Last Updated on November 4, 2025 by mcelik
About 80% of adults deal with lower back pain at some point. Herniated discs are a big reason for this pain. The way pain from a herniated disc feels can really differ from person to person. Find out about Herniated disc pain patterns, including when pain worsens or eases during activity.
Herniated disc pain doesn’t always hurt all the time. It can show up as intermittent pain, localized discomfort, or radiating pain. This last one is called sciatica when it hits the sciatic nerve.
We’ll look into the different pain patterns linked to herniated discs. This will help you get why and when pain happens.
Key Takeaways
- Herniated disc pain can be intermittent or constant.
- The type and level of pain vary among individuals.
- Localized discomfort and radiating pain are common manifestations.
- Sciatica is a specific type of radiating pain affecting the sciatic nerve.
- Understanding pain patterns is key to managing it well.
Understanding Herniated Discs: The Basics
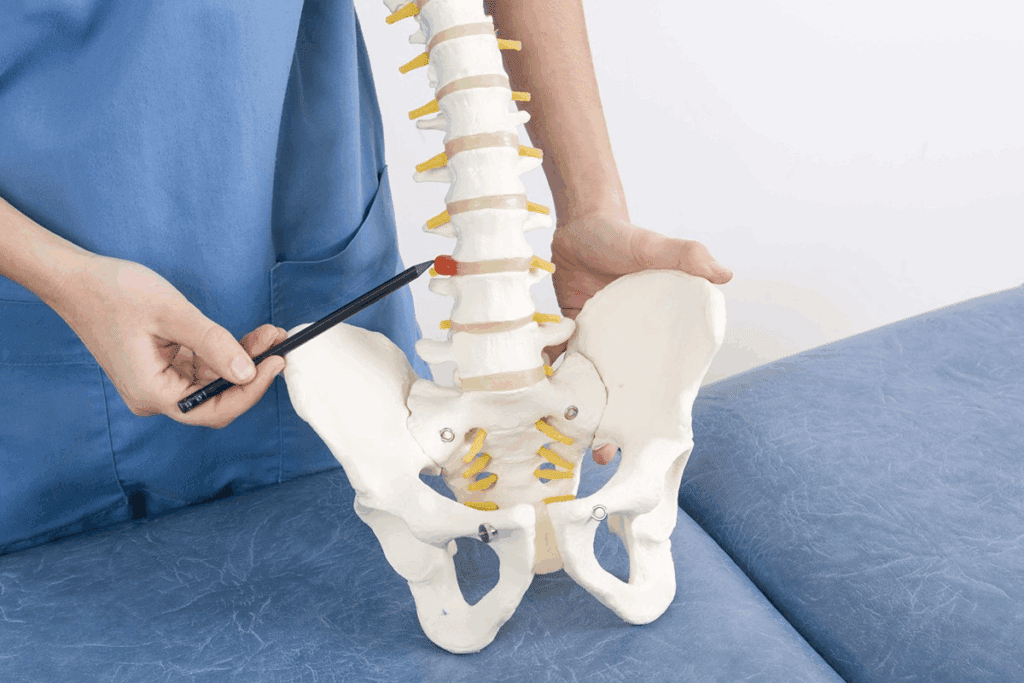
To understand herniated disc pain, knowing what a herniated disc is key. It happens when the soft center of the disc leaks out through a tear. This can irritate nerves and cause pain.
What Is a Herniated Disc?
A herniated disc is also called a slipped or ruptured disc. It’s when the soft inside of the disc bulges out through the tough outer layer. This usually happens in the lower back and neck.
Spinal Anatomy and Disc Function
The spine has vertebrae and discs that act as shock absorbers. The discs have a tough outer layer and a soft, gel-like center. They help the spine move smoothly and absorb shock.
How and Why Discs Herniate
Disc herniation can come from aging, wear and tear, or injury. As we get older, discs dry out and can tear more easily. A sudden injury can also cause a disc to herniate, leading to pain.
- Aging: Discs lose water content and become more susceptible to herniation.
