Last Updated on November 4, 2025 by mcelik

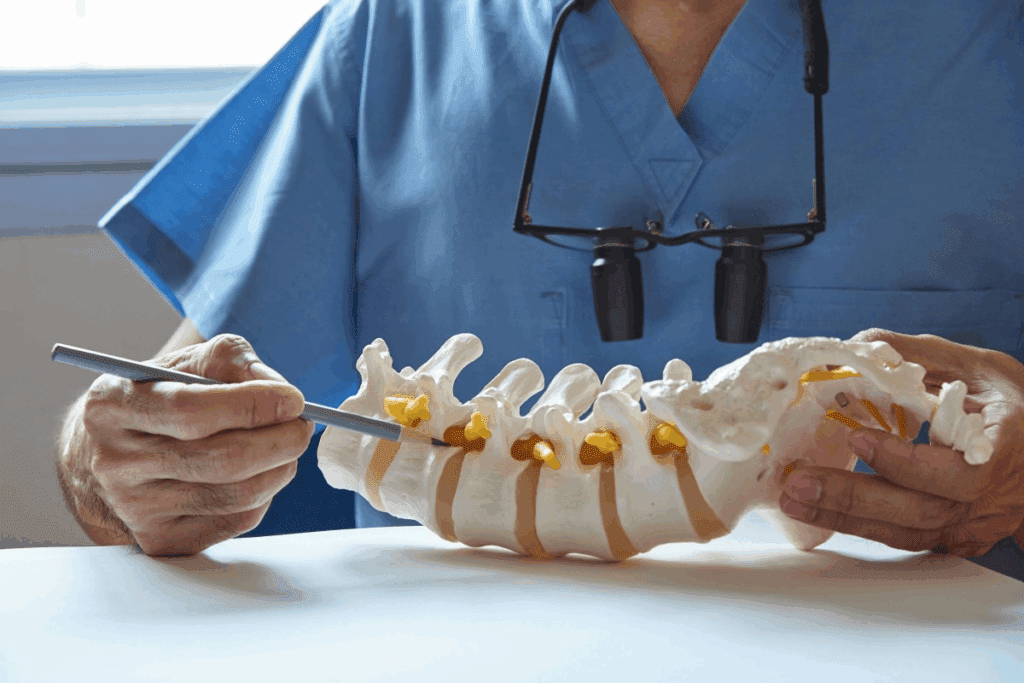
Many people deal with back pain from a herniated disc. But can it lead to paralysis? The answer is not simple. A herniated disc happens when the soft center of the disc leaks out through a tear. This can press on nearby nerves or the spinal cord. Understand how Herniated Disc and Paralysis are connected and when spinal pressure becomes dangerous.
This pressure can cause many symptoms, like numbness and tingling. In bad cases, it can even cause paralysis. We will look into how herniated discs and paralysis are connected. We’ll talk about the risks, symptoms, and ways to treat it.

It’s important to know about herniated discs to understand the risk of paralysis and other nerve problems. A herniated disc, also called a slipped or bulging disc, happens when the soft center leaks out through a tear in the outer layer.
A herniated disc happens when the tough outer layer cracks or tears. This lets the soft inner material, called the nucleus pulposus, leak out. This can press on nerves, causing pain, numbness, and tingling.
Many things can cause a disc to herniate, like wear and tear, injury, or genetics. As we age, our discs lose moisture and become less flexible, making them more likely to herniate. Sudden injuries or strains can also cause this problem.
Some common causes include:
Herniated discs can happen anywhere in the spine but are most common in the lumbar region. Where and how the herniation happens can affect symptoms and risks.
| Location | Common Symptoms | Associated Risks |
| Lumbar Region | Sciatica, lower back pain, numbness in legs | Risk of cauda equina syndrome |
| Cervical Region | Neck pain, numbness or tingling in arms | Risk of spinal cord compression |
| Thoracic Region | Mid-back pain, numbness or weakness in torso or legs | Risk of spinal cord injury |
Knowing where and how a disc herniates is key to finding the right treatment. It helps figure out the risk of nerve problems, including paralysis.
