How do doctors rule out cancer? Colorectal cancer is a big problem worldwide. Finding it early is key to treating it well. Doctors use many tests and procedures to find cancer.
Doctors use different ways to check for cancer. They start with simple tests and might do more detailed tumor biopsy procedures. Finding cancer early is important for better treatment results.
Key Takeaways
- Early detection is key for treating cancer well.
- Many tests help find cancer.
- Doctors need a detailed plan for accurate diagnosis.
- Tumor biopsy procedures are used for sure diagnosis.
- Cancer screening tests help find cancer early.

The Importance of Cancer Detection and Prevention
Finding cancer early is key because it makes treatment more likely to work. Cancer happens when cells grow out of control. It can come from genes, lifestyle, and the environment. Knowing how cancer starts and what increases its risk helps prevent and detect it early.
What is cancer and how does it develop?
Cancer starts when cells grow and spread without control. This can happen due to genes or the environment. For example, UV rays or harmful chemicals can cause genetic changes. Lifestyle choices, like smoking and diet, also play a big part.
Why early detection improves outcomes
Finding cancer early means treatment can start sooner. This makes treatment more effective. Doctors might use surgery, chemo, or radiation, depending on the cancer type and stage. Early detection also lowers the chance of cancer spreading.
Risk factors that prompt diagnostic evaluation
Some risk factors mean you might need to see a doctor sooner. These include family history, smoking, infections, and exposure to harmful substances. People with a family history of cancer or smokers should get checked regularly. Knowing these risks helps find who needs early detection.
| Risk Factor | Description | Implication for Cancer Detection |
| Family History | Having close relatives with a history of cancer | Increased risk; regular screening recommended |
| Smoking | Use of tobacco products | Higher risk of lung and other cancers; screening advised |
| Certain Infections | Infections like HPV and Hepatitis B | Increased risk of specific cancers; vaccination and screening recommended |
First Steps in the Cancer Diagnostic Process
The journey to find out if a patient has cancer starts with a detailed first step. This step is all about gathering info and doing initial checks. These help decide what tests to do next.
Comprehensive Medical History Assessment
Getting a full medical history is key in finding cancer. It’s about learning about the patient’s health now and in the past. It also looks at family history and lifestyle. This helps spot risks and pick the right tests.
Important parts of a full medical history include:
- Past medical conditions and surgeries
- Family history of cancer
- Exposure to known carcinogens
- Lifestyle factors such as smoking and diet
Physical Examination Techniques
A physical check-up is also vital in the early stages. Doctors use different methods to look for signs of cancer. The method used depends on the type of cancer suspected.
For example, a breast check is done for breast cancer. A prostate check is done for prostate cancer.
Identifying Warning Signs and Symptoms
Spotting early signs of cancer is very important. Both patients and doctors need to know about body changes that could mean cancer. Common signs include losing weight without trying, feeling pain all the time, and changes in bowel or bladder habits.
| Symptom | Possible Cancer Association |
| Unexplained Weight Loss | Various cancers, including pancreatic and lung cancer |
| Changes in Bowel Habits | Colorectal cancer |
| Unusual Bleeding | Cervical, endometrial, or other cancers |
Spotting these signs early can lead to quicker diagnosis and treatment. This can greatly improve chances of recovery.
Routine Cancer Screening Guidelines
Regular cancer screenings are recommended based on age and individual risk factors. This proactive approach to health care can significantly improve the chances of detecting cancer at an early stage when it is more treatable.
Age and Risk-Appropriate Screening Recommendations
Cancer screening guidelines vary based on age, gender, and individual risk factors. For instance, guidelines for breast cancer screening recommend that women with a family history of breast cancer begin screening earlier than those without such history.
General Screening Recommendations:
- Breast cancer screening typically starts at age 40 or 45.
- Colorectal cancer screening begins at age 45.
- Cervical cancer screening starts at age 21.
