Last Updated on December 2, 2025 by Bilal Hasdemir
About 15% of people in the U.S. have a hiatal hernia. This condition can make surgery necessary. Surgery can significantly enhance quality of life. How Is Hiatal Hernia Surgery Done: Procedure Overview
A hiatal hernia happens when stomach parts move up into the chest. This is through a hole in the diaphragm. Hiatal hernia repair surgery helps fix this issue. It alleviates symptoms such as severe heartburn and difficulty swallowing.
Key Takeaways
- Hiatal hernia surgery is a big step to ease severe symptoms.
- The surgery repairs the hernia and prevents further complications.
- Understanding the surgical procedure prepares patients for what to expect.
- Hiatal hernia repair surgery can really boost a patient’s life quality.
- It’s a common fix for those with bad hiatal hernia symptoms.
Understanding Hiatal Hernias
A hiatal hernia happens when part of the stomach moves up into the chest. This is through an opening in the diaphragm. It can cause symptoms and complications. Knowing about it, its types, and when surgery is needed is key.
Definition and Types of Hiatal Hernias
Hiatal hernias are mainly two types: sliding and paraesophageal. Sliding hernias are common. They happen when the stomach and esophagus slide up into the chest. Paraesophageal hernias occur when stomach bulges up beside the esophagus. This can lead to serious problems.
Common Symptoms and Complications
Symptoms of hiatal hernias include heartburn, chest pain, and trouble swallowing. If not treated, serious issues like gastric volvulus or strangulation can happen. These are emergencies.
- Heartburn and regurgitation
- Chest pain or discomfort
- Difficulty swallowing
- Shortness of breath
When Surgery Becomes Necessary
Surgery is often needed for severe symptoms or complications. It’s also considered if other treatments fail. The choice to have surgery depends on the hernia’s severity, the patient’s health, and any complications.
Deciding on surgery for hiatal hernias involves weighing benefits against risks. Benefits include symptom relief and preventing future issues. Risks include those of surgery itself.
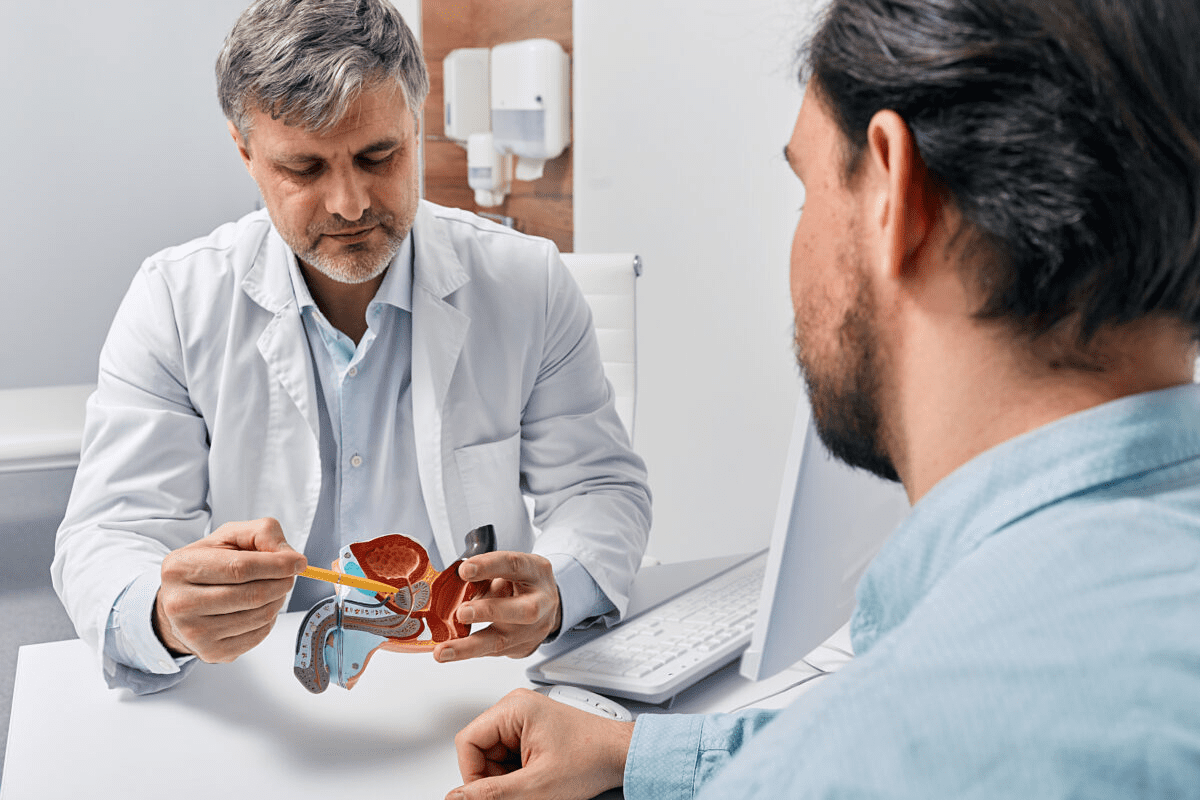
Pre-Surgical Evaluation Process
The pre-surgical evaluation is a key step before hiatal hernia repair surgery. It checks if patients are good candidates for the surgery. It also looks for any risks or complications.
