% of all childhood cancers. It happens in about 1.2 kids per million under 15, mostly boys.
Epidemiological studies link hepatoblastoma to certain genetic syndromes and birth defects. Kids with Beckwith-Wiedemann syndrome, FAP, and other genetic issues are at higher risk.
Risk Factors and Genetic Associations
The exact reason for hepatoblastoma is not fully known. But, some risk factors and genetic links have been found. These include:
- Genetic syndromes like Beckwith-Wiedemann and FAP
- Being born small or early
- Exposure to certain substances in the womb
Studies suggest genetic mutations play a part in hepatoblastoma. The CTNNB1 gene, which codes for β-catenin, is often mutated in these tumors.
Clinical Presentation in Children
Hepatoblastoma symptoms can differ, but common ones are:
- Abdominal swelling or distension
- Abdominal pain or discomfort
- Weight loss or loss of appetite
- Jaundice or liver dysfunction signs
Spotting hepatoblastoma early is vital for good treatment. A thorough diagnostic process, including imaging and lab tests, is needed to find and treat it.
As we learn more about hepatoblastoma, it’s clear we need a team effort for the best care. Next, we’ll look into how to diagnose and treat this tough condition.
Diagnostic Approaches for Hepatoblastoma

Diagnosing hepatoblastoma needs a detailed plan. This includes lab tests, imaging, and tumor markers. Finding this rare liver cancer early is key to treating it right.
Initial Screening and Laboratory Tests
The first step is screening and lab tests. These tests look for signs of a liver tumor.
- Complete Blood Count (CBC) to check overall health and blood cell counts.
- Liver function tests to see how well the liver works.
- Alpha-fetoprotein (AFP) levels, as high AFP is a key sign of hepatoblastoma.
Lab tests are very important at the start. They help figure out if a tumor might be there.
Imaging Techniques in Diagnosis
Imaging is key in finding hepatoblastoma. It shows the tumor’s size, where it is, and how big it is.
- Ultrasound: Often the first test, it spots liver masses and checks their details.
- Computed Tomography (CT) scans: Gives detailed pictures of the liver, showing the tumor’s size and spread.
- Magnetic Resonance Imaging (MRI): Gives clear images that help tell hepatoblastoma apart from other liver issues.
| Imaging Technique | Primary Use in Hepatoblastoma Diagnosis | Key Benefits |
| Ultrasound | First to spot liver masses | Non-invasive, quick, and easy to get |
| CT Scan | Looks at tumor size and spread | Clear images, good for staging |
| MRI | Tells hepatoblastoma apart from other issues | Great for soft tissue, no radiation |
The Role of Tumor Markers
Tumor markers, like alpha-fetoprotein (AFP), are very important in diagnosing and managing hepatoblastoma. High AFP levels often mean this tumor is present.
Watching AFP levels helps see how well treatment is working and if the tumor comes back. It’s a key part of diagnosing and following up on hepatoblastoma.
