We know that hepatoblastoma, a rare liver cancer, mainly hits kids. It comes in different sizes, which really affects how well the treatment works.
The size of the tumor is key in figuring out how well a patient will do and what treatment they need. Hepatoblastoma tumors can be small, under 5 cm, and have a 97% chance of survival after five years. Or, they can be big, up to 25 cm.
It’s important to know how big and what kind of tumors are. This helps doctors find the best treatment. It also helps improve the liver cancer survival rate by age.
Key Takeaways
- Hepatoblastoma tumors vary significantly in size.
- Tumor size is a critical factor in prognosis and treatment.
- Small tumors (
- Large tumors can reach up to 25 cm.
- Accurate diagnosis is key for the best treatment plan.
Understanding Hepatoblastoma: A Complete Overview
To understand hepatoblastoma, we must first know what it is and its impact. It’s a rare and aggressive liver tumor mainly found in children. We’ll dive into its definition and how common it is to fully grasp this condition.
Definition and Epidemiology of Hepatoblastoma
Hepatoblastoma is a cancer of the liver that mostly hits kids, often in the first year and a half of life. It’s the top liver cancer in kids, making up a big part of liver cancers in young ones. It’s mostly seen in babies and toddlers.
Epidemiological Characteristics:
- Primarily affects children under 3 years old
- Most common liver cancer in pediatric populations
- Typically diagnosed within the first 18 months of life
- Has a slight male predominance
Knowing about hepatoblastoma’s spread helps catch it early. Accurate diagnosis and understanding its spread are key to treating it.
The importance of hepatoblastoma’s spread is in early detection and screening. Knowing who’s at risk helps doctors spot it sooner.
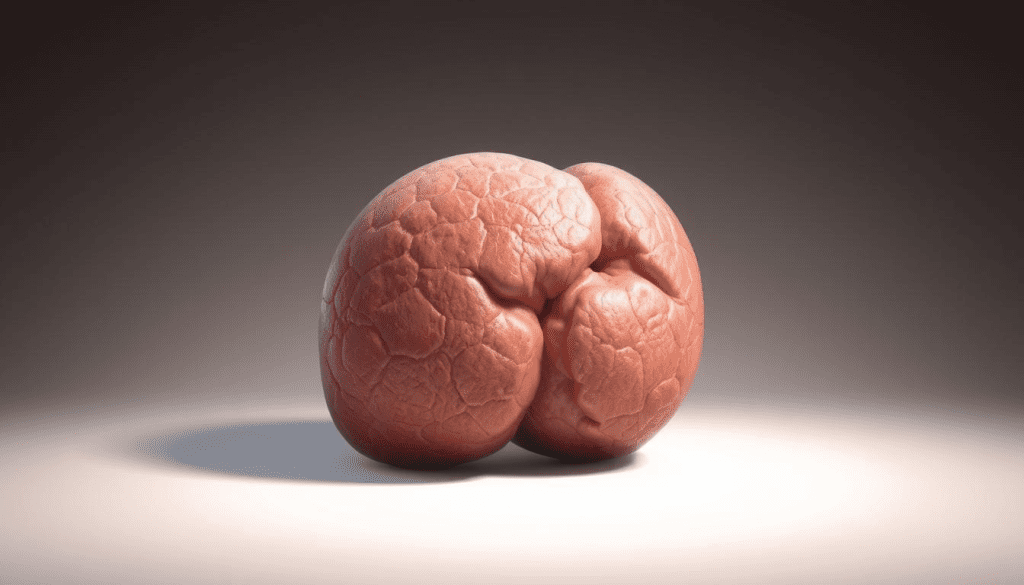
A liver lesion like hepatoblastoma is serious because it can grow and harm the liver. In kids, finding a liver tumor quickly is vital for their health.
We aim to give top-notch, caring care to those with hepatoblastoma. We know it’s a tough disease and our patients need all the support they can get.
Size Range of Hepatoblastoma Tumors
Hepatoblastoma tumors can vary greatly in size when first found. This size difference affects how they are treated and managed.
