
We are dedicated to top-notch healthcare for international patients. Hepatoblastoma is a rare liver cancer and the most common tumor in kids. It’s often connected to genetic syndromes, with Beckwith-Wiedemann syndrome being a key example.
It’s vital to understand how genetic conditions link to hepatoblastoma. This knowledge helps in early detection and treatment. We’ll look into how certain genetic syndromes raise liver cancer risk. Also, why it’s key to screen kids with these conditions.
Key Takeaways
- Hepatoblastoma is the most common liver cancer in children.
- Beckwith-Wiedemann syndrome is strongly associated with an increased risk of hepatoblastoma.
- Early detection is critical for improving outcomes in children with hepatoblastoma.
- Genetic syndromes play a significant role in the development of liver cancer in young children.
- Screening is essential for children with genetic conditions that increase the risk of hepatoblastoma.
Understanding Hepatoblastoma: A Rare Pediatric Liver Cancer
It’s important to know about hepatoblastoma to catch it early. This rare liver cancer mainly affects kids. We’ll look into what it is, how it’s classified, and the types it can take.
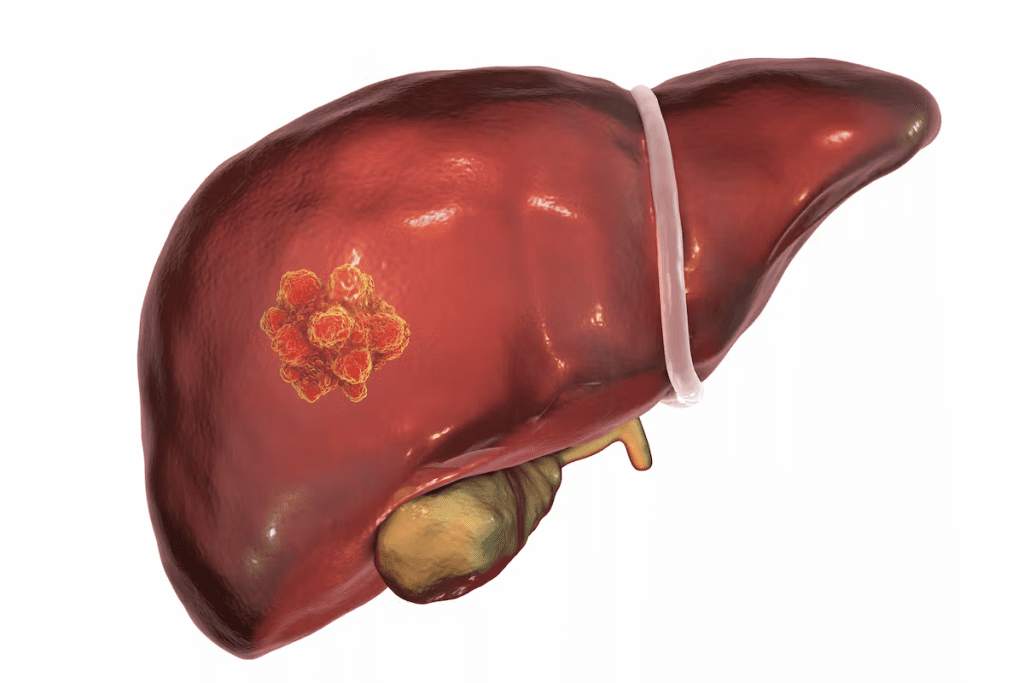
Definition and Classification of Hepatoblastoma
Hepatoblastoma is a cancer that starts in the liver and mostly hits kids under 3. It’s divided into types based on how the cells look. This helps doctors know how aggressive it is and what treatment to use.
Theclassification of hepatoblastoma is key for figuring out the treatment and how well a patient might do. It’s mainly split into epithelial and mixed types, with more specific subtypes based on cell details.
