Last Updated on November 17, 2025 by Ugurkan Demir
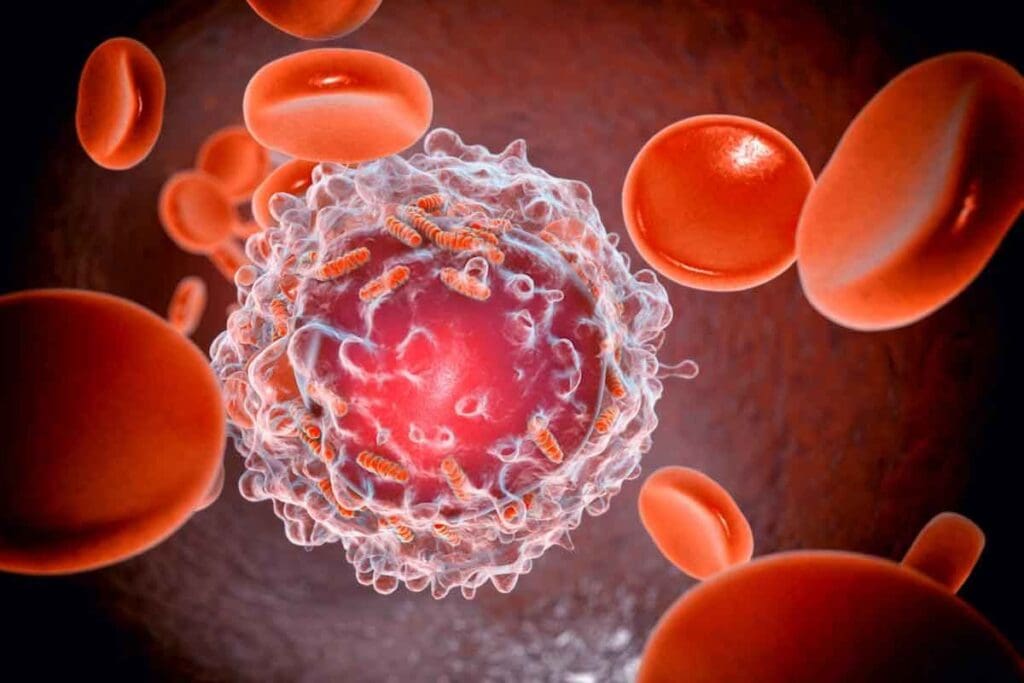
Blood cancer, also known as hematologic cancer, is a group of malignant diseases affecting the blood, bone marrow, or lymphatic system. Cleveland Clinic says it’s a threat to a vital part of you: your blood cells. These cells are key for energy, fighting off infections, and preventing excessive bleeding.
Knowing what is blood cancer is key to understanding its effects. It messes with the body’s blood cell production, causing health problems. We’ll explore how does blood cancer causes these issues, look into the various blood cell cancer types, and explain how they affect the body’s functions.
Learning about blood cancer means exploring its medical terms and definitions. It affects the body’s blood-making parts, like the bone marrow and lymphatic system.
In medical speak, blood cancer is when blood cells grow abnormally. This can cause health problems. The LivHospital says leukemia is cancer in the blood-making tissues, like the bone marrow and lymphatic system.
There are mainly three types of blood cancer: leukemia, lymphoma, and myeloma. Leukemia is cancer in the blood and bone marrow. Lymphoma hits the lymphatic system. Myeloma is cancer of plasma cells.
Blood cancer messes with how blood cells are made. This can lead to many problems. The bad cells take over the bone marrow, making it hard to make healthy blood cells.
| Type of Blood Cell | Normal Function | Impact of Blood Cancer |
| Red Blood Cells | Carry oxygen throughout the body | Reduced oxygen delivery due to anemia |
| White Blood Cells | Play a key role in immune response | Impaired immune function, increasing infection risk |
| Platelets | Essential for blood clotting | Increased risk of bleeding and bruising |
Knowing the medical terms and how blood cancer affects the body is key. It helps doctors and patients understand the condition better. This makes it easier to find the right treatment.

There are three main types of blood cancer: leukemia, lymphoma, and myeloma. Each affects different parts of the blood and lymphatic system. Knowing about these types is key for proper diagnosis and treatment.
Leukemia starts in the bone marrow and affects the blood. It’s caused by too many abnormal white blood cells. This stops normal blood cells from being made.
Leukemia has several types, like acute lymphoblastic leukemia (ALL) and chronic myeloid leukemia (CML).
Lymphoma is a cancer of the immune system’s lymphatic system. It happens when lymphocytes grow out of control. This leads to many types of lymphoma, including Hodgkin and non-Hodgkin lymphoma.
Myeloma, or multiple myeloma, is a cancer of plasma cells in the bone marrow. Cancerous plasma cells take over the marrow, harming normal cells. This can cause bone damage, anemia, and infections.