Diagnostic Tests and Imaging
Diagnostic tests are very important in this process. They help doctors see how big the hernia is and how it affects the body.
- Endoscopy: Allows direct visualization of the esophagus, stomach, and hernia.
- Barium Swallow: Provides detailed images of the upper digestive tract.
- Manometry: Assesses esophageal function and motility.
- 24-hour pH Monitoring: Measures acid exposure in the esophagus.
Medical History Assessment
Looking at a patient’s medical history is very important. It helps find any conditions that might affect the surgery or recovery. This includes:
- Previous surgeries or medical conditions.
- Current medications and possible interactions.
- Allergies or sensitivities.
- Lifestyle factors such as smoking or obesity.
Determining Surgical Candidacy
After the tests and medical history check, the team decides if surgery is right for the patient. They look at:
- The severity of symptoms and how they affect daily life.
- The size and type of hiatal hernia.
- Any complicating factors.
- The patient’s overall health and ability to handle surgery.
By thoroughly evaluating these factors, medical teams can develop a personalized treatment plan for the patient.
Preparing for Hiatal Hernia Surgery
Preparing for hiatal hernia surgery requires making several adjustments. You’ll need to adjust your meds, diet, and lifestyle. Doing this right can make a big difference in how well you do after surgery.
Medication Adjustments
It’s important to talk to your doctor about your meds before surgery. Some meds, like blood thinners, might need to be changed or stopped. This is to lower the risk of bleeding during the operation.
- Tell your doctor about all the meds you’re taking.
- Find out if you need to change or stop any meds that could affect surgery.
- Always follow your doctor’s advice on meds carefully.
Dietary and Lifestyle Changes
Modifying your diet and lifestyle prior to surgery can be very beneficial. It makes the surgery and recovery easier.
- Don’t do heavy lifting or hard activities before surgery, as your doctor says.
- Eat a healthy diet full of nutrients to keep you strong.
- Stick to any special diet your healthcare team tells you to follow.
Nutritional Guidelines
Nutrient | Recommended Foods | Avoid |
Protein | Lean meats, fish, eggs, dairy | High-fat meats |
Fiber | Fruits, vegetables, whole grains | Processed foods |
Pre-operative Instructions
It’s key to follow your doctor’s pre-surgery instructions. They’ll give you specific advice on getting ready for the procedure.
Common pre-operative instructions include:
- Fasting for a certain time before surgery.
- Not taking certain meds or supplements.
- Using special soap to shower or bathe to lower infection risk.