Histological Types and Their Significance
The different types of hepatoblastoma are important. They tell us how the tumor will act and how well it might respond to treatment. The main types are:
- Epithelial Type: This includes fetal, embryonal, macrotrabecular, and small cell undifferentiated subtypes.
- Mixed Epithelial-Mesenchymal Type: This has both epithelial and mesenchymal parts, sometimes with teratoid features.
Knowing these types is vital for creating effective treatment plans. It helps doctors understand how aggressive the tumor is and how it might react to treatment.
Beckwith-Wiedemann Syndrome: The Primary Genetic Link
Children with Beckwith-Wiedemann Syndrome have a higher risk of liver cancer, called hepatoblastoma. This genetic disorder causes overgrowth and an increased risk of tumors, including liver cancer.
Molecular Basis
The genetic changes in Beckwith-Wiedemann Syndrome affect chromosome 11p15.5. This area controls growth and is affected by genomic imprinting. Genetic changes here can cause too much growth and not enough tumor control, leading to tumors like hepatoblastoma.
Clinical Features and Presentation
Beckwith-Wiedemann Syndrome is marked by large birth weight, big tongue, and belly wall defects. Children with this syndrome are at high risk for tumors, with liver cancer being a big worry. Spotting the syndrome early is key to managing and preventing tumors.
The 1,000-10,000 Times Increased Risk Factor
Children with Beckwith-Wiedemann Syndrome face a 1,000 to 10,000 times higher risk of liver cancer than others. This highlights the need for careful monitoring and early detection of liver cancer. Regular checks with ultrasound and alpha-fetoprotein tests are advised to catch liver cancer early.
Other Genetic Syndromes Associated with Hepatoblastoma
Many genetic conditions, aside from Beckwith-Wiedemann Syndrome, raise the risk of hepatoblastoma. We’ll look at these syndromes and how they affect liver cancer risk.
Familial Adenomatous Polyposis (FAP)
Familial Adenomatous Polyposis (FAP) causes many polyps in the colon and rectum. FAP increases the risk of cancers, including hepatoblastoma. The APC gene mutation in FAP can also lead to liver tumors.
Children with FAP are at higher risk of hepatoblastoma. This highlights the need for early screening and monitoring.
Simpson-Golabi-Behmel Syndrome
Simpson-Golabi-Behmel Syndrome is a rare genetic disorder that affects many organs and causes overgrowth. It’s linked to an increased risk of tumors, including hepatoblastoma. The GPC3 gene mutation often causes this condition.
Early diagnosis and management are key to reducing cancer risk.
Trisomy 18 and Hepatoblastoma Risk
Trisomy 18, or Edwards syndrome, is a chromosomal disorder with an extra chromosome 18. While most with Trisomy 18 don’t survive infancy, those who do may face a higher cancer risk, including hepatoblastoma. The genetic imbalance from Trisomy 18 can lead to tumors.

In conclusion, several genetic syndromes, aside from Beckwith-Wiedemann Syndrome, increase the risk of hepatoblastoma. Knowing about these syndromes is key for early liver cancer detection and management in children.
Epidemiology of Hepatoblastoma in Children
Understanding hepatoblastoma’s spread is key to finding risk factors and better care for kids. It’s a rare liver cancer mainly hitting young children.
Age Distribution and Incidence Rates
Hepatoblastoma mostly hits kids under four, with most cases in the first 18 months. In the U.S., it affects about 1.2 to 1.5 kids per million each year. The rates have stayed mostly the same, with a slight rise in some studies.
The age when kids get hepatoblastoma is very important. Children under one year have the highest rates, with rates dropping after four. This shows it’s linked to genetics and before birth.
Geographic and Demographic Patterns
Where kids live and who they are also affects hepatoblastoma rates. Some studies show Asian kids might get it more often than others.
Being born small or early increases the risk. Also, boys get it more than girls, but why isn’t clear.
In short, hepatoblastoma mainly hits young kids, with certain groups at higher risk. Knowing this helps us create better screening and treatment plans.