- Wear and Tear: Continuous strain on the spine can cause discs to degenerate.
- Injury: Sudden trauma can cause a disc to herniate.
Knowing these basics helps us understand how herniated discs cause pain. It also shows how they can be treated.
The Nature of Herniated Disc Pain

To understand herniated disc pain, we must look at its causes. This includes nerve compression and inflammation. It’s a complex issue that affects people differently. Knowing how it works is key to managing it well.
Nerve Compression Mechanisms
Nerve compression is a main cause of herniated disc pain. When a disc herniates, it can press on nerves. This leads to pain and discomfort. The amount of compression affects how much pain someone feels.
Nerve compression can happen in a few ways:
- Direct compression by the herniated disc material
- Inflammation surrounding the nerve roots
- Chemical irritation from the disc contents
Inflammatory Response
The body reacts to a herniated disc with inflammation. This inflammation can make nerve pain worse. It’s important to understand this to find good treatments.
| Inflammatory Mediators | Role in Herniated Disc Pain |
| Cytokines | Promote inflammation and pain signaling |
| Chemokines | Attract immune cells to the site of herniation |
| Prostaglandins | Enhance pain perception and inflammation |
Referred Pain Patterns
Herniated discs can cause pain in areas other than where the herniation is. This happens when nerves are compressed or irritated. These nerves send pain signals to other parts of the body.
Referred pain patterns depend on the herniation’s location:
- Lumbar herniations often refer pain to the legs
- Cervical herniations can cause pain in the arms or neck
Understanding these mechanisms helps doctors give better treatments. This way, people with herniated disc pain can get the help they need.
Types of Herniated Discs and Their Pain Characteristics
Knowing about the different herniated discs is key to managing pain well. These discs can be found in the lumbar, cervical, and thoracic areas. Each area has its own pain patterns.
Lumbar Disc Herniation
Lumbar disc herniation is common and happens in the lower back. It leads to sciatica, causing sharp pain that shoots down to the legs. Activities like lifting heavy things or bending can make the pain worse.
Cervical Disc Herniation
Cervical disc herniation is in the neck and can cause pain in the arms, shoulders, or upper back. Symptoms include numbness, tingling, or weakness. Neck pain can affect daily tasks like driving or using a computer.
Thoracic Disc Herniation
Thoracic disc herniation is less common and is in the mid-back. It can cause chest or abdomen pain, sometimes feeling like heart or stomach issues. The pain can be dull or sharp, getting worse with deep breathing or movement.
Each herniated disc type has its own pain challenges. Knowing these differences helps in finding the right treatment. Consult healthcare professionals to find the best treatment for your specific case.
Herniated Disc Pain Patterns: Is the Pain Constant?
Herniated disc pain can change a lot over time. Research shows that the pain can shift, with sharp pain followed by times when you feel no pain at all. This back-and-forth is common and something patients need to get used to.
Acute vs. Chronic Pain Phases
Herniated disc pain goes through different stages. The acute phase starts with sudden, severe pain from the injury or herniation. This phase is filled with inflammation and a lot of discomfort. On the other hand, the chronic phase is about ongoing pain that might not be as bad but lasts longer.
The shift from acute to chronic pain isn’t always straightforward. Some people might see their pain lessen as the inflammation goes down. But then, pain can come back because of nerve compression or muscle tension.
Pain-Free Intervals
One tricky thing about herniated disc pain is the pain-free intervals. During these times, you might think you’re all better, only to have pain come back. How long these breaks last can depend on how bad the herniation is, your spinal health, and how well any treatments are working.
Typical Pain Cycles
Knowing about pain cycles can help both patients and doctors deal with the condition better. These cycles can be affected by what you do every day, how you stand or sit, and even the time of day. For example, pain might get worse when you sit or stand for a long time but feel better when you rest or do certain exercises.
By understanding your pain patterns, you can take steps to manage it. This might mean changing how you move, keeping good posture, and doing the right exercises.