It’s important to know how the spine and nervous system work together. This is because a herniated disc can cause paralysis. The spine and nervous system are connected, controlling movement and feeling.
The spinal cord is a key part of our nervous system. It runs from the brain to the lower back. It’s protected by vertebrae, which form the spinal column.
The spinal cord sends messages between the brain and the body. It helps us move and react without thinking.
Spinal cord compression can happen if a disc herniates. This can mess up these messages and cause problems. How bad it is depends on where and how much the cord is compressed.
Nerve roots come out of the spinal cord and go to different parts of the body. They help us move and feel things. Nerve root damage from a herniated disc can cause pain, numbness, or weakness.
Each nerve root does a specific job. It affects certain skin areas or muscle groups. Damage to a nerve root can cause specific problems, like losing feeling or muscle weakness.
Nerves are vital for movement and feeling. Motor nerves send signals to muscles, letting us move. Sensory nerves send information back to the brain, helping us feel things.
Spinal nerve damage can mess up these functions. This can lead to neurological damage that affects how we move or feel. Knowing how nerves work helps us understand the effects of a herniated disc.
Disc herniation can harm nerve function in several ways. It mainly does this through mechanical pressure and inflammation. When a disc herniates, it can press on or irritate nearby nerves. This leads to various neurological symptoms.
Mechanical pressure on nerves happens when a herniated disc presses on or moves nerve roots. This can mess up normal nerve function. Symptoms like pain, numbness, tingling, and weakness in the affected limb can occur. The severity of these symptoms depends on how much the nerve is compressed and which nerves are affected.
Key effects of mechanical pressure on nerves include:
Herniated discs can also cause an inflammatory response. The herniated disc material can release chemicals that irritate nerves, leading to inflammation. This inflammation can make nerve dysfunction worse, adding to symptoms.
The inflammatory process involves:
Nerve compression from disc herniation can be either sudden or long-term. Acute compression happens suddenly, often from a specific injury. Chronic compression develops over time, due to progressive disc herniation or spine degeneration.
The differences between acute and chronic nerve compression include:
| Characteristics | Acute Nerve Compression | Chronic Nerve Compression |
| Onset | Sudden | Gradual |
| Symptoms | Severe pain, rapid onset of neurological deficits | Gradual development of symptoms, potentially less severe |
A herniated disc can cause serious problems, like paralysis. But knowing how likely it is helps us make better choices. We’ll look at the real risk of paralysis from herniated discs, using data and risk factors.
The chance of paralysis from a herniated disc is low but not zero. Most studies say less than 1% face serious damage, like paralysis. But some things can make this risk higher.
Where the herniation is matters a lot. Herniations in the neck are more risky because they’re close to the spinal cord. Herniations in the lower back are serious but less likely to cause paralysis.
Several things can raise the risk of paralysis from a herniated disc. These include:
Knowing these factors helps us understand our own risk. It also helps us make better choices about treatment.
The risk of paralysis changes based on where the herniated disc is. Here’s a look:
| Herniation Location | Paralysis Risk | Common Symptoms |
| Cervical | Higher | Neck pain, arm weakness, numbness |
| Thoracic | Moderate | Mid-back pain, possible abdominal weakness |
| Lumbar | Lower | Lower back pain, leg weakness, sciatica |
This shows how different herniated discs have different risks. It stresses the importance of knowing where the herniation is for the right treatment.
It’s important to know the signs of possible paralysis early. A herniated disc can cause serious problems if not treated quickly. We’ll talk about the signs that mean you might need to see a doctor fast.
One key sign is when your neurological symptoms get worse. You might feel your muscles getting weaker or find it hard to move your limbs. You could also feel numbness or tingling in different parts of your body.
These symptoms can get worse and lead to serious problems like leg paralysis. It’s vital to watch for any changes in how you feel and tell your doctor.
Severe pain is another sign you should not ignore. The pain from a herniated disc can feel sharp or dull. If it’s really bad and stops you from doing everyday things, you need to see a doctor.
Changes in how you move and react are also important signs. A herniated disc can affect your reflexes, making them less strong or even gone. You might also find it harder to balance or move around.