- Hepatoblastoma mainly affects children under four years old.
- The incidence rate is about 1.2 to 1.5 cases per million children per year.
- Low birth weight and prematurity increase the risk.
- Males are more commonly affected than females.
Genetic Mechanisms Behind Syndrome-Associated Hepatoblastoma
It’s important to understand the genetics of hepatoblastoma, a rare liver cancer in kids. This cancer is linked to certain genetic syndromes. It’s caused by changes in genes that control cell growth and tumor formation.
The Role of Imprinting Disorders
Imprinting disorders, like Beckwith-Wiedemann Syndrome (BWS), raise the risk of hepatoblastoma. BWS affects chromosome 11p15.5, causing genes to grow too much and others to stop working. This imbalance makes kids more likely to get tumors, including hepatoblastoma.
Key factors in imprinting disorders include:
- Loss of imprinting (LOI) leading to the biallelic expression of genes
- Epigenetic changes affecting gene expression
- Increased susceptibility to tumor development
Tumor Suppressor Genes and Oncogenes
Tumor suppressor genes and oncogenes control cell growth. Changes in these genes can cause cells to grow out of control, leading to tumors. In hepatoblastoma, specific genes are often mutated or not working right.
Notable examples include:
- The CTNNB1 gene, which makes β-catenin, is often changed in hepatoblastoma.
- TP53, a gene that helps control cell growth and death, is also involved.
As scientists learn more about hepatoblastoma’s genetics, it’s clear why early testing is key. Finding the cancer early can greatly improve treatment chances for kids.
Clinical Presentation and Diagnostic Challenges
Hepatoblastoma is hard to diagnose early because its symptoms are not clear. Kids with this rare liver cancer often show signs that look like other stomach problems.
Common Symptoms and Physical Findings
Hepatoblastoma shows up as a swelling in the belly. Common symptoms include belly pain, loss of appetite, and weight loss. Some kids might also show signs of early puberty because of the tumor’s hormone release.
A doctor might find a mass in the right upper belly area. Studies show most kids with this cancer have a mass they can feel.
In serious cases, the tumor can make the belly very big. This can cause breathing problems or other serious issues. Doctors need to think of hepatoblastoma when they see a belly mass in a child.
Differential Diagnosis Considerations
When trying to figure out what’s wrong, doctors look at other liver cancers and non-cancerous growths. A detailed test is needed to correctly identify hepatoblastoma and rule out other problems.
A top doctor says, “You need to be very careful to spot hepatoblastoma early. Its symptoms can be confusing and look like other belly issues.”
It’s hard to tell if it’s hepatoblastoma or something else, and how far it has spread. Tests like ultrasound, CT, and MRI are key. They help see how big the tumor is, where it is, and if it has spread.
Screening Protocols for High-Risk Children
Children with certain genetic syndromes face a higher risk of hepatoblastoma. They need specific screening protocols. Regular screening helps catch the disease early, leading to better treatment options.
Recommended Screening Guidelines by Syndrome
Genetic syndromes vary in their risk for hepatoblastoma. For example, kids with Beckwith-Wiedemann Syndrome (BWS) are at a higher risk. They need more careful screening.
The guidelines for screening include:
- Regular abdominal ultrasounds to check for liver issues.
- Testing for alpha-fetoprotein (AFP) levels, as high levels can signal hepatoblastoma.
Children with Familial Adenomatous Polyposis (FAP) also face a higher risk. The screening plan might differ slightly. It’s key for doctors and caregivers to team up with geneticists to set the right screening schedule.
Imaging and Laboratory Testing Approaches
Imaging is vital in the screening process. Abdominal ultrasound is the first choice because it’s non-invasive and doesn’t use radiation. It’s great for spotting liver tumors and tracking their size.
Laboratory tests, like checking alpha-fetoprotein (AFP) levels, are also key. High AFP levels might mean a tumor is present. But, not all tumors show up in AFP tests.