Some tumors are small, while others can grow up to 25 cm or more. These large tumors are hard to plan for and treat.
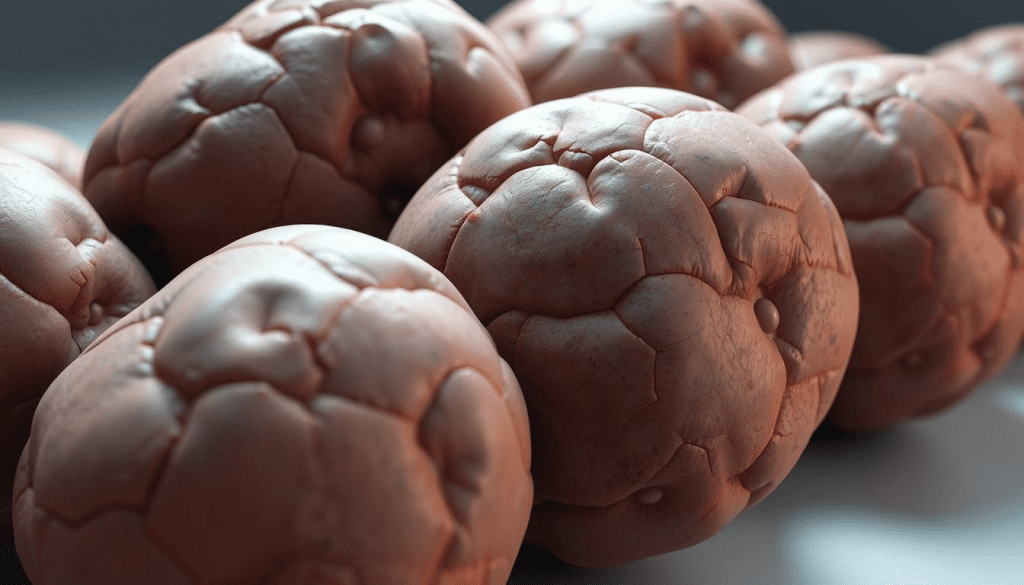
Extensive Tumors: Up to 25 cm and Beyond
Big hepatoblastoma tumors can take up a lot of the liver. Handling these tumors needs a team effort. This includes advanced imaging, special surgery plans, and custom chemotherapy.
Managing large tumors involves:
- Getting the tumor’s exact size and how much of the liver it affects
- Creating a treatment plan just for that patient
- Working together with surgeons, oncologists, and radiologists
- Looking into new treatments for tough cases
We handle complex cases of hepatoblastoma, including big tumors. Our team offers full care from start to finish.
The tumor’s size is key in figuring out the patient’s chances and treatment success. Knowing the size range helps us tailor care for each patient.
Factors Influencing Hepatoblastoma Tumor Size
It’s important to know what affects the size of a hepatic mass on liver. At our institution, we see big differences in tumor in liver sizes when patients first come in.
Age at Diagnosis and Growth Patterns
The age a patient is when they get diagnosed matters a lot. Young kids usually have smaller tumors in liver. Older kids might have bigger masses on the liver.
Early detection in young patients often means smaller lumps on liver. But, older kids might not get diagnosed until their lumps on liver are bigger. This makes treatment harder.
Biological Determinants of Tumor Growth
Genetic changes also play a big role in how fast and big a growth on liver tumor gets. Some genetic factors can make tumors grow faster, leading to bigger tumors in liver.
Our team looks at these genetic factors when making treatment plans. We try to understand why tumors grow the way they do. This helps us make plans that fit each patient’s needs.
In short, the size of a hepatoblastoma tumor depends on age and genetics. Knowing these factors helps us treat patients better.
