Last Updated on November 17, 2025 by Ugurkan Demir

Blood cancer, also known as hematologic cancer or blood cell cancer, is a group of cancers. They start in the bone marrow or lymphatic system and affect blood cell production and function. Understanding how do you get blood cancer helps people learn about its causes, risk factors, and prevention.
The Cleveland Clinic says blood cancer is a big threat to our health. It targets our blood cells. These cells are key because they give us energy, help fight infections, and stop too much bleeding.
It’s important to know the basics of blood cancer. This knowledge helps patients and their families. We will look at how it affects the body. Then, we’ll dive deeper into its causes and types.
Key Takeaways
- Blood cancer is a group of malignancies affecting blood cell production and function.
- It originates in the bone marrow or lymphatic system.
- Blood cells play a vital role in providing energy and fighting infections.
- Understanding blood cancer is essential for patients and their families.
- Blood cancer is a significant health concern worldwide.
Understanding Blood Cancer: A Comprehensive Overview
To understand blood cancer, we need to know its definition, types, and global impact. Blood cancer, also known as hematologic cancer, affects the blood, bone marrow, and lymphatic system. It disrupts the normal production of blood cells, leading to various health complications.
Definition and Medical Terminology
Blood cancer is when abnormal blood cells grow uncontrollably. This stops healthy cells from maturing properly, causing an increase in malignant cells. The main types are leukemia, lymphoma, and myeloma.
Leukemia affects the body’s blood-forming tissues. Lymphoma impacts the lymphatic system, part of the immune system. Myeloma is cancer of plasma cells, a type of white blood cell.
These conditions are classified as hematologic malignancies. Knowing the specific terms is key for diagnosis and treatment. For example, leukemia is divided into acute and chronic forms based on disease progression speed.
Global Impact and Prevalence
Blood cancer is a major global health concern. Studies show that its incidence varies by region. For example, research by Dong et al. (2020) found different leukemia incidence trends in various populations.
Millions of new blood cancer cases are diagnosed every year. The prevalence of different types can be influenced by genetics, environment, and lifestyle. Understanding these factors is vital for prevention and treatment.
The Three Main Types of Blood Cancer
There are three main types of blood cancer: leukemia, lymphoma, and myeloma. Each has its own unique traits and how it affects the body. Knowing these differences helps patients understand their diagnosis and treatment choices.
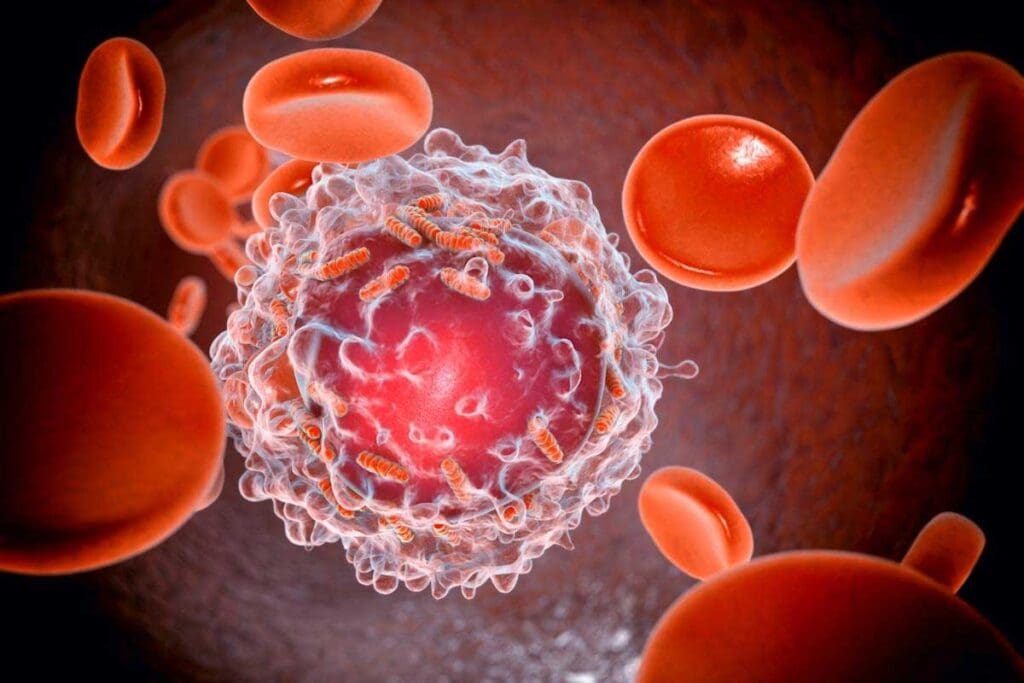
Leukemia: Cancer of the Blood and Bone Marrow
Leukemia affects the white blood cells and can be either acute or chronic. The LivHospital explains that acute leukemia moves fast and needs quick treatment. Chronic leukemia grows slower.