In some cases, a herniated disc can mess with your bowel and bladder functions. This is a serious problem. Symptoms include trouble with urination or bowel movements. If you have these issues, get help right away.
Knowing these signs can help you avoid paralysis. If you notice any of these symptoms, talk to your doctor. They can help figure out what to do next.
When nerves in the lower spine get compressed, it can cause cauda equina syndrome. This is a serious condition that needs quick medical help. It can happen due to a herniated disc, tumor, or other reasons that press on the nerves.
Cauda equina syndrome happens when nerves in the lower spine get squished. It can be caused by a herniated disc, spinal stenosis, or tumors.
The signs of cauda equina syndrome can vary. But common ones include severe lower back pain, numbness or tingling in the legs, and trouble with the bladder or bowels. Seeking medical help right away is key if you notice these symptoms.
Other signs might include weakness or paralysis in the legs, loss of reflexes, and pain or numbness in the groin or genital area. Spotting these symptoms early is critical to avoid lasting harm.
If cauda equina syndrome isn’t treated quickly, it can cause permanent nerve damage. This can lead to chronic pain, paralysis, and loss of bladder and bowel control. The severity of these outcomes shows why getting medical help fast is so important.
Quick diagnosis and treatment can greatly improve your chances of recovery. It can also lower the risk of long-term problems.
Knowing if a spinal cord injury is complete or incomplete is key to recovery hopes. Spinal cord compression happens when pressure is put on the spinal cord. This can be due to herniated discs, trauma, or tumors.
A complete spinal cord injury means the spinal cord is badly damaged. This results in no function below the injury. On the other hand, an incomplete spinal cord injury has partial damage. Some function may be left below the injury site.
The injury’s severity greatly affects the damage and recovery chances. Knowing if a spinal cord compression is complete or incomplete is vital. It helps decide the right treatment and what to expect.
Recovery chances differ a lot between complete and incomplete spinal cord injuries. Those with incomplete injuries usually have a better chance of getting better. This is because some nerve pathways might be working.
People with complete injuries face a tougher road. Yet, with the right rehab, they can see big improvements in their life and function.
Rehab, like physical and occupational therapy, is very important. It helps a lot with recovery. But, how well it works depends on the injury’s severity and the person’s health.
The effects of complete versus incomplete spinal cord compression are huge. Those with complete injuries might face big challenges in moving and feeling things. They might need a lot of help with daily tasks.
Those with incomplete injuries might keep some of their motor and sensory skills. This means they could be more independent.
It’s important to understand these differences for better rehab plans and support. By knowing the unique challenges of each, healthcare can offer better care and guidance.
Diagnosing herniated discs with neurological complications requires several steps. It’s important to get it right to choose the right treatment and avoid more damage.
A detailed physical exam is the first step. We check how well nerves work using different methods. These include:
These tests help us see if there’s nerve damage from the herniated disc.
Imaging studies are key to confirming the diagnosis. They show how bad the herniated disc is. The most common ones are:
Electromyography (EMG) and nerve conduction studies (NCS) are tests for nerve and muscle health. EMG looks at muscle electrical activity. NCS checks nerve signal speed and strength.
| Test | Purpose | Information Provided |
| Electromyography (EMG) | Measures muscle electrical activity | Checks for muscle or nerve problems |
| Nerve Conduction Studies (NCS) | Evaluates nerve signal speed and strength | Finds nerve damage or compression |
These tests are vital for understanding the disc’s impact on nerves. They help us decide the best treatment.
Non-surgical treatments for herniated discs aim to reduce symptoms and improve life quality. Each patient’s case is different, so we tailor treatments to fit their needs.
The time needed for non-surgical treatment varies. We usually suggest trying it for 6 to 12 weeks before looking at surgery. We watch how the patient does and change the plan if needed.
Several things affect how long treatment lasts. These include how bad the symptoms are, if there are nerve problems, and the patient’s health. We also look at how well the patient responds to early treatments.
Managing pain is key in treating herniated discs without surgery. We use a mix of medicines and other methods to help with pain.