We stress the need for a multi-modal screening approach. This combines imaging and lab tests for thorough monitoring of high-risk kids. Such a strategy boosts early detection and improves treatment results for these children.
Treatment Approaches for Syndrome-Associated Hepatoblastoma
Treating hepatoblastoma linked to genetic syndromes needs a detailed plan. We’ll look at different treatments like surgery, chemotherapy, and liver transplant for advanced cases.
Surgical Management Options
Surgery is key in treating hepatoblastoma, aiming to remove the tumor fully. Surgery is often the first step if the tumor is small and can be safely taken out. We look at the tumor’s size, where it is, and the child’s health when planning surgery.
If the tumor is too big or in a tricky spot, neoadjuvant chemotherapy might be used first. This helps make the tumor smaller and easier to remove, improving chances of success.
Chemotherapy Protocols and Considerations
Chemotherapy is vital for treating hepatoblastoma, mainly for tumors that can’t be removed or have spread. Cisplatin-based chemotherapy is commonly used, often with doxorubicin.
We adjust chemotherapy plans for each child based on the tumor type, stage, and how they react to treatment. Watching for side effects and changing the treatment if needed helps avoid long-term harm.
Liver Transplantation in Advanced Cases
Liver transplant is an option for kids with big tumors that can’t be removed and haven’t gotten better with chemotherapy. Liver transplant can be a cure for these tough cases.
We check if a child is a good candidate for a transplant, looking at extrahepatic disease and overall health. Post-transplant chemotherapy might be used to stop the tumor from coming back.
By using these treatments together, we can help more kids with syndrome-associated hepatoblastoma. A team of experts is key in managing these complex cases, making sure each child gets the best care.
Prognosis and Long-term Outcomes
Hepatoblastoma is a rare liver cancer in kids. Its prognosis depends on several key factors. Knowing these factors helps families and doctors make better treatment plans.
Survival Rates and Prognostic Factors
Thanks to new treatments, more kids with hepatoblastoma are surviving. Studies show that over 80% of kids can now beat this cancer(PMC6895795). But, the outcome depends on several factors.
These include the cancer’s stage, the child’s age, and any genetic syndromes. Kids diagnosed early and who are younger usually do better. Certain genetic conditions, like Beckwith-Wiedemann Syndrome, also affect the prognosis.
Long-term Monitoring and Follow-up Care
After treatment, kids with hepatoblastoma need ongoing care. Regular check-ups help catch any signs of cancer coming back. A team of doctors, including oncologists and surgeons, is involved in this care.
The type and frequency of follow-up care vary. But, it usually includes imaging and lab tests. Catching cancer early is key to successful treatment.
It’s vital to have a detailed follow-up plan. This plan should watch for cancer return and also for any long-term effects of treatment. This includes checking for developmental delays or secondary cancers.
Recent Advances in Research and Treatment
The treatment for hepatoblastoma is changing fast. This is thanks to new targeted therapies and precision medicine. Researchers are now focusing on more personalized and effective ways to treat this rare liver cancer in kids.
Targeted Therapies and Precision Medicine
Targeted therapies are a big step forward in treating hepatoblastoma. They aim to kill cancer cells without harming healthy tissues. This is different from traditional chemotherapy, which can harm both.
“The development of targeted therapies has opened up new avenues for treating hepatoblastoma, promising better results with fewer side effects,”
Precision medicine goes even further. It tailors treatment based on each patient’s tumor genetics. By studying a tumor’s genetics, we can find the best treatment for it.
Emerging Clinical Trials and Studies
Many clinical trials are working on new ways to treat hepatoblastoma. These studies help us understand the disease better and find better treatments. For example, some trials are looking into immunotherapy, which uses the immune system to fight cancer.
Other research is about finding biomarkers. These biomarkers help predict which treatments will work best for each patient. This is key for making treatment plans that are just right for each child.