Key characteristics of leukemia include:
- Abnormal white blood cell production
- Impaired immune function
- Potential for anemia and bleeding disorders
Lymphoma: Cancer of the Lymphatic System
Lymphoma targets the lymphatic system, a key part of our immune system. Lewis et al. (2020) note that lymphoma is split into Hodgkin and non-Hodgkin types, with non-Hodgkin being more common.
Common symptoms of lymphoma include:
- Swollen lymph nodes
- Fatigue
- Weight loss
Myeloma: Cancer of Plasma Cells
Myeloma, or multiple myeloma, affects plasma cells in the bone marrow. Cowan et al. (2022) discuss how myeloma impacts bones and the immune system.
Notable features of myeloma:
| Feature | Description |
| Bone lesions | Myeloma cells can cause damage to bones, leading to pain and fractures. |
| Anemia | Reduced red blood cell production can result in anemia. |
| Infections | Impaired immune function increases the risk of infections. |
Leukemia, lymphoma, and myeloma are major cancer types worldwide. Knowing about them is key to creating effective treatments and better patient care.
How Blood Cancer Develops in the Body
Blood cancer starts when blood cells don’t mature right. This leads to cancerous cells. To get how blood cancer starts, we must first know how blood cells are made.
Normal Blood Cell Production Process
Blood cells are made in the bone marrow through hematopoiesis. This process turns stem cells into red, white blood cells, and platelets. Healthy blood cell production is key for oxygen delivery, fighting infections, and stopping bleeding. The bone marrow makes billions of blood cells every day.
The process is controlled by growth factors and genes. Blood cells mature and die in a set order. New cells replace old or damaged ones. This balance keeps blood cell counts healthy.
Disruption of Healthy Cell Maturation
In blood cancer, blood cell production goes wrong. This happens because of genetic mutations or other factors. The cancerous cells grow too much, taking over the bone marrow. This makes it hard for the body to make normal blood cells, causing health problems.
The Cleveland Clinic says DNA mistakes in blood cells can cause cancer. The LivHospital notes that leukemia happens when blood cells mutate, harming the bone marrow’s function. This is a key part of how blood cancer starts.
This disruption can cause different blood cancers like leukemia, lymphoma, and myeloma. Each affects the body in its own way. Knowing this helps us understand how blood cancer grows.
How Do You Get Blood Cancer? Primary Causes
To understand blood cancer, we must look at its main causes. Blood cancer, or hematologic cancer, happens when blood cells’ genes mutate. These changes can come from genes passed down or from new mutations.
Acquired DNA Mutations in Blood Cells
Acquired DNA mutations are changes in blood cells’ DNA over time. They can be caused by chemicals, radiation, or DNA copying errors. Forte et al. (2021) found these mutations are key in blood cancer development.
Key factors leading to these mutations include:
- Exposure to benzene and other industrial chemicals
- Radiation exposure, including from certain medical treatments
- Viruses that can affect blood cells, such as the Human T-Cell Leukemia Virus (HTLV)
Inherited Genetic Predispositions
Inherited genetic predispositions also contribute to blood cancer. Some genetic disorders raise the risk of blood cancer. For instance, people with Down syndrome are more likely to get leukemia.