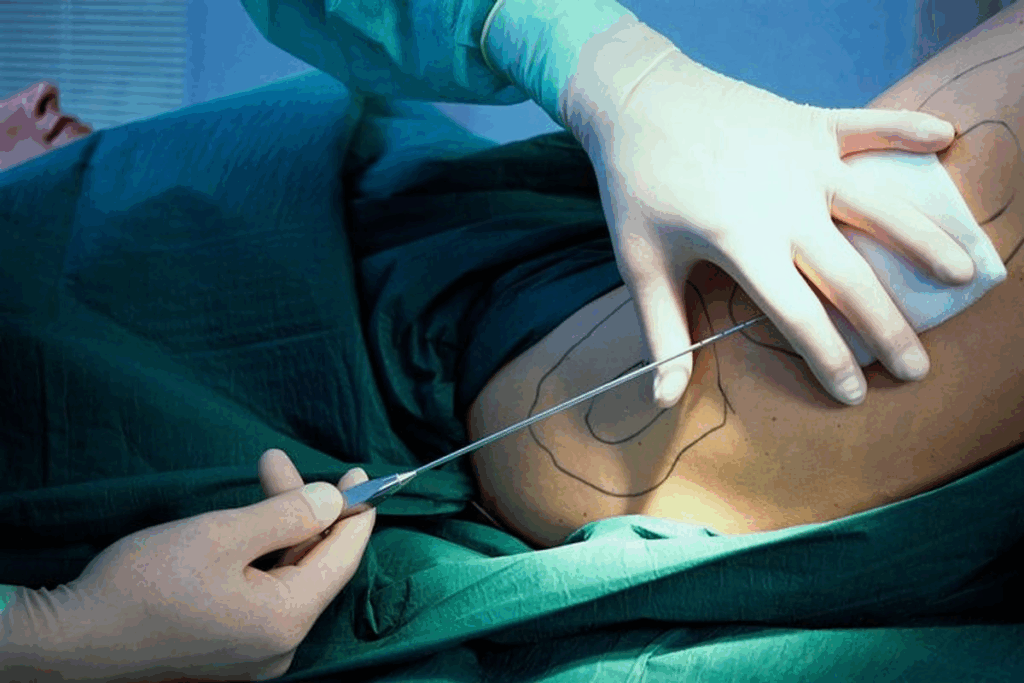
Surgical Approaches for Hiatal Hernia Repair
Treating hiatal hernias through surgery involves different methods. These range from traditional open surgery to modern, minimally invasive techniques. The choice of method depends on the patient’s health, the hernia’s size and type, and the surgeon’s skills.
Open Surgery vs. Minimally Invasive Techniques
For a long time, open surgery was the main way to fix hiatal hernias. This method requires a big cut in the belly or chest to reach the hernia. But, new tech has made minimally invasive techniques more common. These use small cuts and a camera to do the repair.
Minimally invasive surgery has many benefits:
- Less pain after surgery
- Shorter time in the hospital
- Quicker recovery
- Fewer risks of problems
- Better looks after healing
Laparoscopic Approach Benefits
Laparoscopic surgery is a key part of minimally invasive methods. It uses a thin, lighted tube with a camera and tools through small belly cuts. This method has many advantages:
- Better view of the hernia and nearby areas
- Lower risk of surgery problems
- Quicker getting back to normal
- Less scarring
Robotic-Assisted Surgery Options
Robotic-assisted surgery is a cutting-edge, minimally invasive method. It uses a robotic system to help the surgeon. This system gives clear 3D views, precise tools, and better comfort for the surgeon. Its benefits include:
- More precise and skilled work
- Better view and access to areas
- Less tiredness for the surgeon
- Potentially better results in tough cases
Robotic-assisted surgery has many perks. But, it’s not for everyone. It depends on the surgeon’s experience and the patient’s situation.
How is Hiatal Hernia Surgery Done: Step-by-Step Procedure
The process of hiatal hernia surgery is carefully planned to help patients get the best results. It involves many important steps, from getting ready for surgery to recovering afterwards.
Anesthesia Administration
The first thing done in hiatal hernia surgery is giving anesthesia. General anesthesia is used to keep the patient comfortable and pain-free. The anesthesiologist watches the patient’s vital signs and changes the anesthesia as needed.
Surgical Access and Visualization
After the patient is under anesthesia, the surgical team gets to the hernia area. Minimally invasive techniques, like laparoscopy, are often used. This method uses small cuts for a camera and tools, giving a clear view of the area.
Hernia Reduction Process
The next step is to reduce the hernia. The surgeon carefully moves the stomach back to its normal place. This step needs to be done carefully to avoid harming nearby tissues.