Factors That Influence Pain Intensity
Many things affect how much pain someone with a herniated disc feels. Knowing these factors helps in managing pain better and planning treatments.
Severity of Herniation
The severity of the herniation greatly affects pain levels. A more severe herniation can press nerves harder, causing more pain. We use MRI to see how bad the herniation is and how it affects nerves.
Location of the Herniation
The location of the herniation also matters a lot. Herniations in areas with lots of nerve activity or that press on important nerves hurt more. For example, a herniated disc in the lower back can cause sciatica, which is sharp, shooting pain in the leg.
Individual Pain Tolerance
Individual pain tolerance is different for everyone. Things like health, mental state, and past pain experiences can change how pain is felt. We know that treating pain well means looking at each person’s unique situation.
Healthcare providers can make better treatment plans by understanding these factors. This helps in managing pain better and improving life quality for each person.
When Herniated Disc Pain Typically Worsens
Herniated disc pain can change in intensity. It often gets worse with certain activities or positions. Knowing what triggers it is key to managing the pain and feeling better.
Physical Activities That Exacerbate Pain
Some activities can make herniated disc pain worse. These include:
- Heavy lifting, which increases pressure on the spine
- Bending or twisting, which can irritate the affected disc
- High-impact activities, such as running or jumping, which can shock the spine
Changing or skipping these activities can help ease the pain.
Postures That Increase Pressure on Discs
How you sit or stand affects herniated disc pain. Bad postures can put more pressure on the disc, causing more pain. For example:
- Slouching or slumping, which can put additional stress on the spine
- Leaning forward, which can exacerbate nerve compression
Keeping a good posture is important to lessen the pain.
Impact of Prolonged Sitting or Standing
Both sitting for too long and standing for too long can make herniated disc pain worse. Sitting for a long time can put more pressure on the discs. Standing for a long time can lead to muscle fatigue, which also worsens pain. It’s important to find a balance and take breaks to move or stretch.
Morning Pain and Stiffness: Why It Happens
Morning hours can be tough for those with herniated discs. Many people with this condition wake up feeling stiff and in pain.
Waking up in pain is really tough. Several things cause this, like fluid buildup and pain from first movements after rest.
Overnight Fluid Accumulation
Lying down lets fluid build up around the herniated disc. This swelling puts more pressure on nerves, causing stiffness and pain in the morning.
First Movement Pain
Moving after waking can be very painful. This is because stiffness and inflammation get worse at night. Even simple actions like getting out of bed can make it worse.
It’s important to manage morning pain to stay active. Changing your morning routine and doing gentle stretches can help ease the pain.
Managing Morning Discomfort
Here are some ways to reduce morning stiffness and pain:
- Gentle morning stretches to loosen the muscles around the spine
- Applying heat or cold therapy to reduce inflammation and relax muscles
- Adjusting sleeping positions to reduce pressure on the spine
- Gradually increasing activity levels to avoid sudden strain
Using these tips can help people with herniated discs manage their morning pain. This can improve their daily life a lot.
Radiating Pain and Sciatica
It’s important to understand how radiating pain, sciatica, and herniated discs are connected. A herniated disc can press on nerves, causing various symptoms.
Nerve Compression and Radiating Pain
When a disc herniates, it can press on a spinal nerve. This can cause pain that spreads along the nerve’s path. For example, if a disc in the lower back presses on the sciatic nerve, it can cause pain in the leg, known as sciatica.
The pain spreads because of how nerves work. When a nerve is compressed, it sends pain signals to the brain. The brain then feels this as pain in specific areas.
Sciatica Symptoms and Patterns
Sciatica is pain that spreads along the sciatic nerve, from the lower back to the legs. Symptoms can vary and may include numbness, tingling, or weakness in the leg.
Sciatica usually affects one leg at a time. The pain can be mild or severe. Activities that put pressure on the nerve, like coughing or sitting for a long time, can make symptoms worse.
Differentiating Sciatica from Other Conditions
It’s key to tell sciatica apart from other leg pain causes. Sciatica is often linked to herniated discs, but other issues like spinal stenosis or piriformis syndrome can also cause similar symptoms.
