For couples facing infertility, hormone treatment is a proven way to get pregnant. It tackles hormonal imbalances. At places like Liv Hospital, experts know that the right balance of reproductive hormones is key to success hormones for fertility treatment.
Hormone therapy has shown great success in fertility treatments. The World Health Organization (WHO) says about 17.5% of adults worldwide struggle with infertility. By controlling ovulation and getting the uterus ready, hormone treatments boost pregnancy chances.
Key Takeaways
- Hormone treatment addresses hormonal imbalances causing infertility.
- Reproductive hormones are vital for conception and pregnancy.
- Hormone therapy achieves significant success rates in fertility treatments.
- Regulating ovulation and preparing the uterus are key to increasing pregnancy chances.
- Trusted fertility clinics offer complete hormone therapy as part of modern fertility care.
The Science of Reproductive Hormones in Conception
Reproductive hormones are key to conception. Knowing how they work is vital. They control many body functions needed for fertility.
Key Reproductive Hormones Explained
The main hormones for conception are luteinizing hormone (LH), follicle-stimulating hormone (FSH), estrogen, and progesterone. LH and FSH come from the pituitary gland. They help with ovulation and egg growth. Estrogen and progesterone, made by the ovaries, get the uterus ready for a baby.
LH jumps up to start ovulation, releasing a ready egg. FSH helps the ovaries grow follicles, which make estrogen. Estrogen levels go up, making the uterine lining thick and ready for a baby. Progesterone keeps the lining ready for implantation.
The Hormonal Cycle and Fertility Window
The menstrual cycle has different phases, each controlled by hormones. The follicular phase sees estrogen levels go up, helping follicles grow. Then, ovulation happens, moving to the luteal phase, where progesterone takes over, supporting the uterine lining.
Knowing the menstrual cycle and the fertility window is key for getting pregnant. The fertility window is five days before ovulation and the day of ovulation. Having sex during this time boosts chances of getting pregnant.
Common Causes of Hormonal Infertility
Knowing why hormonal infertility happens is key for those trying to conceive. Hormonal imbalances can really affect fertility, making it hard to get pregnant. We’ll look at main conditions like PCOS, thyroid issues, and hyperprolactinemia that lead to hormonal infertility.
Polycystic Ovary Syndrome (PCOS)
PCOS is a common endocrine disorder in women of childbearing age. It affects fertility by causing hormonal imbalances. Women with PCOS often have irregular periods, ovulation problems, and high androgens. These issues can make it hard to conceive and increase miscarriage risk.
The exact cause of PCOS is not known, but genetics and environment play a role. Doctors use clinical exams, ultrasound, and hormone tests to diagnose it.
Thyroid Disorders and Fertility
Thyroid problems, like hypothyroidism and hyperthyroidism, can hurt fertility. The thyroid gland controls metabolism, and its hormones are key for reproduction. Thyroid issues can mess with ovulation, periods, and reproductive health.
Untreated thyroid disorders can cause infertility, miscarriage, and pregnancy problems. Getting the right diagnosis and treatment is important for those trying to conceive.
Hyperprolactinemia and Conception Challenges
High levels of prolactin, known as hyperprolactinemia, can make it hard to get pregnant. Prolactin is a hormone that helps with milk production during breastfeeding. But high levels outside of breastfeeding can mess with ovulation and periods, making it tough to conceive.
Hyperprolactinemia can be caused by pituitary tumors, some medications, and thyroid disorders. Treatment often involves fixing the cause and may include medication to lower prolactin levels.
To understand how these conditions affect fertility, let’s look at some statistics:
Condition | Prevalence | Impact on Fertility |
PCOS | 5-10% of women of reproductive age | Irregular ovulation, hormonal imbalance |
Thyroid Disorders | Up to 5% of the general population | Disrupted ovulation, menstrual irregularities |
Hyperprolactinemia | Variable, often associated with pituitary tumors | Disrupted ovulation, amenorrhea |
Knowing about these common causes of hormonal infertility is the first step to diagnosis and treatment. By fixing hormonal imbalances, many can improve their chances of getting pregnant.