Physical therapy is important in treating herniated discs without surgery. A special exercise program can make muscles stronger, improve flexibility, and help posture.
Physical therapy may include stretching to improve flexibility, exercises to strengthen the spine, and teaching on how to move properly to avoid making symptoms worse.
Non-surgical treatment is best for those with mild to moderate symptoms and no serious nerve problems. It’s also for those who don’t want surgery or aren’t good candidates for it.
By focusing on the patient and using a wide range of non-surgical methods, we can manage symptoms, improve function, and enhance life quality for those with herniated discs.
When a herniated disc risks paralysis, surgery is often the best choice. We know surgery sounds scary, but it’s sometimes the only way to avoid serious damage.
Not every herniated disc needs surgery right away. But some cases are emergencies to stop paralysis. These include:
Quick surgery is key to avoid permanent damage from severe herniated disc symptoms.
There are many ways to treat herniated discs that could lead to paralysis. The right surgery depends on the disc’s location, how bad it is, and the patient’s health.
Some common surgeries are:
Recovery from herniated disc surgery varies. It depends on the surgery type and the patient’s health. Generally, patients can expect:
We stress that follow-up care is key for the best recovery and to avoid problems.
Knowing about surgery options and recovery helps patients make smart choices. Our team is dedicated to giving full care and support during the surgery process.
The journey to recovery after neurological damage is complex. It involves a tailored rehabilitation strategy for each person. We know that rehabilitation is key to helping patients regain lost functions and reach their best recovery.
The first step in rehabilitation is to stabilize the patient and meet their immediate needs. Healthcare professionals conduct a thorough assessment to understand the extent of the damage. They then create a personalized treatment plan. Early intervention is critical to prevent further damage and set the stage for long-term recovery.
During this phase, patients may start various therapies. These include physical therapy to improve mobility, occupational therapy for daily tasks, and speech therapy if needed. The aim is to increase the patient’s independence and improve their quality of life.
Long-term rehabilitation focuses on ongoing recovery and adaptation. It may include continued physical therapy, vocational rehabilitation to help patients return to work, and other interventions. Consistency and patience are key during this phase, as progress may be slow.
We work closely with patients to set realistic goals and adjust their plans as needed. This collaborative approach ensures patients get the support they need to reach their recovery goals.
Assistive devices and adaptations are vital for daily activities. They include mobility aids, ergonomic adjustments, and other tools to improve independence. The right assistive technology can greatly enhance a patient’s quality of life and ability to participate in meaningful activities.
Setting realistic recovery goals is a critical part of rehabilitation. We help patients set achievable objectives that match their needs and aspirations. By breaking down big goals into smaller steps, patients can track their progress and stay motivated.
Recovery from neurological damage is complex and highly individualized. With a detailed rehabilitation program, the right support, and a commitment to recovery, patients can see significant improvements in their function and quality of life.
Living with partial paralysis or neurological deficits is tough. It affects many parts of life, from physical to emotional and psychological. These challenges can be hard to handle.
Adapting to sensory and motor changes is a big challenge. People learn new ways to do daily tasks and manage sensory issues. Rehabilitation programs help a lot in this process.
For example, people might need to use assistive devices or change their homes. This can be hard, both physically and emotionally. It takes patience, support, and sometimes professional help.
The psychological effects of living with partial paralysis or neurological deficits are real. Losing physical function and changing lifestyle can cause frustration, depression, and anxiety. Mental health support is key for coping.
Keeping mental health in check is as important as physical rehab. Support from family, friends, and mental health experts can help a lot. It makes it easier to deal with the condition.
Having access to support resources and communities is vital. These include rehab services, support groups, and online communities. Support groups are great for sharing experiences, getting advice, and finding emotional support.
We suggest using these resources as part of your care plan. They can improve your life and help you deal with the challenges of living with paralysis or neurological deficits.
Keeping your spine healthy is key to avoiding severe disc herniation. It begins with knowing the right ways to move. By using a few simple strategies, we can lower the risk of disc herniation.