A detailed medical check-up is needed to accurately diagnose sciatica. Tests like MRI or EMG might be used to find the root cause of the symptoms.
Muscle Spasms and Secondary Pain
When a disc herniates, it can start a chain of symptoms. Muscle spasms are a common side effect, making pain worse. These spasms add to the discomfort.
Causes of Muscle Spasms Around Herniated Discs
Muscle spasms happen as a protective measure. The muscles tighten to keep the spine stable and prevent more injury. This tightening is a natural response to nerve irritation around the herniated disc.
Contribution to Overall Pain
Muscle spasms around a herniated disc can cause a lot of pain. This pain comes from both the herniation and the muscle tension. As muscles spasm, they can press on nerves, creating a cycle of pain.
Also, muscle tension can change how we move and stand. This can put extra strain on other parts of our body. It can make pain harder to manage.
Breaking the Pain-Spasm Cycle
To stop the cycle of pain and muscle spasms, we need to act. Gentle stretching, physical therapy, and relaxation can help. Sometimes, medication is needed for severe spasms.
It’s key to fix the herniated disc and muscle spasms’ root cause. This might mean changing our lifestyle, improving our workspace, and doing exercises to strengthen our back.
Understanding muscle spasms and their role in pain helps us manage herniated disc pain better. This improves life quality for those affected.
Sleep Disturbances and Nighttime Pain
Herniated disc pain often gets worse at night. This can lead to trouble sleeping and a lower quality of life. It not only affects how you feel but also how you manage pain during the day.
Why Pain May Worsen at Night
Several things can make pain worse at night. Inflammation tends to rise later in the day. Fatigue can also make pain feel more severe. Plus, lying down can shift your spine, irritating the affected disc and nerves.
It’s important to understand these factors to find ways to reduce nighttime pain.
Optimal Sleeping Positions
Choosing the right sleeping position can help reduce nighttime pain. Here are some tips:
- Side Sleeping: Use a supportive pillow between your knees to keep your hips aligned.
- Back Sleeping: Place a pillow under your knees to take pressure off your spine.
- Avoid Stomach Sleeping: This position can cause your neck to be twisted, potentially worsening pain.
Sleep Aids and Strategies
There are also sleep aids and strategies to help manage nighttime pain:
- Relaxation Techniques: Practices like deep breathing or meditation can help reduce stress and promote relaxation.
- Pain Management Medication: Talk to your healthcare provider about taking pain relief medication before bedtime.
- Comfortable Sleep Environment: Make sure your bedroom is cool, dark, and quiet to help you sleep better.
By using these strategies, people with herniated discs can sleep better and feel better overall.
Diagnosing Herniated Disc Pain
Diagnosing herniated disc pain takes a detailed approach. It includes physical exams, imaging studies, and sometimes nerve tests. Getting the diagnosis right is key. It helps doctors create a treatment plan that fits the patient’s needs.
Physical Examination Techniques
A detailed physical exam is the first step. Doctors use different methods to check the patient’s condition. They look at:
- Checking reflexes and muscle strength
- Assessing pain levels and where it hurts
- Evaluating how well the patient moves
- Doing specific tests like the straight leg raise test
These steps help find out if nerves are being compressed or irritated. This is often seen in herniated discs.
Imaging Studies
Imaging tests are key to confirming a herniated disc diagnosis. The main tests used are:
- Magnetic Resonance Imaging (MRI): MRI is the top choice for seeing herniated discs. It shows soft tissues like discs, nerves, and the spinal cord clearly.
- Computed Tomography (CT) scans: CT scans can show the spine and any bone problems. But they’re not as good as MRI for soft tissues.
- X-rays: X-rays aren’t the best for herniated discs. But they can help rule out other back pain causes like fractures or wear and tear.
These tests help doctors see the herniated disc and how it affects nearby areas.
Nerve Conduction Studies
In some cases, nerve tests like NCS and EMG are used. They check muscle electrical activity and nerve signal speed.