Diagnosing Hormonal Imbalances That Affect Fertility
Hormonal imbalances can greatly affect fertility. Accurate diagnosis is key. This involves detailed tests to understand hormonal issues.
Comprehensive Hormone Panels and Testing
Comprehensive hormone panels are vital for diagnosing fertility issues. These tests check hormones like FSH, LH, estrogen, progesterone, and testosterone. They help doctors spot imbalances that might affect fertility.
Key Hormones Tested:
- FSH: Essential for follicle growth and egg maturation
- LH: Triggers ovulation and supports the corpus luteum
- Estrogen: Crucial for the development of the female reproductive system and regulation of the menstrual cycle
- Progesterone: Prepares the uterus for pregnancy and supports embryonic development
- Testosterone: Though often linked with males, females also produce it, playing a role in libido and reproductive health
Ultrasound Monitoring for Follicle Development
Ultrasound monitoring is essential for assessing fertility. It tracks follicle growth, ovulation, and reproductive organ health. This info is key for timing treatments to increase conception chances.
Ultrasound Parameter | Significance | Normal Values |
Follicle Size | Indicates follicle maturity and readiness for ovulation | 18-24 mm |
Endometrial Thickness | Reflects the receptivity of the uterus for implantation | 7-14 mm |
Ovulation Timing | Critical for planning conception or fertility treatments | Typically occurs 24-36 hours after LH surge |
When to Seek Specialized Reproductive Endocrinology Care
If complex hormonal imbalances are found or fertility issues persist, seek a reproductive endocrinologist. These specialists offer advanced care for hormonal disorders and fertility treatments.
Combining hormone panels, ultrasound monitoring, and specialized care helps individuals and couples tackle their fertility challenges.
Hormones for Fertility Treatment: Options and Approaches
Learning about hormone treatments is key to success in fertility treatment. These therapies tackle specific fertility issues. The right treatment depends on the individual’s or couple’s unique situation.
Ovulation Induction Hormones
Ovulation induction hormones help women who don’t ovulate regularly. Clomiphene citrate and letrozole are common oral meds. They stimulate hormones that trigger ovulation.
For those not responding to oral meds, injectable gonadotropins are suggested. These hormones directly stimulate the ovaries. This increases the chances of ovulation and conception.
Hormones for Uterine Lining Support
A healthy uterine lining is key for implantation and pregnancy. Progesterone is often given to support the lining, mainly in IVF treatments.
Progesterone helps create a good environment for embryo implantation. The timing and length of progesterone therapy vary based on the treatment plan.
Hormone Antagonists and Their Role
Hormone antagonists, like gonadotropin-releasing hormone (GnRH) antagonists, prevent early ovulation during treatments. They offer more control over egg retrieval timing. This reduces risks like ovarian hyperstimulation syndrome (OHSS).
GnRH antagonists prevent early ovulation. This optimizes fertility treatment timing, boosting conception chances.
Hormone treatments for fertility include ovulation induction, uterine lining support, and hormone antagonists. Each is vital for addressing different fertility aspects.
Hormone Treatment | Purpose | Common Medications |
Ovulation Induction | Stimulate ovulation | Clomiphene citrate, Letrozole, Gonadotropins |
Uterine Lining Support | Support implantation | Progesterone |
Hormone Antagonists | Prevent premature ovulation | GnRH antagonists |
“The advancements in hormone treatments have significantly improved fertility outcomes, giving hope to many who struggle with conception.”
— Medical Expert, Fertility Specialist
Oral Fertility Medications and Their Effectiveness
Oral fertility medications are key in treating infertility. They offer different options for those trying to conceive. These drugs help with ovulation problems and hormonal imbalances.
Clomiphene Citrate (Clomid) Protocol
Clomiphene Citrate, or Clomid, is a common oral fertility drug. It boosts hormone levels that help an egg mature and release (ovulation).
People take Clomiphene Citrate for five days. This starts on the third, fourth, or fifth day of their period. The usual dose is 50mg a day, but it can change based on how well it works and doctor advice.