Advanced Imaging Techniques for Measuring Hepatoblastoma
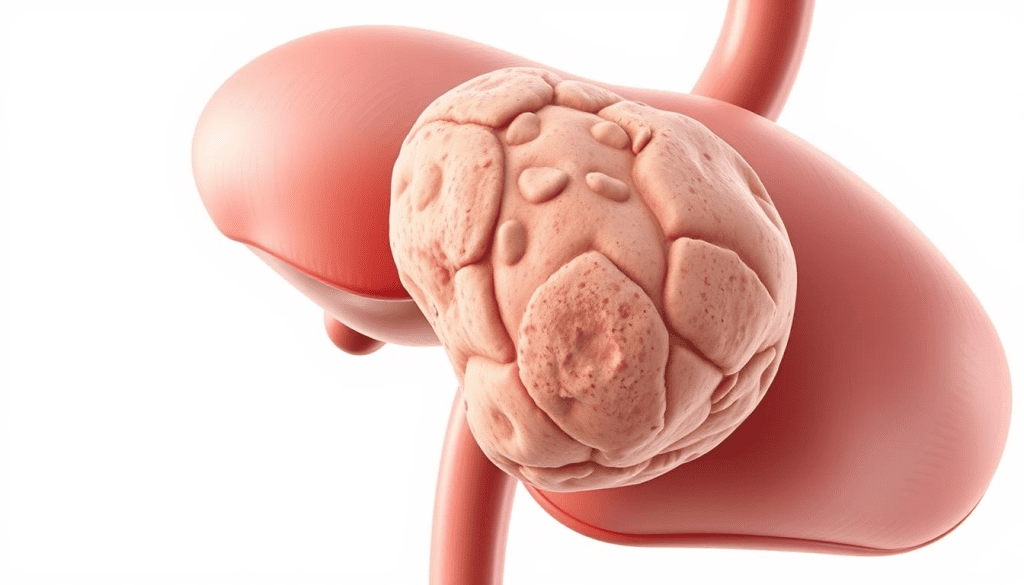
We use top-notch imaging to check the size and spread of hepatoblastoma tumors in the liver. MRI and CT scans are key in measuring these tumors accurately.

Measuring hepatoblastoma right is key for treatment planning. When tumors are found in multiple sites in the liver, knowing their size and location is critical. This helps in planning surgery and understanding the patient’s outlook.
Clinical Implications of Multiple Tumor Sites
Having tumors in multiple sites makes treatment more complex. It needs a detailed plan for surgery and chemotherapy. Advanced imaging helps pinpoint the tumors’ exact spots and sizes, leading to a more personalized treatment.
When there are multiple tumor sites, the team must think about the liver’s function and how treatment might affect the patient’s life. Our team of experts works together to create a detailed treatment plan.
Advanced imaging is not just for the first check-up. It also helps track how well treatment is working. This allows for changes in the treatment plan as needed. This flexible approach is key to better outcomes for patients with hepatoblastoma.
The PRETEXT Staging System and Tumor Size
The PRETEXT staging system is key in checking how much of the liver is affected by hepatoblastoma. At our place, we use it to make treatment plans and give full care.
Assessing Liver Involvement with PRETEXT
The PRETEXT system sorts tumors by how many liver sectors they touch. This helps us see how much of the liver is involved and plan the best treatment.
Key aspects of the PRETEXT staging system include:
- Evaluation of the number of liver sectors involved by the tumor
- Assessment of the tumor’s extent and spread within the liver
- Consideration of vascular involvement and possible metastasis
With the PRETEXT system, we can figure out the stage of hepatoblastoma. Then, we can make a good treatment plan.