Differences Between Screening and Diagnostic Testing
It’s important to understand the difference between screening and diagnostic testing. Screening tests are used to detect cancer in people who are asymptomatic. On the other hand, diagnostic tests are used to confirm the presence of cancer in individuals who are showing symptoms or have had an abnormal screening test result.
| Test Type | Purpose | Population |
| Screening Tests | Detect cancer early | Asymptomatic individuals |
| Diagnostic Tests | Confirm cancer presence | Symptomatic individuals or those with abnormal screening results |
Limitations and Benefits of Cancer Screening
Cancer screening has both benefits and limitations. The primary benefit is early detection, which can lead to more effective treatment and improved survival rates. But, screening can also result in false positives, leading to unnecessary anxiety and additional testing.
Understanding these aspects of cancer screening is vital for making informed decisions about one’s health. By knowing the guidelines, the differences between screening and diagnostic tests, and the possible outcomes, individuals can better navigate the cancer screening process.
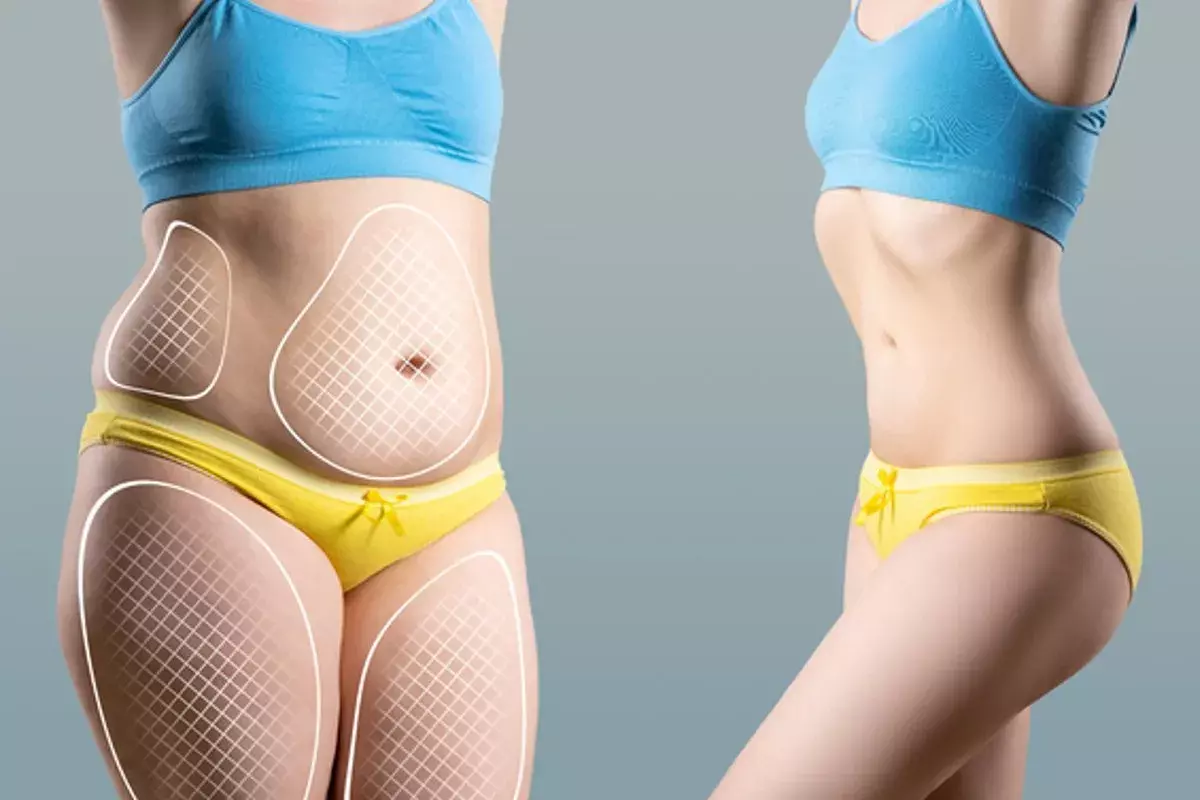
Advanced Imaging Technologies for Cancer Detection
Advanced imaging technologies have changed how we fight cancer. They help doctors find cancer early and accurately. These tools are key for diagnosing, staging, and planning cancer treatments.
X-rays and their role in initial assessment
X-rays are often the first step in checking for cancer. They work well for finding tumors in bones and lungs. Digital X-ray technology makes images clearer and uses less radiation than old methods.