Key benefits of Clomiphene Citrate include:
- It’s good for women with polycystic ovary syndrome (PCOS)
- It’s cheaper than other fertility treatments
- It has a long history of use
Letrozole (Femara) as an Alternative
Letrozole, or Femara, is another drug for ovulation. It was first used for breast cancer but works well for fertility. It lowers estrogen levels, which helps release FSH.
Studies show Letrozole might work better than Clomiphene Citrate, like for women with PCOS. People usually take 2.5mg to 5mg a day for five days, starting on day 3 of their period.
Advantages of Letrozole include:
- It’s less likely to cause multiple pregnancies than Clomiphene Citrate
- It’s good for those who don’t respond to Clomiphene Citrate
- It has fewer side effects related to estrogen
Bromocriptine for Prolactin Regulation
Bromocriptine treats high prolactin levels, which can stop ovulation and fertility. It works by acting like dopamine, which stops prolactin release.
By lowering prolactin, Bromocriptine helps restore normal ovulation and menstrual cycles.
Key points about Bromocriptine:
- It lowers prolactin levels and improves fertility
- The dose starts low and goes up to avoid side effects
- It’s important to check prolactin levels often to adjust the dose
In summary, drugs like Clomiphene Citrate, Letrozole, and Bromocriptine are key in treating fertility issues. Each drug has its own use, benefits, and side effects. Knowing these can help people make better choices for their fertility treatment.
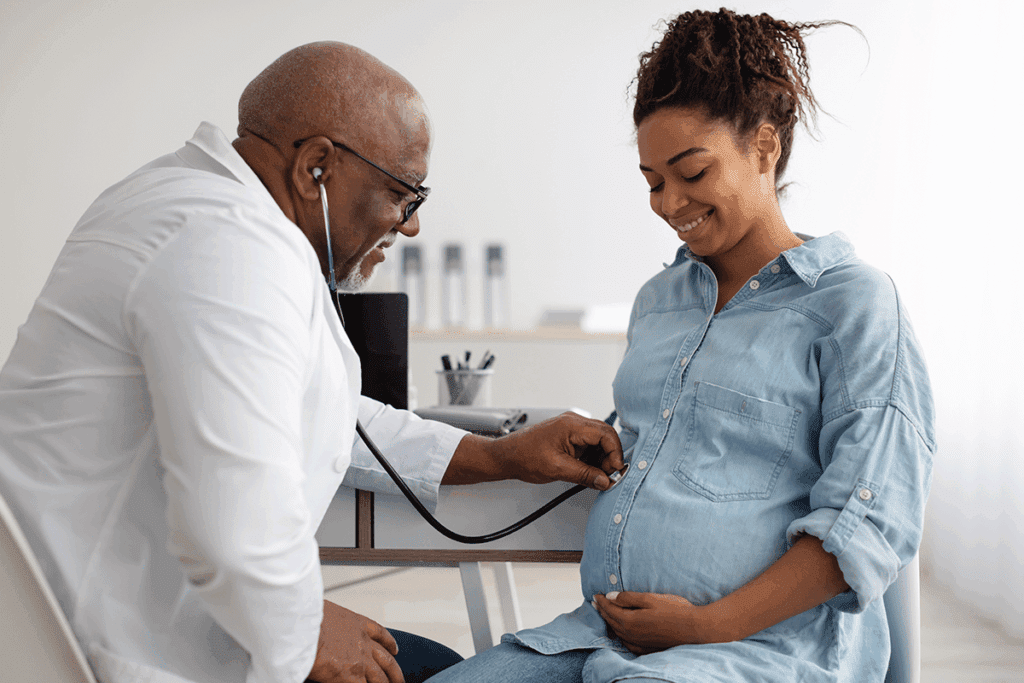
Injectable Fertility Hormone Protocols
Injectable fertility hormones are key in many fertility treatments. They help target specific fertility issues. This is very important in treatments like in vitro fertilization (IVF).
Gonadotropin Injections for Controlled Ovarian Stimulation
Gonadotropin injections are vital in fertility treatments, mainly for controlled ovarian stimulation (COS). They help the ovaries produce more eggs. This increases the chances of getting healthy eggs for fertilization.
The goal is to get as many eggs as possible without risking complications like ovarian hyperstimulation syndrome (OHSS).