The table below shows the main features of these blood cancers:
| Type of Blood Cancer | Primary Location | Cells Affected |
| Leukemia | Blood and Bone Marrow | White Blood Cells |
| Lymphoma | Lymphatic System | Lymphocytes |
| Myeloma | Bone Marrow | Plasma Cells |
Blood cancer disrupts the body by messing with blood cell production. The Cleveland Clinic says faulty DNA leads to cancerous blood cells. This can harm many body systems.
Blood cancer messes with the bone marrow’s job to make blood cells. The bone marrow turns stem cells into red, white blood cells, and platelets. But cancer cells take over, reducing healthy cell production.
Blood cancer also hurts the body’s ability to fight off infections and carry oxygen. White blood cells, key for fighting infections, are affected. This makes us more likely to get sick.
Red blood cells, which carry oxygen, can also be impacted. This leads to fatigue and shortness of breath. Platelets, needed for blood clotting, decrease, raising the risk of bleeding.
In short, blood cancer damages the body by messing with blood cell production. This affects the immune system and oxygen transport. Knowing this helps us understand how blood cancer impacts the body.
Genetic mutations play a big role in blood cancer. These changes can be passed down or happen over time. They affect how blood cells are made and work, leading to cancer.
Some inherited conditions raise the risk of blood cancer. For example, Down syndrome and ataxia-telangiectasia are linked to leukemia. These disorders mess with DNA repair and cell growth.
Families with blood cancer history may have genetic risks. While these don’t mean cancer is sure to come, they do up the risk. Knowing about these links helps in early detection and prevention.
Acquired mutations happen over a person’s life. They can come from radiation, chemicals, or DNA copying mistakes. These changes can cause blood cancer by messing with cell functions.
Being around benzene, a chemical in some jobs, raises leukemia risk. Also, past chemo or radiation can cause mutations leading to blood cancers.
Studies are working to understand how genes and environment mix to cause blood cancer. Knowing this helps find at-risk people and find better ways to stop or treat the disease.
Being around certain things can raise your chance of getting blood cancer. Our surroundings are key in figuring out our risk.
“The connection between environmental exposures and blood cancer is a big area of study,” says a top expert in blood cancer. “Knowing these risks helps us prevent the disease.”
Benzene is a big risk for blood cancer. benzene can lead to some types of leukemia. It’s used in many factories, putting workers at risk.
Other chemicals linked to blood cancer include:
It’s important to cut down on these toxins to lower blood cancer risk. Wear protective gear, follow safety rules, and support clean air and water policies.
Radiation is another big risk for blood cancer. Ionizing radiation, like X-rays, can raise the risk of blood cancers, including leukemia.
Sources of radiation exposure include:
While some radiation is unavoidable, knowing the risks helps. Taking steps to reduce exposure can lower blood cancer risk.
In summary, environmental factors are a big deal in blood cancer. By understanding these risks and taking steps to avoid them, we can fight this disease.
Certain medical history factors can increase an individual’s risk of developing blood cancer. We will explore how previous medical conditions and treatments contribute to this risk.
Previous cancer treatments are a significant risk factor for developing certain types of blood cancer. According to the LivHospital, individuals who have undergone specific types of chemotherapy and radiation therapy for other cancers are at a higher risk of developing certain types of leukemia.
Previous cancer treatments, including chemotherapy and radiation therapy, can damage the DNA in cells. This damage can lead to mutations that may cause blood cancer. The risk is higher for individuals who have received:
These treatments can increase the risk of developing therapy-related myelodysplastic syndrome (t-MDS) or therapy-related acute myeloid leukemia (t-AML).
Pre-existing blood disorders can also increase the risk of developing blood cancer. Certain conditions, such as myeloproliferative neoplasms (MPNs), can evolve into more aggressive forms of blood cancer, including acute myeloid leukemia (AML).
Other pre-existing blood disorders that may increase the risk of blood cancer include:
Individuals with these conditions require regular monitoring and follow-up care. This is to detect any progression to blood cancer.
The bone marrow is key to making blood cells. It’s found in bones like the hips and thighbones. It’s where blood cells are made.
Bone marrow is vital for our health. It makes red blood cells for oxygen, white blood cells for fighting infections, and platelets for clotting. It has stem cells that turn into these blood cells. In a healthy person, it makes blood cells well.
Blood cancer messes with the bone marrow’s job. Cancer cells fill the marrow, stopping normal blood cell making. This can cause anemia, infections, and bleeding.
Cancer disrupts the bone marrow in different ways. Leukemia makes bad white blood cells. Lymphoma affects the lymphatic system, linked to the marrow. Myeloma fills the marrow with cancer cells.
Knowing how cancer messes with the bone marrow is key. Doctors can then find better treatments. This helps get blood cell making back to normal and improves health.
Spotting the signs of blood cancer early can make a big difference. Blood cancer includes leukemia, lymphoma, and myeloma. It shows different symptoms that might seem like other, less serious issues. Knowing these signs is key to catching it early and treating it well.
Spotting blood cancer early means paying attention to small signs. Look out for persistent fatigue, unexplained weight loss, and frequent infections. These happen because blood cancer messes with how blood cells are made. This can cause anemia, weaken the immune system, and more.