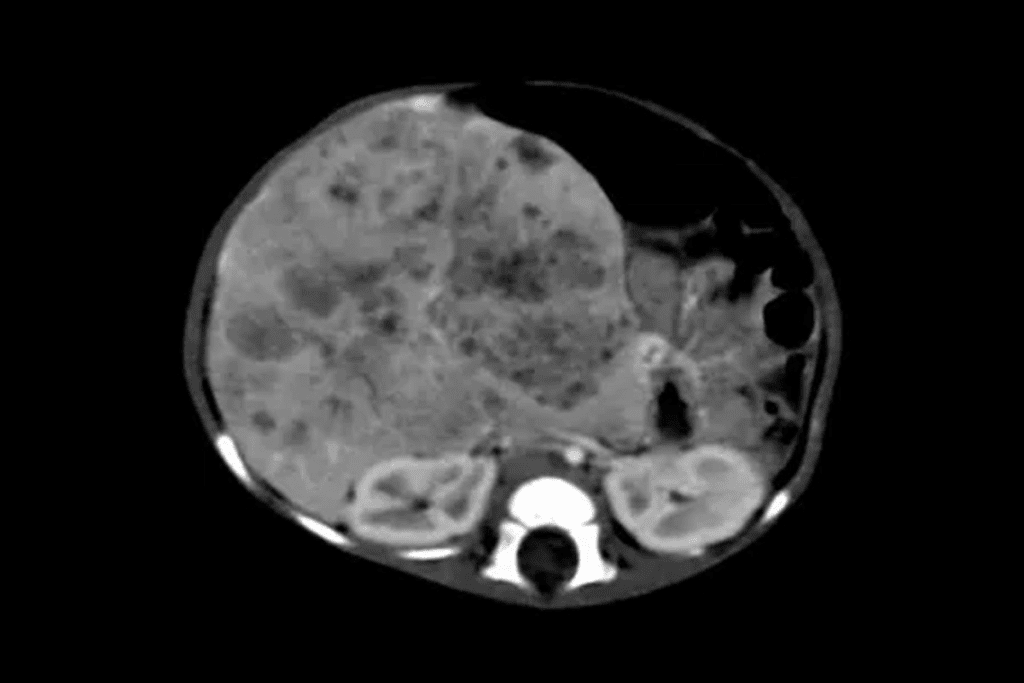
Correlation Between Tumor Size and PRETEXT Stage
Tumor size is a big deal in figuring out the PRETEXT stage. This stage affects treatment plans and how well a patient might do. Bigger tumors usually mean a higher PRETEXT stage, showing more liver involvement.
The relationship between tumor size and PRETEXT stage can be summarized as follows:
- Small tumors are often early PRETEXT stages (I or II), showing little liver involvement.
- Big tumors usually mean more advanced PRETEXT stages (III or IV), showing a lot of liver involvement.
Knowing this link is key for doctors to plan the right treatment and guess how a patient will do.
Impact of Tumor Size on Prognosis and Survival Rates
The size of a hepatoblastoma tumor greatly affects a patient’s chances of survival. At our institution, we’ve seen how tumor size impacts outcomes. We stress the need for early detection and customized treatment plans to boost survival chances.
Small Tumors and 97% Five-Year Survival Rate
Patients with small tumors, under 5 cm, have a 97% five-year survival rate. This shows how vital early detection is. Small tumors tend to respond well to treatment, leading to better results for patients. Catching the disease early is key to better survival rates.
Challenges and Outcomes with Large Hepatoblastoma Masses
Larger tumors, on the other hand, are harder to treat and have lower survival rates. They can be tough to remove surgically and complicate chemotherapy. Treating big tumors needs a multidisciplinary approach, combining surgery, medicine, and support care. Despite these hurdles, new treatments are helping patients with big tumors live longer.
Our experience highlights the importance of understanding how tumor size, treatment, and patient factors interact. By taking a personalized treatment approach, we can improve outcomes for patients with both small and large tumors.
Multidisciplinary Approach to Treating Hepatoblastoma
Treating hepatoblastoma requires a team effort. This includes surgery, chemotherapy, and new treatments. At Livhospital.com, we focus on a detailed approach to tackle this tough condition.
Surgical Planning Based on Tumor Size
Planning surgery is key in treating hepatoblastoma. The size of the tumor is very important. Larger tumors need more complex surgery, like liver removal or transplant. We create treatment plans that fit each patient’s needs.
The tumor’s size and where it is affect the surgery plan. MRI and CT scans help us plan. Knowing the tumor’s size and where it is helps us succeed in surgery.
