Last Updated on October 20, 2025 by
Hepatoblastoma is a rare liver cancer that mainly affects kids under 3. It’s the top liver cancer in kids, making up 50% to 60% of all cases.
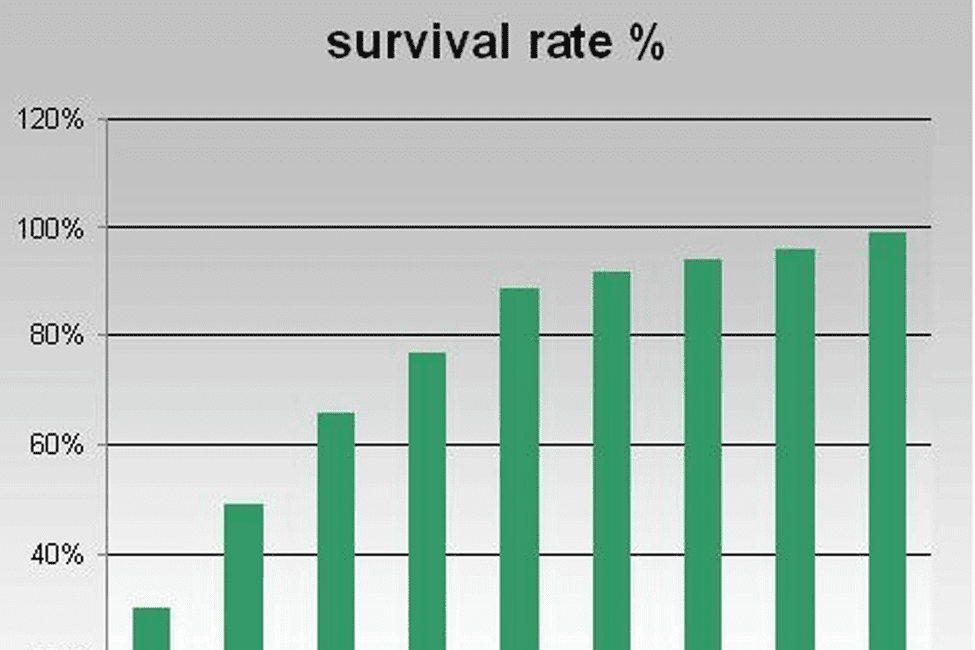
The 5-year survival rate for hepatoblastoma has gotten much better. Now, the 5-year survival rate is 80% to over 90% for those with localized disease.
Thanks to better treatments and catching it early, survival rates are going up. Knowing these numbers is key for patients, families, and doctors everywhere.
Hepatoblastoma is a rare liver cancer that mainly hits young kids. It’s a big worry for kids’ health. We need to know what it is, how common it is, its signs, risk factors, and causes.
Hepatoblastoma is a liver tumor that mostly happens in babies and toddlers. It’s the top liver cancer in kids, but it’s rare. It’s hard to know how common it is because it’s so rare. But, it’s thought to affect about 1 in 1 million kids under 15.
The first signs of hepatoblastoma can be hard to spot. This makes finding it early tough. Common signs include:
These signs can mean many things. So, it’s important to get a full check-up from a doctor.
We don’t know all about what causes hepatoblastoma. But, we do know some things that might increase the risk. These include:
Studies say that genes and the environment might play a part. More research is needed to understand how it starts and grows.
Knowing about hepatoblastoma is key for catching it early and treating it well. Survival depends on finding it early, the stage it’s in, and getting the right care. We’ll look into these more in the next parts.
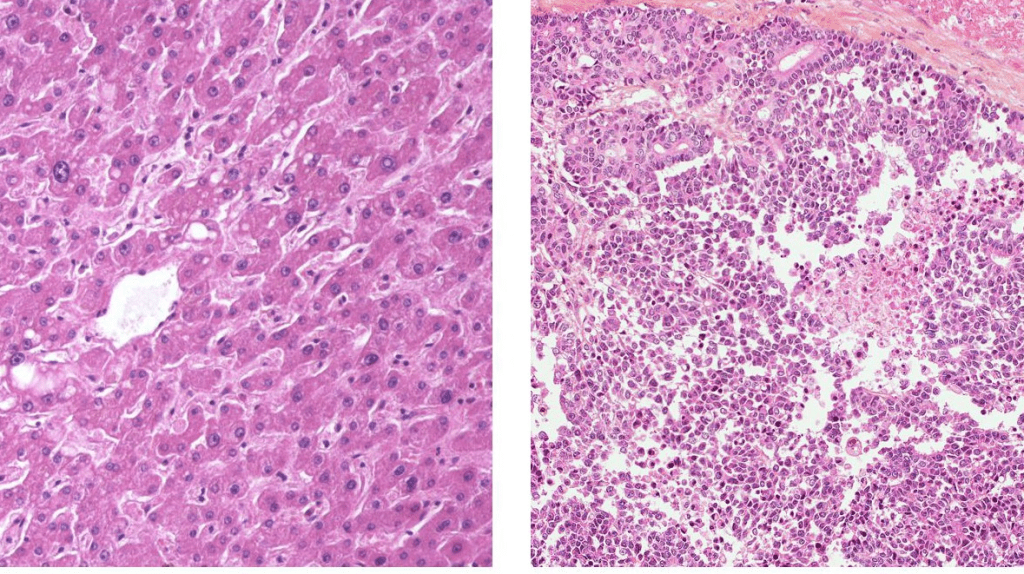
Diagnosing hepatoblastoma uses imaging and blood tests. Early detection is key to better survival chances. It means treatment can start sooner.