There are different types of gonadotropins used, including follicle-stimulating hormone (FSH) and luteinizing hormone (LH) or a combination of both. The choice of gonadotropin and the dosage depends on individual patient factors, including ovarian reserve and response to previous stimulation.
Key Considerations for Gonadotropin Therapy:
- Monitoring follicle development through ultrasound and hormone level checks
- Adjusting dosages based on ovarian response
- Minimizing the risk of OHSS through careful patient selection and monitoring
Human Chorionic Gonadotropin (hCG) Trigger Shots
Human chorionic gonadotropin (hCG) trigger shots are important in IVF cycles. They help time egg retrieval. Administering hCG when follicles are ready triggers egg maturation.
“The timing of hCG administration is critical, as it ensures that egg retrieval occurs when the eggs are fully mature, hereby optimizing the chances of successful fertilization and pregnancy.”
Hormone | Function | Administration Timing |
Gonadotropins | Stimulate ovarian follicle growth | Daily injections for 8-14 days |
hCG | Trigger final egg maturation | Single injection, 34-36 hours before egg retrieval |
Self-Administration Techniques and Best Practices
Self-administering injectable fertility hormones needs proper technique. This ensures the treatment works well and is comfortable. Patients learn how to do this from their healthcare providers.
Best practices include:
- Rotating injection sites to prevent tissue damage
- Maintaining a clean and sterile environment during administration
- Properly disposing of needles and syringes
By learning self-administration techniques and following best practices, patients can manage their fertility treatment at home. This makes their treatment experience better.
Preparing Your Body for Hormone Treatment
To get the most out of hormone treatment, it’s key to get your body ready. This means doing health checks and making lifestyle changes. These steps are important for the best results and to feel better overall.
Pre-Treatment Health Assessments
Before starting hormone treatment, a detailed health check is needed. This includes:
- Comprehensive Medical History: Looking at your medical history to find any conditions that might affect treatment.
- Hormone Level Testing: Blood tests to check your hormone levels and find any imbalances.
- Ultrasound and Other Diagnostic Tests: Using imaging tests to check your reproductive health and find any problems.
These tests help doctors make the treatment fit your needs better. This makes the treatment more effective.
Nutritional Considerations and Supplements
What you eat is very important when getting ready for hormone treatment. Eating a balanced diet with the right nutrients helps your reproductive health. Here are some tips:
- Antioxidant-Rich Foods: Eating foods high in antioxidants, like fruits and veggies, helps reduce stress.
- Omega-3 Fatty Acids: Adding foods with omega-3s, like fish and nuts, helps balance hormones.
- Supplements: Some supplements, like folic acid and vitamin D, may be suggested to help with fertility and health.
Nutrient | Food Sources | Benefits |
Antioxidants | Fruits, Vegetables | Reduces oxidative stress |
Omega-3 Fatty Acids | Fish, Nuts, Seeds | Supports hormonal balance |
Folic Acid | Leafy Greens, Fortified Cereals | Essential for fetal development |
Lifestyle Modifications to Enhance Treatment Outcomes
Making lifestyle changes can really help hormone treatment work better. Here are some changes to consider:
- Maintaining a Healthy Weight: Keeping a healthy weight helps with hormone regulation and fertility.
- Reducing Stress: Doing things that reduce stress, like yoga or meditation, helps with hormonal balance.
- Avoiding Harmful Substances: Cutting down on alcohol, tobacco, and other harmful substances helps your reproductive health.
By making these lifestyle changes, you can make your body more responsive to hormone treatment.
Customized Treatment Approaches for Different Hormonal Profiles
Reproductive medicine has made big strides. Now, we can tailor treatments for different hormonal issues. Every person’s hormonal makeup is unique. Understanding these differences is key to successful fertility treatments.
Protocols for Anovulation and PCOS
Anovulation, or not ovulating, is a big reason for infertility. It’s often linked to Polycystic Ovary Syndrome (PCOS). Clomiphene citrate and letrozole help women with PCOS ovulate. The right choice depends on the patient’s health and history.
For those with PCOS who don’t respond to pills, gonadotropin injections might be suggested. These shots help the ovaries make eggs. This boosts the chances of ovulation and getting pregnant.