These tests are helpful when the diagnosis is not clear. They help tell if pain or weakness is from nerve compression or something else.
Conservative Treatment Approaches
Managing herniated disc pain often starts with conservative treatments. These methods aim to ease symptoms and enhance life quality without surgery. We’ll look at rest, physical therapy, and medication options.
Rest vs. Activity: Finding the Right Balance
Finding the right mix of rest and activity is key. Too much rest can make you stiff and weak. A balanced approach with gentle exercises and gradual activity is best.
Gentle exercises keep you flexible and reduce muscle tension. Walking, swimming, or yoga are good choices. Avoid heavy lifting and bending to prevent worsening the condition.
Physical Therapy Interventions
Physical therapy is vital for herniated disc pain. A physical therapist creates a plan to strengthen muscles, improve flexibility, and posture. Manual therapy, like massage, can also help with pain and stiffness.
Physical therapy offers many benefits, including:
- Improved muscle strength and flexibility
- Enhanced posture and spinal alignment
- Reduced pain through manual therapy techniques
- Education on proper body mechanics and ergonomics
Medication Options
There are many medications for herniated disc pain. Over-the-counter pain relievers like ibuprofen or acetaminophen can help. Muscle relaxants or oral steroids may be used for severe cases.
Always follow your doctor’s advice on medications. They can have side effects and interact with other drugs. A personalized pain management plan is essential, considering your health and history.
Combining rest, physical therapy, and medication can help manage pain. We work with patients to create a treatment plan that meets their needs and promotes recovery.
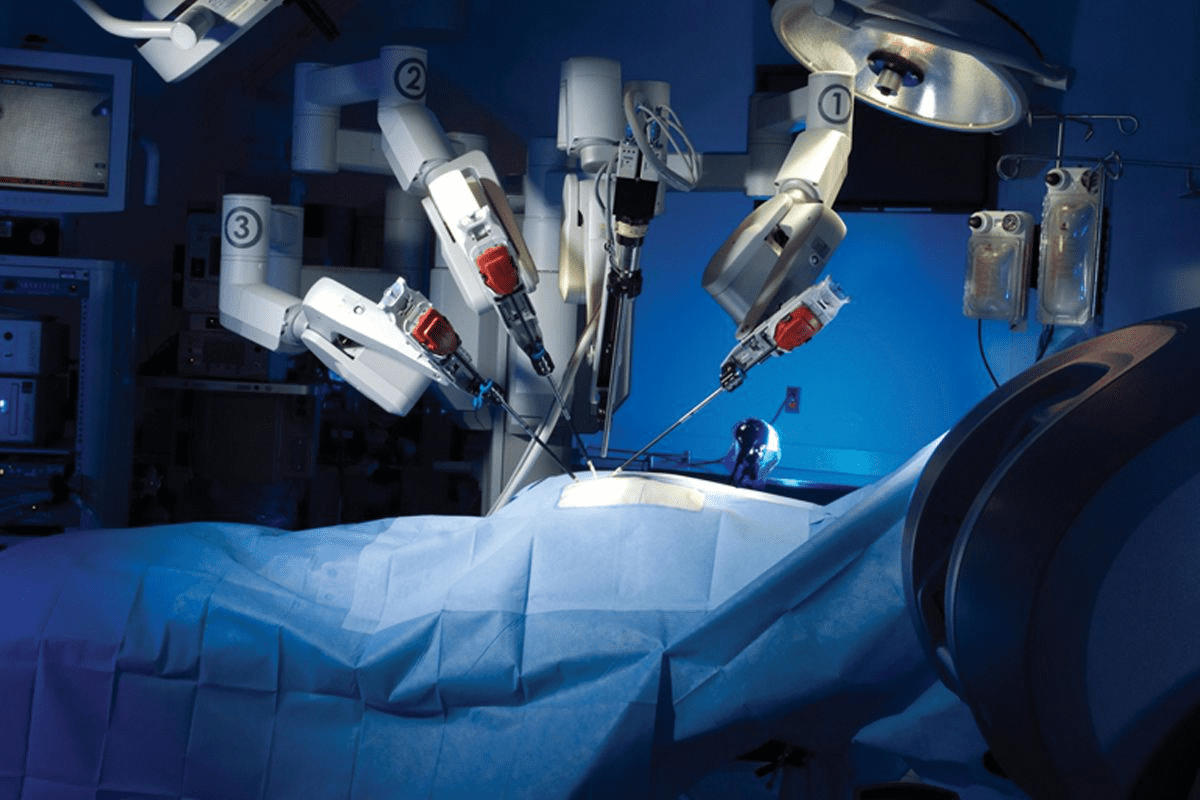
When Surgery Might Be Necessary
When other treatments don’t help, surgery might be needed. This can seem scary, but it can really help those with bad symptoms. It’s a big step, but it can bring a lot of relief.