Imaging tests like ultrasound, CT, and MRI are main tools. They show the tumor’s size, where it is, and how far it has spread.
Serum alpha-fetoprotein (AFP) testing is also vital. High AFP levels often mean hepatoblastoma. It helps in diagnosing and checking how well treatment works.

Finding hepatoblastoma early greatly helps patients. Early treatment can stop the tumor from growing and spreading.
Regular check-ups and screenings are important, mainly for those at high risk. Timely diagnosis lets doctors plan better treatment. This boosts survival chances.
Using advanced tests and focusing on early detection can raise survival rates for hepatoblastoma patients.
Hepatoblastoma staging systems help doctors understand how far the disease has spread. This is key in deciding the best treatment plan. The stage of the disease also affects how well a patient might do.
The PRETEXT staging system is a common way to check how much of the liver is affected by the tumor. It looks at the liver in four parts and how much of it has cancer. This helps doctors figure out if surgery is possible and what treatment to use.
The PRETEXT system checks the liver’s four sections and how much cancer is there. It tells doctors about the tumor’s size and where it is. This is important for deciding if surgery can remove the tumor.
This system helps doctors decide if surgery is an option. It also tells them if other treatments, like chemotherapy, are needed.

There are other ways to classify hepatoblastoma too. These include the Children’s Hepatic tumors Strategy Group (CHT-SG) and the International Childhood Liver Tumor Strategy Group (SIOPEL). These systems look at the tumor’s type, the patient’s age, and how well the tumor responds to treatment. They give a more detailed view of the disease.
By using these different systems together, doctors can get a clearer picture of the disease. This helps them make better treatment plans. It also improves the chances of a good outcome for the patient.
Hepatoblastoma, a rare liver cancer in kids, has seen better survival rates in recent years. Thanks to new treatments like surgery, chemotherapy, and liver transplants, more kids are living longer. This is a big step forward for those facing this disease.

The 5-year survival rate for hepatoblastoma has greatly improved. Studies show that kids with localized hepatoblastoma now have a 80-90% chance of survival. This shows how early detection and new treatments are making a difference.
“The rise in survival rates is thanks to global research and better treatments,” says a top pediatric oncologist. Working together has helped us understand and treat the disease better, leading to better outcomes for patients.
Back in the day, the outlook for hepatoblastoma was much worse. But over the years, survival rates have gone up. This is thanks to better surgery, chemotherapy, and the use of liver transplants in some cases.
New international trials and better ways to classify the disease have also helped. By finding the best treatments for each child, doctors can improve their chances of survival.
As we learn more about treating hepatoblastoma, it’s key to keep working together. This means using all kinds of treatments and supporting the whole child and their family.
The stage of hepatoblastoma at diagnosis is key to a child’s survival chances. The disease stage affects the treatment plan and the patient’s outlook.
Children with localized hepatoblastoma have a good chance of survival. Their survival rates are 80% to 90%. Early detection and proper treatment are important for these positive results.
For advanced or metastatic hepatoblastoma, survival rates are lower. They range from 50% to 70%. This stage requires aggressive and complex treatments.
Relapse in patients is a tough situation. The 5-year survival rate for recurrent or metastatic hepatoblastoma is a concern. It highlights the need for better treatment options.
Every patient’s case is different. Survival rates can change based on many factors. These include the treatment’s success and the patient’s health.
Advances in treatment have greatly improved survival chances for patients with hepatoblastoma. This liver cancer is common in children. A mix of treatments is needed for the best results.
Surgery is key in treating hepatoblastoma. It’s the only way to cure it. Complete surgical resection is essential. New surgical methods have made it easier to perform successful surgeries.
Surgery is not just for the first treatment. It also helps with relapses and leftover disease. Doctors and surgeons work together to plan the best surgery timing.
Chemotherapy is important in treating hepatoblastoma. It helps shrink tumors before surgery. Neoadjuvant chemotherapy is key in treating tumors that can’t be removed at first.