Chemotherapy Protocols for Different Tumor Dimensions
Chemotherapy is a big part of treating hepatoblastoma. We tailor the treatment to the tumor’s size and type. Chemotherapy helps shrink the tumor before surgery, making it easier to remove. We use proven chemotherapy plans and adjust them as needed.
We watch how well the chemotherapy works with regular scans and tests. We change the treatment plan if needed to get the best results and reduce side effects.
Innovative Therapies for Challenging Cases
For tough cases of hepatoblastoma, new treatments offer hope. Targeted and immunotherapies are being tested as new options. We keep up with the latest treatments and trials to help our patients.
We’re dedicated to giving our patients the best care for hepatoblastoma. We use surgery, chemotherapy, and new treatments together. Our goal is to improve our patients’ chances of success.
Conclusion: Advancing Care for Hepatoblastoma Patients
The size of hepatoblastoma tumors is key in deciding treatment and outcomes. At Livhospital.com, we are dedicated to improving care for these patients. We aim to offer top-notch healthcare and support for patients from around the world, following the latest standards.
We are always looking to improve and provide ethical, high-quality care. This lets us use the latest research to help children with hepatoblastoma. We aim to better treatment results and support families through tough times.
Our commitment to excellent care is shown in our team approach to treating hepatoblastoma. We believe in working together and using the newest medical science. This way, we can make a big difference in our patients’ and their families’ lives.
FAQ
What is hepatoblastoma?
Hepatoblastoma is a rare and aggressive liver tumor. It mainly affects children, often diagnosed in the first 18 months of life.
How big can hepatoblastoma tumors be?
Tumors can range from small, under 5 cm, to large, up to 25 cm or more.
What is the significance of tumor size in hepatoblastoma?
The size of the tumor greatly affects treatment and prognosis. Smaller tumors usually have better outcomes, while larger ones are more challenging to treat.
What is the PRETEXT staging system?
The PRETEXT system is used to assess liver involvement in hepatoblastoma. It categorizes tumors based on how many liver sectors they involve.
How does tumor size affect prognosis and survival rates in hepatoblastoma?
Tumor size is a key factor in survival. Tumors under 5 cm have a 97% five-year survival rate. Larger tumors have lower survival rates.
What is the role of advanced imaging techniques in hepatoblastoma?
Advanced imaging is vital for accurately measuring and assessing tumors. This information is essential for staging and treatment planning.
How is hepatoblastoma treated?
Treatment involves a team effort, including surgery, chemotherapy, and new therapies. Plans are tailored based on tumor size and characteristics.
What are the challenges in treating large hepatoblastoma masses?
Large tumors require complex surgeries and often have lower survival rates. Early detection and tailored treatments are critical.
What is the importance of early detection in hepatoblastoma?
Early detection is key to better outcomes. Smaller tumors have better prognosis and survival rates.
What is the hepatic tumor?
A hepatic tumor is an abnormal growth in the liver. It can be benign or malignant, with hepatoblastoma being malignant.
What does a mass on the liver mean?
A liver mass is an abnormal growth that needs evaluation. It can be caused by conditions like hepatoblastoma and requires proper treatment.
References
Agrawal, S., & Balamurugan, V. (2020). Laparoscopic versus open inguinal hernia repair: A meta-analysis of randomized controlled trials. Journal of Minimal Access Surgery, 16(1), 1“9.https://doi.org/10.4103/jmas.jmas_35_19
Centers for Disease Control and Prevention. (2024). Facts about birth defects.https://www.cdc.gov/ncbddd/birthdefects/facts.html
Hockenberry, M. J., Wilson, D., & Rodgers, C. C. (2019). Wong’s nursing care of infants and children (11th ed.). Mosby.https://www.elsevier.com/books/wongs-nursing-care-of-infants-and-children/hockenberry/978-0-323-54939-5
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). (2023). Patient information on hernia repair.https://www.sages.org/publications/patient-information/patient-information-for-hernia-repair-from-sages/



