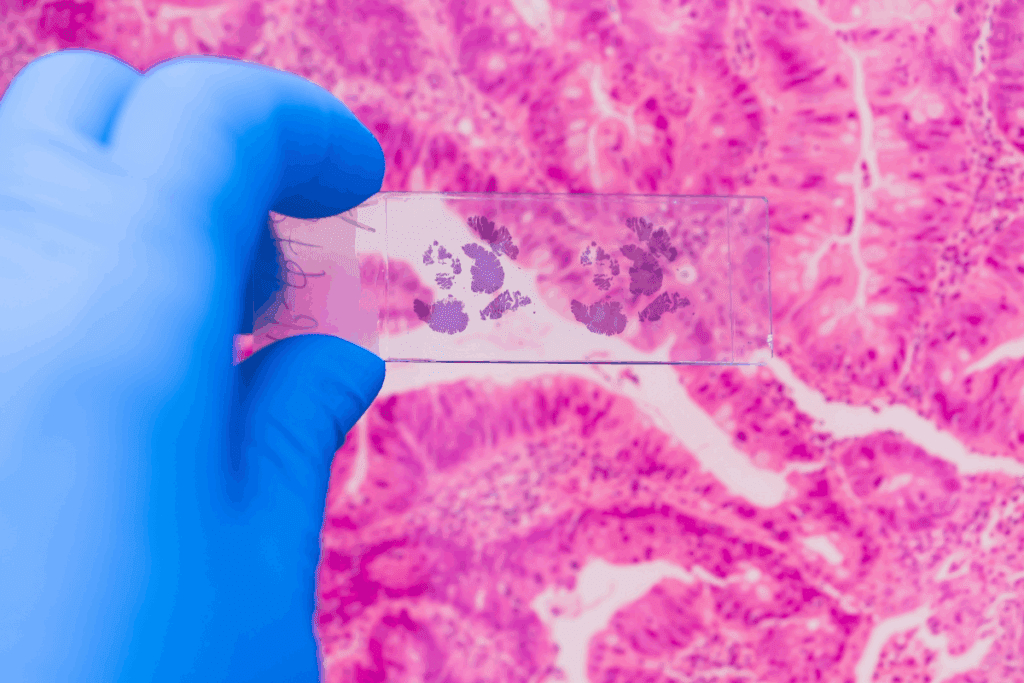
The Importance of Hepatoblastoma Biopsy in Diagnosis
Hepatoblastoma biopsy is key in finding out what treatment you need. It’s a rare liver cancer mostly found in kids. Getting it right is vital for good care. We’ll look at why getting tissue samples is important, how they help decide treatment, and when you really need a biopsy.
Why Tissue Diagnosis Matters
Getting a biopsy is the first step to confirm hepatoblastoma. It helps tell it apart from other liver issues. Accurate diagnosis is the base of good cancer care.
Also, a biopsy tells us about the tumor’s type. This info helps decide how to treat it. For example, some tumors might need stronger treatments because they grow faster.
Histological Classification and Its Impact on Treatment
The type of hepatoblastoma found through biopsy affects treatment. Different types might need different treatments. For instance, some types might have a better chance of recovery, while others might need stronger treatments.
Knowing the type helps doctors predict how the tumor will act and how it will react to treatment. This is key for making a treatment plan that works best for you.
When Biopsy Is Absolutely Necessary
There are times when a biopsy might not be needed right away. But there are cases where you really need one. This is when the diagnosis is unsure or the tumor can’t be removed right away.
In these situations, biopsy gives vital information for planning treatment. It helps avoid wrong treatments and makes sure you get the best care for your tumor and health.
Types of Biopsy Procedures for Liver Tumors in Children
There are several biopsy procedures for diagnosing liver tumors in kids. Each has its own benefits and things to consider. The right biopsy depends on the tumor’s size, location, the child’s health, and what the doctors think it might be.
Percutaneous Needle Biopsy
Percutaneous needle biopsy is a simple procedure. A thin needle goes through the skin into the tumor to get tissue samples. It’s liked for being easy and quick to recover from. It causes less damage and has fewer risks than surgery.
We use ultrasound or CT scans to guide the needle. This method is less invasive but might not always get enough tissue for detailed analysis.
Laparoscopic Biopsy
Laparoscopic biopsy uses small cuts in the belly to insert a thin tube with a camera. It also has tools to get tissue samples. This way, doctors can see the tumor and nearby tissues clearly.
- It lets doctors check if the disease has spread.
- They can also do some treatments during the same time.
Laparoscopic biopsy is a good mix of being less invasive and getting enough tissue for diagnosis.
Open Surgical Biopsy
Open surgical biopsy is more invasive. It involves a bigger cut to directly reach the tumor. It’s usually chosen when other methods can’t get a diagnosis.
It’s good for getting a big tissue sample, which is key for detailed tests. But, it takes longer to recover and has more risks than other methods.
In conclusion, picking the right biopsy for liver tumors in kids is complex. It depends on the child’s situation, the tumor, and the risks and benefits of each method. Choosing wisely helps get an accurate diagnosis, which is vital for treatment.
The Hepatoblastoma Biopsy Procedure: Step by Step
The hepatoblastoma biopsy is a key step in diagnosing liver cancer in kids. It involves several steps, from getting ready to aftercare. Knowing each step helps ensure the best care for children.