The LivHospital says fever or chills and persistent fatigue are common in leukemia. If you have these symptoms for a long time, see a doctor.
Each type of blood cancer has its own set of symptoms. For example, leukemia can cause anemia and more infections because of bone marrow failure. Lymphoma might make your lymph nodes swell, give you fever, and cause night sweats. Myeloma can lead to bone pain, anemia, and more infections because of bad cells in the bone marrow.
It’s important to know these differences to get the right treatment. Doctors use tests and exams to figure out what kind of blood cancer you have and how far it has spread.
To find out if someone has blood cancer, doctors use blood tests, bone marrow biopsies, and other tests. They start with blood work and tests. Then, they might do more detailed tests if needed.
The first step is often blood tests to look for odd blood cell levels or cancer signs. The LivHospital says leukemia is often found during these tests. These tests can spot cancer signs in the blood.
Blood tests usually include a complete blood count (CBC). This counts different blood cells. If the results are off, more tests might be needed.
If blood tests hint at blood cancer, advanced tests are done to confirm it. They also figure out the cancer type.
These tests help doctors make a precise diagnosis. This is vital for choosing the right treatment.
Blood cancer treatment varies greatly. It includes many therapies to fight different diseases. The Cleveland Clinic says there are many safe and effective ways to treat blood cancer. We’ll look at treatments for leukemia, lymphoma, and myeloma.
Chemotherapy is key in treating blood cancers. It uses drugs to kill cancer cells. It’s often paired with other treatments.
Radiation therapy uses rays to destroy cancer cells. Both treatments can cause side effects. Yet, they are vital in managing blood cancer.
Choosing between chemotherapy and radiation depends on the cancer type and stage. Chemotherapy is often used for leukemia and lymphoma. Radiation therapy might be used for lymphoma or to prepare for a stem cell transplant.
Stem cell transplantation replaces diseased stem cells with healthy ones. It’s important for some blood cancers like leukemia and lymphoma. There are two types: autologous (using the patient’s own cells) and allogeneic (using donor cells).
Deciding on stem cell transplantation depends on health, cancer type, and donor availability.
Targeted therapies and immunotherapies are new, precise treatments. Targeted therapies attack specific cancer cells. Immunotherapies use the immune system to fight cancer.
Targeted therapies include drugs for specific genetic mutations. Immunotherapies include CAR-T cell therapy. It’s promising for blood cancers like ALL and DLBCL.
These treatments are changing blood cancer therapy. They offer hope to patients and their families.
Prevention is key. There are many lifestyle changes and monitoring strategies to lower blood cancer risk. While some risks can’t be changed, managing what we can is very important.
The LivHospital says avoiding certain chemicals, like benzene, can lower leukemia risk. This shows how important it is to be careful about our environment and avoid harmful substances.
Healthy lifestyle choices can help lower blood cancer risk. Some of these choices include:
People at higher risk, like those with a family history or past exposure, need regular checks. This may include:
By following these lifestyle tips and monitoring, people can lower their blood cancer risk.
Research has greatly improved blood cancer treatments and outcomes. The Cleveland Clinic notes that more people can now live with blood cancer thanks to new treatments. These include targeted therapies like stem cell transplantation and immunotherapies.
Blood cancers like leukemia, lymphoma, and myeloma need quick and accurate diagnosis. It’s important for patients and doctors to understand how serious blood cancer is. Early detection and awareness are critical in managing the disease.
Research keeps uncovering the mysteries of blood cancer, leading to new treatments. By keeping up with the latest research, patients can make better choices about their care. This improves their quality of life.
Blood cancer, also known as hematologic cancer, is a disease that affects blood cells. It makes it hard for the body to make healthy blood cells. This leads to various health issues.
There are three main types of blood cancer. Leukemia affects the blood and bone marrow. Lymphoma impacts the lymphatic system. Myeloma is a cancer of plasma cells.
Blood cancer is caused by genetics and the environment. It can come from inherited disorders, genetic changes, or exposure to harmful substances. It can also result from previous cancer treatments.
Blood cancer disrupts blood cell production. This causes problems like anemia, infections, and bleeding. It also affects the immune system and oxygen transport.
Symptoms vary by cancer type. Common signs include fatigue, weight loss, fever, and swollen lymph nodes. If symptoms last, seek medical help.
Tests diagnose blood cancer. These include blood work, bone marrow biopsies, and imaging studies. Accurate diagnosis is key for effective treatment.
Treatments include chemotherapy, radiation, stem cell transplants, and more. The right treatment depends on the cancer type, stage, and patient factors.
Preventing blood cancer is not guaranteed. But, a healthy diet and avoiding toxins may help. High-risk individuals should be monitored closely.
Blood cancer is a serious condition. It needs immediate medical attention. The outcome depends on the cancer type, stage, and patient factors.
Bone marrow produces blood cells. In blood cancer, it makes abnormal cells. This disrupts blood cell production.
Yes, genetic disorders and mutations can lead to blood cancer.
Radiation can damage blood cell DNA. This leads to genetic mutations and increases blood cancer risk.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!