Diaphragm Repair Techniques
After fixing the hernia, the surgeon works on the diaphragm. They close the hiatus to stop future hernias. They might use primary closure or mesh reinforcement to help the repair.
Hiatal hernia surgery is complex and requires a lot of care. Familiarizing themselves with these steps helps patients know what to expect.
Fundoplication Techniques in Hiatal Hernia Repair
Fundoplication techniques are key in fixing hiatal hernias. They help strengthen the lower esophageal sphincter. This is done by wrapping the stomach’s upper part around the esophagus’s lower part. This stops acid reflux and helps with symptoms of hiatal hernias.
Nissen Fundoplication (360-Degree Wrap)
Nissen fundoplication, or a 360-degree wrap, is a common method. It wraps the stomach’s fundus around the esophagus. This creates a strong barrier against stomach acid flowing back into the esophagus. The Nissen technique is very good at reducing GERD symptoms and is often done laparoscopically.
This method greatly reduces acid reflux symptoms and has low complication rates with skilled surgeons. But, some might find it hard to swallow or get gas-bloat syndrome.
Toupet Fundoplication (Partial Wrap)
Toupet fundoplication, or a 270-degree wrap, is a partial method. It wraps the stomach’s fundus around the esophagus’s back side. This is less tight than Nissen and might be better for those at risk of swallowing problems.
The Toupet technique is great for those with esophageal motility issues. It offers a partial wrap to lower the risk of swallowing trouble while controlling reflux.
Dor Fundoplication and Other Variations
Dor fundoplication is a partial method, with a 180-degree to 270-degree wrap. It’s often used with other surgeries, like Heller myotomy for achalasia, to stop reflux.
Other methods, like Lind and Belsey Mark IV, have their own uses and benefits. The right technique depends on the patient’s anatomy, the surgeon’s style, and the hernia’s type.
In summary, fundoplication techniques are vital in hiatal hernia repair. They offer various options to meet different patient needs. Knowing the differences between Nissen, Toupet, Dor, and others helps surgeons choose the best approach for their patients.
Mesh Reinforcement in Hiatal Hernia Surgery
In hiatal hernia surgery, mesh reinforcement is key. It uses a synthetic or biological material to support the weakened area. This area is around the esophageal hiatus.
Types of Surgical Mesh Materials
Surgical mesh materials are divided into synthetic and biological types. Synthetic meshes are made from materials like polypropylene or polyester. They are durable and promote tissue growth. Biological meshes come from animal tissues and are absorbed by the body over time. This reduces the risk of long-term problems.
When Mesh Reinforcement is Recommended
Mesh reinforcement is often suggested for large hiatal hernias or those at high risk of recurrence. The decision to use mesh varies based on the patient’s anatomy and the hernia’s complexity.
- Large hiatal hernias that require additional support
- Patients with a history of hernia recurrence
- Cases where the tissue quality is poor
Potential Complications with Mesh
While mesh reinforcement improves surgery outcomes, it comes with risks. These include mesh erosion, dysphagia, and adhesions. Mesh erosion happens when the mesh moves into surrounding tissues or organs. This can lead to severe issues.
In summary, mesh reinforcement is a valuable tool in hiatal hernia surgery. It offers support and may lower recurrence risk. But, it’s important to choose patients and mesh types wisely to avoid complications.
Specialized Techniques for Large Hiatal Hernias
Surgery for big hiatal hernias needs a careful plan. These hernias are big and complex, so they can’t be fixed with just one method.
Collis Gastroplasty
Collis gastroplasty is a special surgery for big hiatal hernias. It’s used when the esophagus is too short. The surgery makes a new esophagus by wrapping the stomach around it. This makes the esophagus longer and helps fix it without tension.
Key benefits of Collis gastroplasty include:
- Enabling a tension-free repair by lengthening the esophagus
- Reducing the risk of recurrence by ensuring adequate esophageal length
- Improving the overall outcome by allowing for a more anatomically correct repair
Tension-Free Repair Methods
Fixing large hiatal hernias without tension is key. Methods that do this have fewer failures and better results for patients.