CT scans: When and why they’re ordered
Computed Tomography (CT) scans are used when X-rays aren’t enough. They’re great for finding tumors in organs like the liver, pancreas, and kidneys. CT scans give cross-sectional images that show tumor size and spread.
MRI scans for detailed tissue examination
Magnetic Resonance Imaging (MRI) scans show soft tissues in detail. They’re essential for finding cancers in the brain, spine, and breast. MRI scans help tell different soft tissue tumors apart and see how far cancer has spread.
PET scans for metabolic activity assessment
Positron Emission Tomography (PET) scans check how tissues work. They spot cancerous tissues because they work harder than normal tissues. PET scans are often paired with CT scans (PET-CT) for a full picture.
These advanced imaging tools are vital in the battle against cancer. They help find cancer early, diagnose it accurately, and plan treatments well. Knowing how each imaging method works helps doctors make better care plans for patients.
Blood Tests and Laboratory Analysis in Cancer Diagnosis
Blood tests are key in finding cancer. They give clues that help doctors choose the right treatment. By looking at blood samples, doctors can learn a lot about a patient’s health, including if they might have cancer.
Complete Blood Count and Basic Metabolic Panels
A complete blood count (CBC) checks different parts of the blood. It looks at red and white blood cells and platelets. If these counts are off, it could mean cancer or another health problem.
A basic metabolic panel (BMP) checks things like electrolyte levels and kidney function. These can be affected by cancer or its treatment.
Tumor Markers and Their Significance
Tumor markers are substances in the blood, urine, or tissues of some cancer patients. They help track how cancer is growing, if it’s coming back, and how well treatment is working. For example, PSA is used for prostate cancer and CA-125 for ovarian cancer.
Circulating Tumor DNA Testing
Circulating tumor DNA (ctDNA) testing is a blood test that looks for DNA from tumors. It’s a way to check on tumor genetics without surgery. This helps doctors choose the right treatments and see if they’re working.
Proteomics Blood Tests: The Cutting Edge
Proteomics blood tests look at proteins in the blood for cancer signs. This new tech could lead to finding cancer early and treating it in a way that’s just right for each person. It might change how we find and treat cancer.
In short, blood tests and lab work are very important in finding and treating cancer. They help doctors understand what’s going on in a patient’s body. This leads to better diagnoses and treatment plans.
Organ-Specific Cancer Screening Methods
Organ-specific cancer screening has changed how we find cancer early. This has made treatments more effective. It’s important to know the different tests for each organ.
Mammography and Breast Imaging
Mammograms are key for finding breast cancer early. Women over 40 should get a mammogram every year. But, the age might change based on your risk.
New breast imaging like 3D mammography and MRI help find cancer better. They are great for women with dense breasts.
Colonoscopy and Colorectal Cancer Screening
Colonoscopy is the best way to find and remove polyps before they turn into cancer. Start screening at 45 if you’re at average risk. You’ll need to go every 10 years if you’re healthy.
Other tests like fecal occult blood tests (FOBT) and CT colonography are options. They’re good for those who can’t or don’t want to have a colonoscopy.
Pap Smears and HPV Testing
Pap smears have been key in finding cervical cancer for years. HPV testing has made them even better. Women aged 30 to 65 should get tested every 5 years with both.
HPV vaccines have also helped lower cervical cancer rates. This shows how important it is to prevent cancer.
PSA Testing and Prostate Examinations
PSA tests check for prostate cancer in the blood. But, there are worries about finding too many cancers. Talk to your doctor about the pros and cons before getting tested.
Digital rectal examination (DRE) is also used to screen for prostate cancer. It’s often done with PSA tests.
| Cancer Type | Screening Method | Recommended Starting Age |
| Breast Cancer | Mammography | 40 |
| Colorectal Cancer | Colonoscopy | 45 |
| Cervical Cancer | Pap Smear/HPV Testing | 21 (Pap Smear) |
| Prostate Cancer | PSA Testing | Discuss with healthcare provider |
Screening for specific organs is key in fighting cancer. Knowing your screening options and following guidelines can greatly reduce cancer risk.