Pre-Procedure Preparation
Before the biopsy, getting ready is key. We review the child’s health history and do blood tests. We also use imaging to find the tumor.
Preparation includes:
- Reviewing the child’s medical history and current health status
- Conducting necessary laboratory tests
- Performing imaging studies to guide the biopsy
- Discussing the procedure and its implications with the family
Anesthesia Considerations in Pediatric Patients
Anesthesia is vital for kids having a biopsy. It’s tailored to the child’s age, weight, and health. Experienced professionals administer it. The use of anesthesia in pediatric patients requires a deep understanding of their unique physiological responses and the ability to manage possible complications.
The Biopsy Technique
The biopsy takes a tissue sample from the liver tumor. The method depends on the tumor’s location and the child’s health. Common methods include needle biopsy, laparoscopic biopsy, and open surgery.
| Biopsy Method | Description | Advantages |
| Percutaneous Needle Biopsy | A minimally invasive procedure using a needle to obtain tissue | Less invasive, quicker recovery |
| Laparoscopic Biopsy | A procedure using a laparoscope to visualize and sample the tumor | Direct visualization, less tissue damage |
| Open Surgical Biopsy | A surgical procedure to directly access and sample the tumor | Allows for direct access, potentially more tissue for analysis |
Post-Procedure Care
After the biopsy, careful monitoring is key. We manage pain, watch for bleeding or infection, and give clear instructions for home care.
Effective care includes:
- Pain management strategies
- Monitoring for complications such as bleeding or infection
- Providing clear instructions for post-discharge care
- Follow-up appointments to check on the child’s recovery
By following these steps, we ensure the biopsy is safe and effective. This gives us the info we need for diagnosis and treatment.
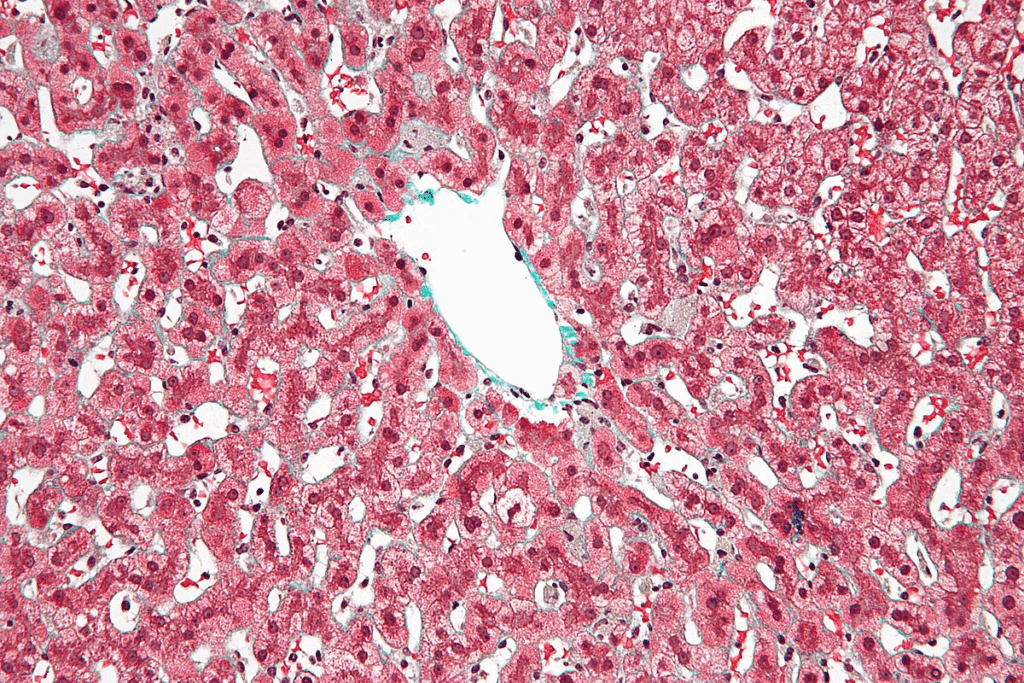
Pathological Examination of Hepatoblastoma Tissue
Looking closely at hepatoblastoma tissue is key to diagnosing and treating this rare liver cancer in kids. This step helps us understand the tumor’s characteristics. It guides how we should treat it.