The table below lists some genetic predispositions and their risks:
| Genetic Disorder | Associated Blood Cancer Risk |
| Down syndrome | Increased risk of leukemia |
| Li-Fraumeni syndrome | Increased risk of various cancers, including blood cancers |
| Ataxia-telangiectasia | Increased risk of leukemia and lymphoma |
Knowing these causes helps in finding ways to prevent and detect blood cancer early. By understanding the risks from both genetic factors, we can take steps to lower our risk of getting blood cancer.
Environmental Risk Factors for Blood Cancer
Certain environmental exposures can increase the risk of blood cancer. It’s important to know how our surroundings affect our health.
Chemical Exposure and Industrial Toxins
Being exposed to certain chemicals and toxins is a big risk for blood cancer. Benzene, found in gasoline and used in many industries, raises the risk of leukemia. Pesticides and some solvents also increase the risk of blood cancers.
- Benzene exposure: Happens mainly in industries that work with benzene, like the petrochemical industry.
- Pesticide exposure: Farmers and those in agriculture are at higher risk because they often use pesticides.
- Solvent exposure: People in industries that use solvents, like dry cleaners, are at a higher risk.
Radiation Exposure Risks
Being exposed to ionizing radiation is another risk for blood cancer. This kind of radiation can damage DNA in cells, leading to cancer.
Sources of ionizing radiation include:
- X-rays and CT scans: Medical imaging that uses ionizing radiation.
- Nuclear accidents: Exposure to radioactive materials from nuclear accidents.
- Cosmic radiation: Pilots and astronauts face higher risks due to cosmic radiation.
Benzene and Other Known Carcinogens
Benzene is a known carcinogen that raises the risk of leukemia, mainly Acute Myeloid Leukemia (AML). Other carcinogens that may increase blood cancer risk include:
- 1,3-Butadiene: Used in making synthetic rubber.
- Formaldehyde: Used in making resins and as a preservative.
Knowing these environmental risks is key to prevention and early detection. By reducing exposure to these risks, we can lower blood cancer rates.
Medical History Factors That Increase Blood Cancer Risk
Our medical history can tell us a lot about our risk for blood cancer. Some past health issues can greatly affect our chances of getting this disease.
Previous Cancer Treatments and Therapies
Some cancer treatments, like chemotherapy and radiation, can raise the risk of blood cancer. The LivHospital says people who had these treatments for other cancers are at higher risk.
Chemotherapy and radiation therapy can harm cell DNA, leading to cancer-causing mutations. These treatments are key in fighting cancer, but knowing their long-term risks is important for patient care.
Pre-existing Blood Disorders
Having blood disorders before can also up the risk of blood cancer. For example, myelodysplastic syndromes, as studied by Sekeres et al. (2022), can lead to leukemia. These conditions affect blood cell production and can turn into more serious blood cancers.
It’s key to watch and manage these conditions to lower blood cancer risk. Regular health checks and screenings help catch problems early.
Immune System Disorders and Blood Cancer
Immune system problems can make it harder for the body to fight cancer. People with weakened immune systems, due to illness or treatments, may face a higher risk of blood cancer.
It’s important to understand how immune system issues and blood cancer risk are connected. Research into this area is ongoing, and its findings are key to better patient care.
Recognizing the Warning Signs of Blood Cancer
Spotting blood cancer early is key, but it’s tough because its symptoms are not always clear. Blood cancer includes leukemia, lymphoma, and myeloma. These diseases share symptoms with many other illnesses, making diagnosis tricky.
Common Symptoms Across Blood Cancer Types
Even though leukemia, lymphoma, and myeloma are different, they share some common signs. These include:
- Fatigue: Feeling very tired that doesn’t get better with rest.
- Frequent Infections: Being more likely to get sick because your immune system is weak.