There are many chemotherapy plans, based on the tumor’s stage, the patient’s age, and other factors. International studies have helped make these treatments better.
Liver transplantation is an option for patients with tumors that can’t be removed or come back. It offers a chance of cure for those with poor outlooks.
Choosing liver transplantation involves a detailed check-up. This includes looking at the patient’s health and the success of the transplant. Better care after the transplant has led to better survival rates.
In summary, treating hepatoblastoma is complex. It needs a mix of surgery, chemotherapy, and sometimes liver transplantation. The right treatment plan is key to good outcomes. Ongoing research aims to make these treatments even better.
Knowing what affects hepatoblastoma prognosis is key for good treatment plans. This rare liver cancer mainly hits kids. Thanks to better treatments, survival rates have gone up. But, the outcome depends on several important factors.
The type of tumor is a big factor in hepatoblastoma prognosis. Genetic markers and the tumor’s look really matter. Some genetic changes can make the tumor grow faster or respond better to treatment. High levels of alpha-fetoprotein (AFP) at first can mean a tougher disease. But, if AFP goes down while treating, it’s a good sign.
When a child gets diagnosed and their health matters a lot. Younger kids usually do better than older ones. The child’s overall health and any other health issues can affect how well they do with treatment.
How well a child responds to treatment is very important. Removing the tumor completely is a big step towards survival. How well the child does with chemotherapy and sticks to the treatment plan also plays a big role. New surgery methods and better chemotherapy have helped more kids survive.
Getting care from a team of experts is vital for better outcomes. A team of pediatric surgeons, oncologists, and others work together. They make sure each child gets the best care, which helps them live longer.
By focusing on these factors, doctors can make treatment plans that work better. This helps kids with hepatoblastoma have a better chance of survival.
Medical research and teamwork have greatly improved survival chances for kids with hepatoblastoma. This progress comes from the hard work of researchers, doctors, and global organizations. They work together to make treatments better and more effective.
International trials are key to better hepatoblastoma treatments. These trials combine data and resources. This helps researchers find the best ways to treat the disease.
The International Childhood Liver Tumours Strategy Group (SIOPEL) leads global efforts. They aim to improve treatment results for kids with hepatoblastoma.
These trials have led to better treatment plans. Plans that fit each patient’s needs based on their risk level. This means patients get the latest and best treatments.
There’s been a big leap in how we figure out the risk of hepatoblastoma. Knowing the risk helps doctors choose the right treatment. This makes sure patients get the best chance of being cured without too much harm.
New imaging, biology, and genetics help us better understand tumors. This lets doctors put patients into risk groups more accurately. This way, treatments can be more focused, helping both low-risk and high-risk patients.
New treatments that target specific parts of the tumor are exciting. As we learn more about hepatoblastoma, we can make treatments that are more precise. This means less harm to healthy cells.
Research into these new treatments is ongoing. Many promising options are being tested. This shows the power of ongoing research and teamwork in fighting hepatoblastoma cancer.
Hepatoblastoma, a rare liver cancer in kids, has seen big improvements in treatment and survival rates. Early detection and a team approach have made a big difference. Ongoing research keeps pushing these gains forward.
Places like those on livhospital.com are key in this fight. They use the latest treatments and care to help kids. By focusing on how to improve survival rates, we can make treatments better.
Research is always finding new ways to fight hepatoblastoma. We’re dedicated to giving each patient the best care possible. Together, we can make a big difference in the lives of kids with this disease.
Hepatoblastoma is a rare liver cancer found mainly in kids under 3. It starts in liver cells.
Symptoms include belly pain, a mass in the belly, and weight loss. Finding it early is key to better treatment.
Doctors use ultrasound, CT scans, and MRI to find it. They also check alpha-fetoprotein levels in the blood. These tests help plan treatment.
The PRETEXT system divides the liver into four parts to check tumor spread. It helps decide if surgery is possible.
Kids with localized disease have a 5-year survival rate of 80% to over 90%. Survival rates depend on the disease stage.
Early-stage disease has much better survival rates than advanced disease. Quick treatment is vital for better chances.
Treatments include surgery, chemotherapy, and liver transplant. The best option depends on the disease and the patient.
Prognosis depends on tumor type, patient health, treatment response, and access to care. Knowing these factors helps plan better treatment.
Advances include global trials, better risk assessment, and new treatments. These steps have raised survival rates.
Early detection leads to better treatment and survival. It allows for timely action before the disease grows.
Multidisciplinary care ensures a complete treatment plan. It improves survival by addressing all patient needs.
Surgery is key, but often, a mix of treatments is needed. This includes chemotherapy and sometimes liver transplant, based on the disease stage.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!