Histological Subtypes and Their Significance
Hepatoblastoma has different types based on how the tumor looks under a microscope. Each type has its own traits and how well it might do in treatment. The main types are:
- Epithelial type
- Mixed epithelial and mesenchymal type
- Small cell undifferentiated type
Knowing these types is important. It helps us choose the best treatment for each child. Some types might do better with certain medicines.
Immunohistochemistry and Molecular Testing
Immunohistochemistry and molecular testing are also important. They help us:
- Find special markers in the tumor
- Learn about the tumor’s genes
- Find the right therapy for the tumor
Immunohistochemistry helps us tell hepatoblastoma apart from other tumors by looking at proteins. Molecular testing shows us genetic changes that might be treated with specific medicines.
Interpretation of Biopsy Results
Understanding biopsy results needs a lot of knowledge and skill. We look at many things, like:
- The tumor’s type
- Special markers in the tumor
- Genetic changes found by molecular testing
Getting biopsy results right is very important. It helps us make a treatment plan that fits each child’s needs.
Risks and Complications of Liver Biopsies in Children
Pediatric liver biopsies are generally safe but carry risks and complications. When we think about diagnosing hepatoblastoma, we must consider these risks. We need to weigh them against the benefits of getting a tissue diagnosis.
Bleeding and Hematoma Formation
Bleeding is a major risk with liver biopsies. The liver is full of blood vessels, making bleeding a possibility. We must be ready to handle any bleeding issues that might arise.
- Bleeding Risk Factors: Patients with bleeding problems or those on blood thinners are at higher risk.
- Management Strategies: Fixing bleeding problems before the biopsy, using ultrasound, and watching closely after.
Infection and Other Procedural Complications
Infection is a rare but possible complication. We use clean techniques and antibiotics to lower this risk.
- Infection Prevention: Keeping everything clean and using antibiotics when needed.
- Other Complications: Rare issues like bile leaks, lung problems, and damage to nearby areas.
Long-term Considerations
While immediate problems are a big worry, we also think about long-term effects. Liver biopsies in kids can lead to scarring and adhesions later on.
- Scarring and Adhesions: These can make future surgeries harder.
- Tumor Seeding: Though rare, there’s a small chance of spreading tumor cells through the biopsy site.
Knowing these risks and how to reduce them helps make liver biopsies safe for kids. This way, they remain a valuable tool in fighting pediatric cancer.
When Biopsy May Be Avoided: The PRETEXT System
The PRETEXT system offers a new way to think about when a biopsy isn’t needed for diagnosing hepatoblastoma. This system is key in figuring out how big the tumor is in the liver. It can change how doctors diagnose and treat the disease.
Understanding PRETEXT Staging
The PRETEXT system checks how much of the liver is affected by the tumor. It looks at which parts of the liver are involved. This helps doctors decide if the tumor can be removed and what treatment to use.
| PRETEXT Stage | Description |
| I | One section involved, three adjoining sections free |
| II | Two sections involved, two adjoining sections free |
| III | Three sections involved, one section free |
| IV | All four sections involved |
Cases Where Immediate Surgery May Be Preferred
In some cases, surgery might be chosen right away if the tumor looks like it can be removed. Doctors make this decision with a team, looking at the tumor’s size, where it is, and the child’s health.
The “Treat First, Biopsy Later” Approach
For some, starting treatment before getting a biopsy might be the best choice. This is when doctors are pretty sure it’s hepatoblastoma based on tests. They might start chemotherapy or other treatments first. Then, they might do a biopsy if they’re not sure after starting treatment.
Using the PRETEXT system helps doctors decide if a biopsy is really needed. This can make diagnosing hepatoblastoma in kids faster and easier.
Controversies in Hepatoblastoma Biopsy
Hepatoblastoma biopsy is a key tool in diagnosing liver cancer in kids. But, it’s not without its challenges. Debates have risen about the biopsy process.