Treatment | Primary Use | Benefits |
Clomiphene Citrate | Ovulation Induction | Works well for many with PCOS, easy to use |
Letrozole | Ovulation Induction | Good for those not responding to Clomiphene, less chance of twins |
Gonadotropin Injections | Controlled Ovarian Stimulation | Helps those not responding to pills, precise control |
Treatments for Diminished Ovarian Reserve
Women with low ovarian reserve face special challenges. Minimal stimulation protocols or natural cycle IVF might be advised. These methods aim to avoid overstimulation and increase egg retrieval chances.
In some cases, pretreatment with estrogen or other hormones may be suggested. This can improve fertility treatment outcomes for women with low ovarian reserve.
Addressing Luteal Phase Defects with Progesterone
Luteal phase defects make it hard for an embryo to implant. Progesterone supplementation is a common fix. It supports early pregnancy stages.
The right timing and length of progesterone use vary. It depends on the patient’s needs and the fertility treatment.
Estrogen Antagonist Protocols and Their Benefits
Estrogen antagonists, like clomiphene citrate, stimulate ovulation. They block estrogen receptors in the hypothalamus. This boosts FSH production, helping follicles grow and ovulate.
These protocols are great for women with PCOS or ovulation issues. They’re simple, effective, and have fewer risks of twins compared to gonadotropin injections.
Success Rates and Statistics for Hormone Treatments
Knowing how well hormone treatments work is key for those trying to get pregnant. Hormone therapy is a big help in treating infertility. Its success rate is a big factor in choosing the right treatment.
Hormone therapy has shown to be very effective. For example, it can lead to a 29.72% success rate in the first cycle. Also, after more cycles, success rates can go up to 75.4%. These numbers show how hormone treatments can help people conceive.
First-Cycle Success Rates
First-cycle success rates are important. They show how well hormone treatments work right away. Studies show many people get pregnant in the first cycle. This is good news for those who have had trouble getting pregnant.
Recent data shows a 29.72% success rate in the first cycle. This means many people can get pregnant early in their treatment.
Cumulative Success Across Multiple Cycles
Cumulative success rates give a bigger picture. They show how well hormone treatments work over time. As people go through more cycles, their chances of getting pregnant go up.
Our data shows cumulative success rates can hit 75.4% after many cycles. This means even if it takes more than one cycle, the chances of success stay high.
Cycle Number | Cumulative Success Rate (%) |
1 | 29.72 |
2 | 45.10 |
3 | 60.25 |
4+ | 75.40 |
Factors That Influence Treatment Outcomes
Many things can affect how well hormone treatments work. These include age, health conditions, and the type of hormone therapy used.
“The interplay between hormonal balance and fertility is complex. Understanding the factors that influence treatment outcomes is key for better success rates.”
For example, age plays a big role because fertility drops with age. Also, conditions like PCOS and thyroid problems can affect results.
Healthcare providers can improve success rates by knowing these factors. They can tailor treatments to better meet individual needs.
Combining Hormone Treatments with Assisted Reproductive Technologies
Hormone treatments are key when paired with IUI and IVF. They help stimulate ovulation and improve the uterine environment. This makes it easier to conceive through these technologies.
Intrauterine Insemination (IUI) with Hormonal Support
IUI involves placing sperm directly into the uterus. Adding hormonal support makes it more effective. Hormones like clomiphene citrate and gonadotropins help stimulate ovulation. This increases the chances of successful fertilization.