- Abnormal Bleeding: Bleeding easily, like nosebleeds or bleeding gums.
- Weight Loss: Losing weight without trying, a sign in many cancers.
- Swollen Lymph Nodes: Lymph nodes that are bigger than usual, found in the neck, armpits, or groin.
The Cleveland Clinic and LivHospital say these signs might mean you have blood cancer. Leukemia, for example, can also cause fever, night sweats, and bone pain, along with the usual symptoms.
When to Seek Medical Attention
If you keep feeling sick or have severe symptoms, you should see a doctor. These signs can mean many things, not just blood cancer. But, a doctor’s check-up is vital to find out what’s wrong.
When to be concerned:
- If you’re always tired and it stops you from doing things you need to do.
- If you keep getting sick or if your sickness is really bad.
- If you notice a lot of bruising or bleeding without any reason.
- If you lose a lot of weight without trying to.
Getting diagnosed early can really help with treatment. If you’re worried about your symptoms, talk to your doctor.
Diagnosis and Classification of Blood Cancers
Diagnosing blood cancer involves several tests and exams. It’s key to find the right treatment plan. Knowing the type of blood cancer is essential.
Blood Tests and Bone Marrow Biopsies
Blood tests are often the first step. They show if there are abnormal blood cells or cancer signs. A bone marrow biopsy is also important. It takes a bone marrow sample for checking.
These tests find cancer cells and figure out the blood cancer type. For example, leukemia is found by looking for odd white blood cells in the blood or bone marrow.
Imaging Studies and Other Diagnostic Procedures
Imaging studies like CT scans, MRI scans, or PET scans are used too. They show how far the cancer has spread and if it’s in lymph nodes or organs.
Other tests, like lumbar punctures or flow cytometry tests, help understand the cancer. This helps plan the best treatment.
Staging and Classification Systems
After diagnosing blood cancer, staging shows how far it has spread. Different cancers have their own staging systems. For example, lymphoma uses the Ann Arbor Staging System, while leukemia’s staging depends on blood and bone marrow cell counts.
Knowing the stage and type of blood cancer is vital. It helps choose the right treatment and predict how well it will work.
Treatment Approaches for Different Blood Cancers
The treatment for blood cancer has grown, with many options for each patient. We now have treatments that can fight different blood cancers alone or together.
Chemotherapy and Radiation Therapy
Chemotherapy is a key treatment for many blood cancers. It uses drugs to kill cancer cells. We often mix chemotherapy with other treatments for the best results.
Radiation therapy uses high-energy rays to destroy cancer cells. It’s often used for lymphoma and sometimes leukemia.
Some key points about chemotherapy and radiation therapy include:
- Targeted cell destruction: Both treatments aim to kill cancer cells while protecting healthy cells.
- Combination therapy: Chemotherapy is often paired with other treatments like radiation therapy or targeted therapies.
- Side effect management: We work to reduce side effects such as nausea, fatigue, and hair loss.
Stem Cell Transplantation
Stem cell transplantation is a treatment that can cure some blood cancers. It replaces damaged stem cells with healthy ones. This allows the bone marrow to make normal blood cells. There are two types: autologous (using the patient’s own stem cells) and allogeneic (using donor stem cells).
The benefits of stem cell transplantation include:
- Potential for cure: It can offer a chance of long-term remission or cure for some patients.
- Immune system reset: Allogeneic transplantation can reset the patient’s immune system.
- High-dose chemotherapy: It allows for the use of high-dose chemotherapy, which can be more effective against cancer cells.
Targeted Therapies and Immunotherapies
Targeted therapies and immunotherapies are new ways to treat blood cancer. They target specific cancer cell characteristics or boost the immune system against cancer. Examples include monoclonal antibodies, CAR T-cell therapy, and other innovative treatments.
Some advantages of targeted therapies and immunotherapies are:
- Precision medicine: These treatments target cancer cells more precisely, reducing harm to healthy cells.
- Improved outcomes: Many patients have seen significant improvements with these newer therapies.