The Biopsy Procedure: Gold Standard for Diagnosis
The biopsy procedure is the top choice for finding cancer. It helps doctors know if cancer is there and what kind it is.
Types of Biopsies and When They’re Performed
There are many types of biopsies, each for different situations. The right one depends on where the tumor is, the patient’s health, and more.
- Needle Biopsy: Uses a needle to get tissue or fluid. It’s less invasive and good for tumors that are easy to reach.
- Surgical Biopsy: Removes part or all of the tumor. Needed for bigger samples or hard-to-reach tumors.
- Endoscopic Biopsy: Uses an endoscope to get tissue from inside the body. Often for cancers in the gut.
- Incisional Biopsy: Takes a part of the tumor. Used for big tumors.
- Excisional Biopsy: Removes the whole tumor or affected area. Good for skin cancers or small tumors.
What Happens During a Biopsy Procedure
Patients might get local or general anesthesia for a biopsy. This depends on the type and where the tumor is.
The steps are:
- Preparation: The area is cleaned and ready.
- Anesthesia: The area is numbed with local anesthesia.
- Sampling: The biopsy needle or tool gets the tissue sample.
- Post-procedure: The area is bandaged, and the patient is watched for any problems.
Understanding Pathology Reports
After the biopsy, the sample goes to a lab for study. The report gives key details about the sample, like:
- Tumor Presence: If cancer cells are there.
- Tumor Type: What kind of cancer it is, like carcinoma or sarcoma.
- Grade: How much the tumor cells look like normal cells.
- Stage: How big the cancer is.
| Report Component | Description | Importance |
| Tumor Presence | Shows if cancer cells are found | Key for diagnosis |
| Tumor Type | Tells the cancer type | Helps decide treatment |
| Tumor Grade | Shows how abnormal the cells are | Affects how well the patient will do |
AI-Assisted Pathology Interpretation
AI is now helping with pathology, making diagnoses faster and more accurate.
AI can:
- Look at big data to find patterns.
- Help pathologists spot problems.
- Give exact data to support the diagnosis.
AI in pathology is a big step forward. It could make diagnoses better and help patients more.
Understanding the Cancer Diagnostic Process
Diagnosing cancer is a tough task. It uses medical history, physical checks, and new tech. This journey has many steps, from first symptoms to diagnosis. It needs a team effort from different doctors.
The Diagnostic Pathway from Symptoms to Diagnosis
The first step is when a patient tells their doctor about symptoms. The doctor will take a detailed medical history and do a physical check. This helps find any signs of cancer.
If something looks off, the doctor might do tests like X-rays or blood tests. These tests help get more info.
If tests hint at cancer, a biopsy might be needed. A biopsy looks at tissue or cells closely. It’s the best way to know if cancer is there.
Multidisciplinary Approach to Cancer Diagnosis
Diagnosing cancer is a team effort. It involves many doctors working together. This team includes primary care doctors, radiologists, pathologists, surgeons, and oncologists.
A radiologist looks at scans to find problems. A pathologist checks tissue samples for cancer. This teamwork makes sure all parts of the patient’s health are looked at. This leads to a more accurate diagnosis.
Timeframes and Expectations During Diagnosis
How long it takes to get a cancer diagnosis varies. It depends on the cancer type, how complex the case is, and the tests needed. It can take from a few days to weeks.
| Diagnostic Step | Typical Timeframe | Description |
| Initial Assessment | 1-2 days | Medical history and physical examination |
| Imaging Studies | 1-7 days | X-rays, CT scans, MRI, etc. |
| Biopsy and Pathology | 3-14 days | Examination of tissue or cells for cancer |
| Diagnosis Confirmation | 1-3 days | Final diagnosis based on all test results |
Knowing how cancer is diagnosed can help patients feel less anxious. By understanding what’s happening, patients can better handle their journey. They can make informed choices about their care.
The Cancer Staging Process
After finding out you have cancer, the next step is to figure out how far it has spread. This is called cancer staging. It’s a key part of treatment planning and helps doctors know how serious the cancer is.
TNM Classification System Explained
The TNM system is a common way to stage cancer. TNM means Tumor, Node, and Metastasis. It gives a detailed look at how far the cancer has spread.