Risk of Tumor Seeding
One big worry is tumor seeding. Tumor seeding means cancer cells could spread through the biopsy needle. This could make surgery harder.
Experts are studying how common this risk is. But, they agree it’s something to think about when choosing a biopsy. Using new imaging and precise biopsy methods can help lower this risk.
Sampling Error Concerns
Another issue is sampling error. Liver tumors can be different in different parts. So, the biopsy might not always show the whole picture. Sampling error can lead to wrong or incomplete diagnoses, affecting treatment plans.
To avoid this, multiple core biopsies are often suggested. Using imaging during the biopsy can also help get a better sample.
Debate on Timing: Pre-treatment vs. Post-resection
When to do a biopsy is also debated. Some say before treatment to guide it. Others think after surgery gives better info for follow-up treatment.
“The decision on when to perform a biopsy must be made on a case-by-case basis, taking into account the individual patient’s condition and the specific characteristics of the tumor,” according to a recent clinical guideline.
Each case is different. We must consider the tumor’s size, location, and the patient’s health. The PRETEXT staging system is also important in making these decisions.
In summary, the debates around hepatoblastoma biopsy show how complex diagnosing and treating this cancer is. Understanding these issues helps us improve care for our young patients.
Alternatives to Traditional Biopsy
We’re exploring new ways to diagnose pediatric liver tumors, moving away from old biopsy methods. We’re looking for ways to be more precise and less invasive. This search has led us to new alternatives to traditional biopsy.
Liquid Biopsy and Circulating Tumor DNA
Liquid biopsy is a new tool that analyzes blood for tumor DNA. It’s a non-invasive way to find and track liver cancer. This method is safer and lets us check on the disease more often.
- Detects genetic changes linked to hepatoblastoma
- Helps track how well treatments are working
- May spot cancer coming back early
Advanced Imaging as a Diagnostic Tool
Technologies like MRI and CT scans are key in finding liver tumors. They give us detailed info on tumor size and location. These advances have made diagnosing more accurate.
| Imaging Technique | Advantages |
| MRI | Shows soft tissues well, no radiation |
| CT Scan | Fast and detailed images |
Emerging Non-invasive Techniques
New, non-invasive methods are being studied for liver cancer diagnosis. These include:
- Urine-based biomarkers
- Volatile organic compounds (VOCs) analysis
- Advanced ultrasound techniques
These new methods are a big step towards safer, friendlier diagnosis. As research goes on, we’ll see more progress in treating pediatric liver tumors.
International Guidelines and Protocols for Hepatoblastoma Diagnosis
Diagnosing hepatoblastoma needs a detailed plan, following international rules. These rules help make sure kids get the best care possible. This improves their chances of beating this rare liver cancer.
SIOPEL Approach
The SIOPEL (International Society of Paediatric Oncology Epithelial Liver Tumor Study Group) method is key in treating hepatoblastoma. It stresses the need for accurate staging and risk grouping. This helps doctors choose the right treatment plan.
PRETEXT staging uses imaging to see how big the tumor is and where it is in the liver. This info is key for planning treatment. SIOPEL also points out how important chemotherapy is in treating this cancer, often used with surgery.
COG Guidelines
The Children’s Oncology Group (COG) has its own set of rules for treating hepatoblastoma in North America. COG’s approach involves surgery, chemotherapy, and sometimes radiation. They also stress the need for a precise diagnosis, often through biopsy.
Biopsy is very important in COG’s protocols. It helps doctors understand the cancer better and decide on the best treatment. COG’s work has helped a lot in treating this cancer.
JPLT Protocol
The Japanese Pediatric Liver Tumor Study Group (JPLT) also has its own guidelines for treating hepatoblastoma. JPLT has worked on making treatment plans better, including using chemotherapy and surgery. They also focus on PRETEXT staging and risk grouping.
Though SIOPEL, COG, and JPLT have some differences, they all aim to help kids with hepatoblastoma. By setting standards for diagnosis and treatment, they help doctors work together better. This leads to better care for this rare disease.