Using proper body mechanics is vital to prevent disc herniation. This means keeping good posture, lifting right, and avoiding sudden twists or bends. Being aware of our movements helps lessen spine and disc strain.
Core strengthening is also key in preventing disc herniation. Our core muscles, like abs and back, support our spine. Regular exercises that strengthen these muscles improve spinal stability and lower herniation risk.
Some great core exercises include:
Workplace ergonomics is also important in preventing disc herniation. A well-set workspace promotes good posture and lessens spine strain. Adjust your chair, monitor, and keyboard to comfortable levels.
Along with proper body mechanics, core strengthening, and workplace ergonomics, making lifestyle changes helps too. This includes staying at a healthy weight, exercising regularly, and not smoking.
By adding these preventive steps to our daily routine, we can greatly lower the risk of severe disc herniation. This keeps our spine healthy and working well.
Knowing when to get emergency help for a herniated disc can save lives. A herniated disc can press on nerves or the spinal cord. This can cause serious damage if not treated quickly.
Some symptoms mean you need emergency care. These include:
When you go to the emergency room, tell the doctors everything. This includes:
Getting help fast is key to avoiding long-term harm. Timely medical care can greatly improve outcomes for those with severe herniated disc issues. Waiting too long can lead to permanent damage.
At the hospital, you’ll get a detailed check-up. This includes:
| Evaluation Component | Description |
| Physical Examination | Assessment of neurological function, including strength, sensation, and reflexes. |
| Imaging Studies | Use of MRI or CT scans to visualize the herniated disc and its impact on surrounding nerves. |
| Diagnostic Tests | Electromyography (EMG) and nerve conduction studies to assess nerve function. |
Knowing when to seek emergency care is critical for those with severe herniated disc symptoms. Recognizing red flag symptoms and acting quickly can greatly improve your chances of a good outcome.
It’s important to know about the dangers of herniated discs to avoid serious issues like paralysis. We’ve looked into how a herniated disc can harm the spinal cord and why quick treatment is key.
A herniated disc can cause paralysis by pressing on the spinal cord or nerve roots. This can lead to serious nerve damage. The chance of paralysis depends on where and how bad the herniation is.
Getting medical help right away is vital to avoid lasting nerve problems. There are different treatments, from simple care to surgery, based on how bad the problem is.
Preventing herniated discs is also critical. Keeping a healthy posture, strengthening your core, and making sure your work area is set up right can help a lot. These steps can lower the risk of disc problems.
Knowing about herniated discs, their symptoms, and treatment options helps people protect their spine. This way, they can avoid serious issues like paralysis.
Yes, a herniated disc can press on the spinal cord or nerves. This might lead to paralysis. The risk depends on where and how severe the herniation is.
Look out for weakness, losing sensation, changes in reflexes, and severe pain. If you notice these, get medical help right away.
Paralysis from a herniated disc is not common. But, it can happen, mainly if the disc presses on the spinal cord. The risk is higher with certain types and locations of herniation.
Cauda equina syndrome is when nerves in the spinal canal get compressed, often by a herniated disc. It’s a serious condition that needs quick medical attention to avoid lasting damage.
Sometimes, treatments like pain management and physical therapy can help. They might prevent paralysis. But, severe cases might need surgery.
Surgery is needed if there’s severe nerve damage, like big weakness, loss of feeling, or cauda equina syndrome. In some cases, emergency surgery is required.
Recovery starts with rest, then physical therapy. How well you recover depends on the damage and how well the surgery works.
Reversing paralysis depends on how severe and long the compression was. Quick medical help can help, but some cases might have lasting damage.
To lower the risk, keep good posture, strengthen your core, and make sure your work area is ergonomic. These steps can help prevent disc problems.
Look out for sudden, severe pain, worsening nerve problems, loss of bladder or bowel control, and big weakness or numbness. If you see these, get medical help fast.
Doctors use physical checks, imaging like MRI, and tests like electromyography and nerve conduction studies. These help figure out how much nerve damage there is.
Living with nerve damage means adapting to new feelings and movements. You’ll also need to manage the emotional side and find support. Rehabilitation and tools can improve your life.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!