Indications for Surgical Intervention
Surgery is usually considered when certain things happen. For example, if nerve compression causes a lot of pain or weakness. Other reasons include:
- Severe or getting worse neurological problems
- Cauda equina syndrome, which is an emergency
- Pain that stops you from doing daily things and can’t be fixed by other treatments
- Big disc herniations that press on nerves
Types of Surgical Procedures
There are many ways to fix herniated discs. The right one depends on where and how big the herniation is, and the patient’s health.
- Discectomy: This is when they remove the bad part of the disc.
- Microdiscectomy: A smaller version of discectomy, using special tools and a microscope.
- Spinal Fusion: Sometimes, fusing the spine is needed to keep it stable, if it’s unstable.
We’ll talk more about these options. We’ll cover their good points and possible downsides.
Recovery Expectations After Surgery
How long it takes to get better after surgery varies. It depends on the surgery and the person. Usually, people can expect:
- First few weeks: Rest and not doing much
- Physical therapy to get stronger and more flexible
- Slowly getting back to normal over weeks or months
It’s very important to follow the doctor’s instructions after surgery. We’ll also look at ways to handle pain and discomfort while recovering.
Self-Management Strategies for Pain Relief
Managing pain from herniated discs is key. By using certain methods and changing your lifestyle, you can lessen pain and live better.
Heat and Cold Therapy
Heat and cold therapy are simple yet effective ways to manage pain. Heat therapy relaxes muscles and boosts blood flow, aiding in healing. Cold therapy cuts down inflammation and dulls pain. Switching between heat and cold can offer the best relief.
- Apply heat for 15-20 minutes with a warm bath, shower, or a low-setting heating pad.
- Use cold packs wrapped in a towel to avoid skin contact, applying for 10-15 minutes.
Gentle Stretches and Exercises
Doing gentle stretches and exercises keeps your spine flexible and strengthens muscles. This reduces pressure on the herniated disc. Start slowly and gently to avoid making things worse.
Recommended exercises include:
- Pelvic tilts
- Knee to chest stretches
- Cat-cow stretches
Seeing a healthcare professional or physical therapist can help tailor exercises for you.
Ergonomic Adjustments
Adjusting your daily activities and workspace ergonomically can lessen back strain. This includes:
- Maintaining proper posture while sitting and standing
- Using ergonomic furniture and accessories
- Taking regular breaks to stretch when working or driving
By using these self-management strategies, you can actively manage your herniated disc pain. This improves your overall well-being.
The Recovery Timeline: What to Expect
Understanding the recovery process for a herniated disc is key. Knowing the healing phases and signs of improvement is vital. The journey can be complex, with many factors affecting healing speed and success.
Typical Healing Phases
The healing process for a herniated disc has several phases. First, managing pain and inflammation is the focus. Acute pain usually goes away in the first few weeks as healing starts.
Next, symptoms and function slowly get better, taking months. Physical therapy and gentle exercises are important. They help strengthen muscles and improve spine flexibility. Patients often see ups and downs in symptoms.