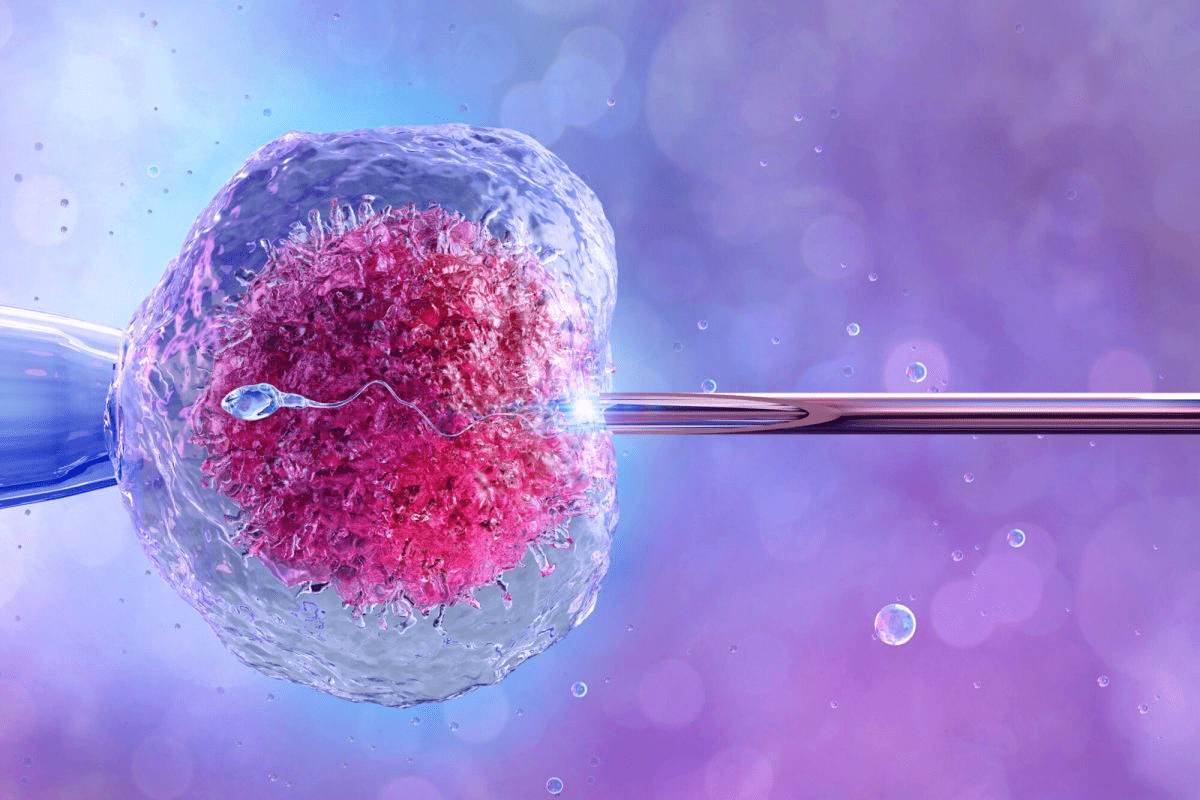
In Vitro Fertilization (IVF) Hormone Protocols
IVF fertilizes an egg outside the body and then transfers it to the uterus. Hormone protocols are vital for IVF to control ovarian stimulation. This ensures the production of multiple eggs.
Gonadotropin-releasing hormone (GnRH) agonists or antagonists prevent premature ovulation. This allows for better timing of egg retrieval. Gonadotropins followed by a trigger shot of hCG help with egg maturation.
Frozen Embryo Transfer and Hormonal Preparation
Frozen embryo transfer (FET) involves thawing and transferring previously frozen embryos. Hormonal preparation of the uterus is key for FET success. Estrogen and progesterone prepare the uterine lining, mimicking a natural cycle.
This hormonal support makes the uterine environment receptive to the embryo. It increases the chances of implantation and successful pregnancy.
Combining hormone treatments with assisted reproductive technologies greatly improves fertility outcomes. Tailoring hormone protocols to individual needs is essential for success.
Managing Side Effects and Risks of Fertility Hormone Treatments
Fertility hormone treatments offer hope for those trying to conceive. But, it’s important to know about and manage their side effects. These treatments can cause physical and emotional issues, and sometimes lead to serious problems like ovarian hyperstimulation syndrome.
Common Physical Side Effects and Coping Strategies
Fertility hormone treatments can cause physical side effects. These include bloating, breast tenderness, and mood swings. To deal with these, a healthy lifestyle is key. This includes eating well and exercising regularly. Staying hydrated also helps reduce side effects.
Some people may face more serious side effects, like ovarian enlargement or abdominal pain. If this happens, your healthcare provider can adjust your treatment to help.