Case Studies: When Biopsy Changed the Treatment Course
Many case studies show how biopsy results can change treatment plans for hepatoblastoma patients. It’s not just a test; it’s key to deciding how to treat the disease.
Unexpected Histological Findings
In some cases, biopsy results were different from what tests and images showed. For example, a biopsy might find a mix of epithelial and mesenchymal types of hepatoblastoma. This can greatly affect treatment choices.
Case Study 1: A 2-year-old had a liver tumor. Tests thought it was a common type of hepatoblastoma. But the biopsy found a rare, high-risk type. This led to stronger treatment, like more chemotherapy and watching for cancer spread.
Distinguishing Hepatoblastoma from Other Liver Tumors
Biopsy is key in telling apart hepatoblastoma from other liver tumors. Getting the right diagnosis is vital for choosing the right treatment.
| Tumor Type | Typical Age Group | Common Treatment Approach |
| Hepatoblastoma | Infants and young children | Surgery and chemotherapy |
| Hepatocellular Carcinoma | Older children and adults | Surgery, chemotherapy, and targeted therapy |
| Benign Liver Tumors | Variable | Observation or surgical resection |
Impact on Treatment Strategy and Outcomes
Biopsy results help not just in diagnosing but also in planning treatment. Knowing the tumor’s details lets doctors tailor care to each patient.
Case Study 2: A biopsy showed a high-risk tumor in a patient. This led to stronger chemotherapy, which helped the patient a lot.
These stories highlight how vital biopsy is in treating hepatoblastoma. It gives doctors the info they need to make better choices, helping patients more.
Conclusion: The Future of Hepatoblastoma Diagnosis
Looking ahead, we see big changes in diagnosing hepatoblastoma. New ways to test and treat will help kids with this rare liver cancer. The biopsy will keep being key to making the right diagnosis and treatment plans.
New tech like liquid biopsy and better imaging are on the horizon. They might make diagnosing and treating liver tumors in kids even better. But, the biopsy will always be important for liver cancer diagnosis.
We expect better results for patients with these new tools and strategies. Working together, researchers, doctors, and global groups will shape the future of treating hepatoblastoma.
FAQ
What is hepatoblastoma and why is biopsy important for its diagnosis?
Hepatoblastoma is a rare liver cancer found mainly in children. A biopsy is key for diagnosing it. It helps confirm the tumor type and guides treatment.
What are the different types of biopsy procedures used for diagnosing liver tumors in children?
There are three main biopsy types: percutaneous needle biopsy, laparoscopic biopsy, and open surgical biopsy. Each is chosen based on the tumor and the child’s health.
What are the risks associated with liver biopsies in children?
Risks include bleeding, infection, and long-term issues. But, these risks are low when done by skilled doctors.
How is the pathological examination of hepatoblastoma tissue performed?
The tissue is analyzed for tumor types. Techniques like immunohistochemistry and molecular testing provide detailed tumor information.
Are there alternatives to traditional biopsy for diagnosing hepatoblastoma?
Yes, alternatives include liquid biopsy and advanced imaging. These methods are being studied for accurate diagnoses without invasive procedures.
What international guidelines are followed for hepatoblastoma diagnosis?
Guidelines from SIOPEL, COG, and JPLT are followed. They help standardize diagnosis and treatment.
Can biopsy change the treatment course for hepatoblastoma?
Yes, biopsy results can change treatment plans. Unexpected findings can lead to better treatment strategies.
What is the PRETEXT staging system, and how does it relate to biopsy?
The PRETEXT staging system assesses liver tumor extent. Sometimes, biopsy is skipped for immediate surgery or a “treat first” approach.
What are the controversies surrounding hepatoblastoma biopsy?
Debates include concerns about tumor seeding and sampling errors. There’s also debate on the best biopsy timing.
How is the future of hepatoblastoma diagnosis evolving?
The future may see more non-invasive diagnostics and precise molecular tests. These could reduce the need for traditional biopsies.
References:
- Djouder, N., & Rigual, M. del Mar. (2025). Macrophages harness hepatocyte glutamate to boost liver regeneration. Nature.