- Tumor (T): This part talks about the size of the tumor and if it has grown into nearby tissue.
- Node (N): It shows if the cancer has reached the lymph nodes nearby and how far it has spread.
- Metastasis (M): This part tells if the cancer has moved to other parts of the body.
By looking at these three parts, doctors can find out the cancer’s stage. This is very important for choosing the right treatment.
How Staging Influences Treatment Decisions
The stage of cancer is very important for treatment choices. It tells doctors if the cancer is just in one place or if it has spread. This helps decide what treatment to use.
For example, if the cancer is in its early stages, doctors might suggest surgery or radiation. But if it’s more advanced, they might recommend chemotherapy or targeted therapy.
Additional Factors in Cancer Assessment
While the TNM system is key, other things also play a role in cancer assessment and treatment planning. These include:
- Tumor grade: This is what cancer cells look like under a microscope. It shows how fast the cancer might grow.
- Biomarkers: These are special proteins or genes that give clues about the cancer’s behavior and how it might react to treatment.
- Patient’s overall health: The patient’s overall health and any other health issues they might have can also affect treatment choices.
By looking at these factors along with the cancer stage, doctors can make a treatment plan that fits the patient’s needs best.
How Doctors Definitively Rule Out Cancer
Doctors use a mix of medical history, physical exams, and advanced tests to rule out cancer. This detailed method is key to giving patients accurate diagnoses and easing their worries.
Criteria for Excluding Cancer Diagnosis
To rule out cancer, doctors look at test results, symptoms, and medical history. A negative test result and no cancer symptoms can greatly lower the chance of cancer.
The rules for not having cancer are strict. They include:
- Normal results from imaging tests like X-rays and CT scans
- Negative biopsy results, when needed
- A medical history with no risk factors or past cancers
- Lab tests, like blood work, that are normal
Understanding False Negatives and Their Implications
A false negative happens when a test says there’s no cancer when there is. It’s important for doctors and patients to understand this, as it can delay finding cancer and affect treatment.
False negatives can be caused by:
- The cancer’s stage, with early stages harder to miss
- The type of test used, with some being less accurate
- Errors in testing or reading results
Follow-up Protocols After Negative Results
After getting negative results, doctors suggest follow-up steps. These steps can include regular check-ups, more tests, or watching symptoms.
These follow-ups are based on the person’s risk factors, medical history, and tests. This approach helps catch any changes early that might mean cancer or other health problems.
When to Seek a Second Opinion
Patients might wonder when to get a second opinion on their cancer diagnosis. A second opinion can offer more confidence or a different view on diagnosis and treatment.
Getting a second opinion is a good idea in these cases:
- When there’s doubt about the diagnosis
- If the diagnosis is rare or complex
- When looking at treatment options and wanting to explore all choices
Monitoring After Cancer Treatment
Monitoring after cancer treatment is key for survivors. It helps doctors spot and handle problems early. This care is essential for catching cancer back and managing treatment side effects.
Surveillance Protocols for Cancer Survivors
Cancer survivors need a custom plan for follow-up care. This plan depends on their cancer type, treatment, and risk factors. Surveillance protocols include regular check-ups, imaging, and lab tests.
For example, breast cancer survivors might get regular mammograms and breast exams. Those who had colon cancer might need colonoscopies and CT scans.
Minimal Residual Disease Detection
Minimal residual disease (MRD) means a few cancer cells might stay after treatment. Finding MRD is important because it shows a higher chance of cancer coming back. New tests like liquid biopsies help find MRD.
Liquid biopsies check blood for cancer DNA. This is less painful than old tissue biopsies. It helps see if cancer cells are left behind.
Recurrence Monitoring Strategies
How to watch for cancer coming back changes based on the cancer and treatment. Doctors often use imaging like CT scans and PET scans. They also check tumor markers in lab tests.
| Cancer Type | Monitoring Strategy | Frequency |
| Breast Cancer | Mammograms, Clinical Breast Exams | Annually or as recommended |
| Colorectal Cancer | Colonoscopy, CT Scans | Every 3-5 years or as recommended |
| Lung Cancer | CT Scans, PET Scans | Every 6-12 months or as recommended |
By using these plans, doctors can catch problems early. This helps improve life for cancer survivors.