Emotional and Psychological Support During Treatment
Fertility treatments can be emotionally tough. Patients often feel anxious, stressed, and experience mood swings. Seeking emotional support through counseling or support groups is very helpful. Your healthcare provider can also offer resources and advice for managing emotional challenges.
“The emotional journey of fertility treatment is just as important as the physical. Support and understanding can make a significant difference.” – Medical Expert, Fertility Specialist
Ovarian Hyperstimulation Syndrome: Prevention and Management
Ovarian Hyperstimulation Syndrome (OHSS) is a risk with fertility treatments. It happens when the ovaries get too big and swollen. Careful monitoring by your healthcare provider can help prevent or catch OHSS early.
- Risk factors for OHSS include young age, low body weight, and a history of OHSS.
- Symptoms to watch for include severe abdominal pain, nausea, vomiting, and shortness of breath.
- Prevention strategies may involve adjusting medication dosages or using alternative treatment protocols.
When to Contact Your Doctor About Complications
Knowing when to seek medical help is important during fertility treatment. If you have severe symptoms like persistent abdominal pain, heavy vaginal bleeding, or difficulty breathing, call your healthcare provider right away. Quick action can prevent serious problems.
Understanding the side effects and risks of fertility hormone treatments helps patients feel more confident in their journey. Always talk to your healthcare provider for personalized advice and care.
Conclusion: Navigating Your Fertility Journey with Hormone Treatments
Understanding hormone treatments can help you navigate your fertility journey. It empowers you to make informed decisions about your reproductive health.
We’ve looked at the science behind reproductive hormones and common causes of hormonal infertility. We’ve also discussed various treatment options, like oral medications and injectable hormone protocols.
Knowing about different hormone treatment approaches can help you tackle fertility challenges. It can also improve your chances of conceiving.
Hormone treatments are key in addressing fertility issues. Knowing your options and what to expect can guide your fertility journey.
Combining hormone treatments with other fertility options, like assisted reproductive technologies, can increase your chances of success. This way, you can achieve your dream of building a family.
FAQ
What is hormone treatment for infertility, and how does it work?
Hormone treatment for infertility uses medicines to balance or boost reproductive hormones. This helps with ovulation and fertility. It aims to fix hormonal imbalances, increase egg production, and get the uterus ready for implantation.
What are the common hormone treatments used for fertility?
Common treatments include Clomiphene Citrate and Letrozole for ovulation. Gonadotropin injections and hCG shots are also used. Progesterone supports the luteal phase, and estrogen antagonists are used in some cases.
How do I know if I need hormone treatment for infertility?
If you’re having trouble getting pregnant, get a full check-up. Tests like hormone panels and ultrasounds help find if hormone treatment is needed.
What are the possible side effects of fertility hormone treatments?
Side effects can be bloating, mood swings, and tender breasts. Serious risks like OHSS can happen with injectables. We help manage these side effects and risks.
Can hormone treatments be used with assisted reproductive technologies like IVF?
Yes, hormone treatments are often used with IVF. We customize hormone protocols to support the IVF process, improving success rates.
How long does hormone treatment for fertility typically last?
Treatment length varies based on individual needs. We adjust treatment as needed, usually for several cycles to achieve success.
Are there any lifestyle changes that can enhance the effectiveness of hormone treatment for fertility?
Yes, a healthy lifestyle can help. Eating well, exercising, and managing stress can support fertility and hormone treatment. We offer advice on nutrition and lifestyle.
Can estrogen help improve fertility?
Estrogen is key for fertility. In some cases, estrogen antagonist protocols can help. We tailor treatments based on individual hormonal needs.
What is the success rate of hormone treatment for fertility?
Success rates depend on age, fertility issues, and treatment. We provide personalized success rate information and discuss chances across multiple cycles.
How do I prepare for hormone treatment for fertility?
Preparing involves health checks, nutrition, and lifestyle changes. We guide you to prepare for treatment, improving outcomes and well-being.
References
World Health Organization. Hormone Treatment: A Guide to Pregnancy for Infertility. Retrieved from https://www.who.int/news-room/fact-sheets/detail/infertility