- Ongoing research: The field is rapidly evolving, with new treatments being developed all the time.
We keep improving our understanding and treatment of blood cancer. By using these different approaches, we can offer tailored care to each patient.
Reducing Your Risk: Prevention Strategies
Living a healthy lifestyle and knowing about environmental dangers can lower your chance of getting blood cancer. While we can’t stop all cases, we can reduce risks and make healthy choices.
Lifestyle Modifications
Changing your lifestyle can help lower your risk of blood cancer. The Leukemia & Lymphoma Society says some key changes include:
- Not smoking: Smoking increases the risk of many cancers, including blood cancers.
- Maintaining a healthy weight: Being overweight or obese raises the risk of cancer.
- Eating a balanced diet: Eating lots of fruits, veggies, and whole grains is good for your health.
The LivHospital says avoiding smoking and chemicals is very important. “A healthy lifestyle is key to preventing cancer,” they say. This includes eating right and staying active.
Environmental Exposure Reduction
It’s also important to avoid environmental toxins to prevent blood cancer. This means:
- Avoiding chemical exposure: Stay away from industrial toxins and chemicals that can cause cancer.
- Minimizing radiation exposure: Be careful with radiation from medical tests and other sources.
By understanding and reducing these risks, we can take steps to lower our chance of getting blood cancer. Health experts stress the importance of being aware and taking preventive actions.
“Prevention is always better than cure, and in the case of blood cancer, making informed choices can significantly impact your risk profile.”
Conclusion: Understanding Blood Cancer in Modern Medicine
It’s key to understand blood cancer early for better treatment. Thanks to medical research, treatments have gotten much better. Now, doctors can tailor care to each patient’s needs.
Places like Cleveland Clinic and LivHospital show how far we’ve come in treating blood cancers. Leukemia, lymphoma, and myeloma are now more manageable. This gives hope to patients and their families. Supporting research and awareness can help us do even better.
Our knowledge of blood cancer has grown a lot. We’re working hard to improve how we manage and treat it. With ongoing research and better medical care, the outlook for those with this disease is hopeful.
FAQ
What is blood cancer?
Blood cancer, also known as hematologic cancer, affects the blood, bone marrow, or lymphatic system. It happens when blood cells grow abnormally. This can cause various health issues.
What are the main types of blood cancer?
The main types are leukemia, lymphoma, and myeloma. Leukemia affects the blood and bone marrow. Lymphoma targets the lymphatic system. Myeloma is a cancer of plasma cells.
What causes blood cancer?
Causes include genetic and environmental factors. These include DNA mutations, inherited traits, chemical exposure, and certain conditions.
What are the symptoms of blood cancer?
Symptoms include fatigue, weight loss, fever, and night sweats. You might also have recurring infections. Other signs are swollen lymph nodes, bone pain, and anemia.
How is blood cancer diagnosed?
Tests like blood tests and bone marrow biopsies are used. Imaging studies and other procedures help determine the disease’s type and stage.
What are the treatment options for blood cancer?
Treatments vary based on the disease’s type and stage. Options include chemotherapy, radiation, stem cell transplants, targeted therapies, and immunotherapies.
Can blood cancer be prevented?
Preventing blood cancer is challenging, but steps can reduce risk. Avoid harmful chemicals and radiation. Live a healthy lifestyle and get regular check-ups.
How serious is blood cancer?
Blood cancer is serious and can be life-threatening. But, with modern treatments, many manage their disease and achieve remission.
What is the difference between leukemia and lymphoma?
Leukemia affects the blood and bone marrow. Lymphoma targets the lymphatic system. Both have similar symptoms but need different treatments.
Can previous cancer treatments increase the risk of blood cancer?
Yes, treatments like chemotherapy and radiation can raise the risk. They can damage blood cell DNA, leading to cancer.
Reference
- Nematollahi, P. (2023). Environmental risk factors for pediatric acute leukemia. National Institutes of Health – PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10580182/