Navigating the Emotional Aspects of Cancer Testing
Cancer testing is more than just a medical process. It’s a deeply emotional journey for patients and their families. The fear and uncertainty of a possible cancer diagnosis can be very tough to handle.
Coping with Anxiety During the Diagnostic Process
The wait between getting tested and hearing the results can be very stressful. Patients often feel heightened anxiety because they don’t know what’s going to happen.
Effective coping strategies include:
- Learning as much as you can about the testing process
- Reaching out to family, friends, or support groups for help
- Trying activities that help reduce stress, like meditation or yoga
Communicating with Your Healthcare Team
Talking openly with your healthcare team is very important. Patients should feel free to ask about their tests, diagnosis, and treatment options.
“Effective communication is the key to reducing anxiety and ensuring that patients receive the care that is right for them.” – Oncologist
Here’s what patients can do:
- Write down questions to ask during appointments
- Have a family member or friend there for support
- Ask for a second opinion if they’re unsure about their diagnosis or treatment
Support Resources for Patients and Families
There are many support resources for patients and their families to deal with the emotional side of cancer testing.
| Resource | Description |
| Cancer Support Groups | Places where people can share their experiences and get support from others facing similar challenges. |
| Online Forums | Spaces for asking questions, sharing information, and connecting with others. |
| Counseling Services | Professional help to deal with the emotional impact of cancer testing. |
Conclusion: The Future of Cancer Diagnostics
The future of cancer diagnostics is changing fast. New technologies like artificial intelligence and liquid biopsies are making a big difference. They help find cancer early and treat it more accurately.
Testing for cancer is getting better too. Next-generation sequencing and proteomics analysis are helping us understand tumors better. This means treatments can be more targeted and effective.
Using these technologies in hospitals is making diagnosis faster and more accurate. For example, AI helps pathologists spot tiny details in tissue samples. This reduces mistakes and improves diagnosis.
Looking ahead, better cancer diagnostics are key to fighting cancer. With these advancements, doctors will be able to find cancer early. This leads to better treatment and a brighter future for those with cancer.
FAQ
What is the first step in diagnosing cancer?
The first step is a detailed medical history and physical check. This helps find any signs or symptoms that might point to cancer.
What is the difference between screening and diagnostic testing for cancer?
Screening tests look for cancer in people without symptoms. Diagnostic tests confirm or rule out cancer in those with symptoms or abnormal screening results.
What are some common cancer screening tests?
Common tests include mammograms for breast cancer, colonoscopies for colon cancer, and Pap smears for cervical cancer. There’s also PSA testing for prostate cancer.
How do doctors use imaging technologies to detect cancer?
Doctors use X-rays, CT scans, MRI scans, and PET scans. These help see tumors and check their size, location, and activity.
What is a biopsy, and why is it considered the gold standard for cancer diagnosis?
A biopsy removes tissue for a microscope check. It’s the top choice for diagnosing cancer because it gives a clear answer.
What is the TNM classification system used for?
The TNM system stages cancer. It looks at the tumor size (T), nearby lymph nodes (N), and if it has spread (M).
How do doctors determine if cancer has been ruled out?
Doctors check test results, like imaging and biopsies. They also look at symptoms and medical history to see if cancer is ruled out.
What is minimal residual disease detection, and why is it important?
It’s finding small cancer cells left after treatment. It’s key because it shows the risk of cancer coming back and helps plan treatment.
How can patients cope with anxiety during the diagnostic process?
Patients can talk openly with their doctors. They can also get support from loved ones and use counseling or support groups.
What advancements are being made in cancer diagnostics?
New tech like liquid biopsies and AI in pathology is coming. These can make cancer detection more accurate and faster.
What is the role of circulating tumor DNA testing in cancer diagnosis?
It’s a blood test that finds DNA from cancer cells. It helps track cancer, find small amounts left after treatment, and guide treatment.
How do doctors use tumor markers in cancer diagnosis?
Tumor markers are substances from cancer cells. Doctors use tests to watch cancer growth, find it again, and see how treatment is working.