Key areas of research include:
- Developing more effective targeted therapies
- Improving our understanding of hepatoblastoma genetics
- Exploring the role of immunotherapy in treatment
- Identifying biomarkers for personalized medicine approaches
We’re getting better at treating hepatoblastoma, thanks to ongoing research. The future looks bright, with new treatments and therapies giving us hope for better outcomes.
Conclusion: The Importance of Genetic Awareness in Pediatric Liver Cancer
Genetic awareness is key in finding and treating hepatoblastoma in kids with genetic syndromes. We’ve learned that some genetic conditions, like Beckwith-Wiedemann Syndrome, raise the risk of liver cancer.
As we learn more about the genes behind hepatoblastoma, it’s clear that knowing about genetics is vital. It helps us find liver cancer early in kids at risk. This means we can treat it better when it’s smaller.
We’ve talked about how to tackle pediatric liver cancer. This includes genetic tests, imaging, and lab work. Using these methods together helps us diagnose and treat hepatoblastoma better.
Our research keeps showing us new things about hepatoblastoma’s genetics. We’re dedicated to top-notch healthcare for all patients, including those from abroad. By spreading the word about genetic awareness and studying liver cancer, we aim to make a difference in kids’ lives.
FAQ
What is hepatoblastoma and how is it related to genetic syndromes?
Hepatoblastoma is a rare liver cancer found mainly in children. It’s linked to genetic syndromes like Beckwith-Wiedemann and Familial Adenomatous Polyposis (FAP).
What are the common symptoms of hepatoblastoma?
Symptoms include an enlarged belly, weight loss, and loss of appetite. Some kids might also feel jaundice or get tired easily.
How is hepatoblastoma diagnosed?
Doctors use imaging tests like ultrasound and CT scans to find it. Blood tests for alpha-fetoprotein (AFP) and liver function tests are also key. A biopsy might be needed to confirm it.
What is the significance of Beckwith-Wiedemann syndrome in hepatoblastoma?
This genetic disorder greatly raises the risk of getting hepatoblastoma. The risk is 1,000- to 10,000-fold higher than in the general population.
What are the treatment options for hepatoblastoma?
Treatment involves surgery, chemotherapy, and sometimes liver transplant. The plan depends on how far the cancer has spread.
What is the prognosis for children with hepatoblastoma?
The outlook varies based on the cancer’s stage and how well it responds to treatment. Early-stage cases often have better survival rates.
How can children with genetic syndromes be screened for hepatoblastoma?
Regular imaging tests and blood tests for AFP are recommended. This is for kids with syndromes that raise their risk.
What is the role of genetic testing in hepatoblastoma?
Genetic tests can spot syndromes that increase the risk of hepatoblastoma. This helps with early detection and monitoring.
What are the latest developments in hepatoblastoma research and treatment?
New research includes targeted therapies and precision medicine. Clinical trials are also exploring new treatment options.
What is the survival rate for liver cancer, specific to hepatoblastoma, by age?
Survival rates vary by age and cancer stage. Younger children generally have a better chance of recovery.
What is a hepatic tumor or mass on the liver?
It’s an abnormal growth or lesion in the liver. This can be benign or cancerous, like hepatoblastoma.
What is the definition of a lesion on the liver?
A liver lesion is any abnormal area or damage in the liver tissue. It can be caused by tumors, cysts, or inflammation.
What is hepatoblastoma prognosis, and what factors influence it?
The prognosis depends on the cancer stage, treatment response, and any genetic conditions.
References
Klein, S. D., et al. (2023). Occurrence of hepatoblastomas in patients with Beckwith“Wiedemann syndrome. Clinical Epigenetics, 15, Article 99. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10177446/
Zhu, L., et al. (2022). Epigenetics and genetics of hepatoblastoma in Beckwith-Wiedemann Syndrome. Frontiers in Genetics, 13, 1070971. https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.1070971/full


