Signs of Improvement
As the disc heals, several signs of improvement are seen. These include:
- Less pain and fewer episodes
- Better range of motion and flexibility
- Easier daily activities without pain
- Ability to do more strenuous activities or sports
Watching for these signs helps adjust treatment plans. It keeps recovery on track.
When to Be Concerned About Lack of Progress
While recovery speeds vary, some situations need attention. These include:
- Steady or growing pain despite treatment
- More numbness, tingling, or weakness in limbs
- Hard time controlling bowel or bladder
- Big loss of mobility or function
If these symptoms happen, see a healthcare provider. They can reassess and suggest new treatments.
Knowing the recovery timeline and being aware of progress and complications helps. It makes recovery better for those with a herniated disc.
Conclusion: Living with and Beyond Herniated Disc Pain
Managing herniated disc pain well needs a full plan. This includes pain control, long-term plans, and exercises for herniated discs. Knowing about herniated disc pain helps people deal with it better and live better lives.
Being active about spinal health is key when living with herniated disc pain. This means staying at a healthy weight, doing herniated disc exercises regularly, and making work and home spaces ergonomic. It’s also important to watch how you sit and move to avoid making spinal disc injury worse.
We’ve looked at many ways to treat herniated disc pain. From physical therapy and medicine to surgery when it’s needed. Adding self-care like heat and cold therapy, gentle stretches, and the right sleep can really help reduce pain and boost health.
In the end, managing herniated disc pain is about taking charge of your spinal health. Making smart choices about pain management can help you move past the pain. With the right steps, you can aim for a healthier, more active life.
FAQ
Does a herniated disc always cause pain?
No, not every herniated disc causes pain. Pain levels can vary. This depends on the herniation’s location and severity, and how sensitive a person is to pain.
What are the common symptoms of a herniated disc?
Symptoms include pain in one spot, pain that spreads, sciatica, numbness, tingling, and muscle weakness. These depend on where and how severe the herniation is.
Why does herniated disc pain sometimes worsen at night?
Nighttime pain can increase because of inflammation, muscle relaxation, and changes in how the spine aligns during sleep. These changes can put more pressure on the disc and nerves.
Can physical activity exacerbate herniated disc pain?
Yes, activities like heavy lifting, bending, or twisting can make herniated disc pain worse. They increase pressure on the affected disc.
How can I manage morning stiffness and pain caused by a herniated disc?
To manage morning stiffness and pain, try gentle stretches, heat or cold therapy, and slowly getting active after waking up.
What is the difference between acute and chronic herniated disc pain?
Acute pain is sharp and sudden, often from a specific event. Chronic pain is ongoing and can be due to inflammation and nerve irritation.
Can herniated disc pain be constant, or are there pain-free intervals?
Pain from a herniated disc can change. Some people have constant pain, while others have times without pain. The pattern of pain varies based on the herniation’s severity and individual factors.
How is herniated disc pain diagnosed?
Doctors use physical exams, imaging like MRI, and sometimes nerve tests to diagnose. These help find the pain’s source and assess nerve function.
What are the conservative treatment options for herniated disc pain?
Treatments include balancing rest and activity, physical therapy, and pain and inflammation medications.
When is surgery considered necessary for a herniated disc?
Surgery is needed if treatments don’t work, or if there’s nerve damage. Signs include progressive weakness or loss of bladder/bowel control.
What self-management strategies can help alleviate herniated disc pain?
Strategies include using heat and cold, gentle exercises, ergonomic changes, and keeping a healthy weight to reduce spine pressure.
What is the typical recovery timeline for a herniated disc?
Recovery times vary. Most people see improvement in weeks to months with the right treatment and self-care.
How can I prevent herniated disc pain from recurring?
To prevent recurrence, live a healthy lifestyle. This includes regular exercise, proper lifting, and ergonomic adjustmentsto protect your spine.
Reference:
- Benzakour, T., Igoumenou, V., Mavrogenis, A. F., & Benzakour, A. (2019). Current concepts for lumbar disc herniation. International Orthopaedics, *43*(4), 841–851. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6449477/