Tension-Free Repair Technique | Description | Benefits |
Laparoscopic Mesh Repair | Uses mesh to strengthen the hiatal closure, reducing tension on the repair | Low recurrence rate, less postoperative pain |
Robotic-Assisted Repair | Improves precision in dissecting and repairing the hiatus, facilitating a tension-free closure | Improved precision, reduced risk of complications |
Managing Paraesophageal Hernias
Paraesophageal hernias need special care because they can cause serious problems. These include getting stuck and cut off from blood supply.
The key to managing paraesophageal hernias is finding them early and fixing them surgically. Surgery often involves moving the hernia back, removing the sac, and fixing the hiatal area. Sometimes, mesh is used.
Choosing the right surgery depends on many things. These include the size of the hernia, the patient’s health, and the surgeon’s skill. A custom plan helps patients with big and complex hernias get the best care.
Immediate Post-Operative Care
The time right after hiatal hernia surgery is key for a good recovery. Patients are watched closely, and steps are taken to manage pain and prevent problems.
Recovery Room Monitoring
After surgery, patients go to the recovery room. There, doctors and nurses keep a close eye on them. They check heart rate, blood pressure, and oxygen levels to make sure the patient is okay.
Vital Signs Monitoring: This helps find any issues early, so doctors can act fast.
Pain Management Strategies
Managing pain well is very important after surgery. Doctors use different ways to help with pain, including:
- Medications: Giving pain relief drugs as needed.
- Regional Anesthesia: Using epidural anesthesia for pain relief.
- Non-pharmacological Methods: Using deep breathing, relaxation, and positioning to manage pain.
Early Mobilization Protocols
Moving around early is important to prevent problems like blood clots. It also helps with recovery. This means:
- Getting up and walking soon after surgery.
- Doing simple exercises to improve blood flow.
Early movement helps with physical recovery and lowers the chance of complications.
Initial Dietary Guidelines
Changing what you eat is a big part of recovery. At first, patients eat liquids, then soft foods, and later regular food as they can.
Dietary Stage | Foods Allowed | Duration |
Liquid Diet | Clear liquids, broths | 1-2 days |
Soft Diet | Soft foods, pureed foods | 2-5 days |
Normal Diet | Gradual introduction of regular foods | After 5 days |
By sticking to these guidelines, patients can have a smoother recovery and lower the risk of problems after hiatal hernia surgery.
Recovery Timeline After Hiatal Hernia Surgery
Knowing what to expect after hiatal hernia surgery is key. It helps patients manage their recovery better. The time it takes to heal can differ, but there are common steps most follow.
Duration of Hospital Stay
The time in the hospital varies. It depends on the surgery type and the patient’s health. Laparoscopic surgeries usually mean a shorter stay, often 1 to 3 days.
Open surgeries might keep patients in the hospital longer. They could stay up to 5 days or more to ensure they heal well.
Activity Restrictions and Progression
Right after surgery, patients need to avoid heavy tasks. This helps them heal and prevents problems.
- For the first 2-3 weeks, patients should do only light tasks, like short walks.
- By 4-6 weeks, they can start doing more normal things, like driving and light exercise.
- It takes about 6-8 weeks to get back to heavy lifting or strenuous activities.
Returning to Normal Diet and Activities
Changing your diet is important during recovery. At first, you might only eat liquids or soft foods.
Later, you can start eating solid foods again, usually in 4-6 weeks.
Getting back to normal activities takes time too. Most people can get back to their usual life in a few weeks to a couple of months.
Importance of Follow-Up Appointments
Attending follow-up appointments is crucial for patient recovery. They help check how you’re healing and catch any problems early.
These visits let the surgeon see how you’re doing. They might also remove stitches or staples and answer any questions you have.
Going to all your follow-up appointments is key for a good recovery.
Potential Complications and Risks
It’s important to know the risks of hiatal hernia surgery. The procedure is usually safe and works well. But, there are risks that patients should understand.
Common Short-Term Complications
Short-term issues can happen during or right after surgery. These might include:
- Infection at the surgical site
- Bleeding or hematoma
- Reaction to anesthesia
- Respiratory or cardiac issues
Table: Common Short-Term Complications
Complication | Description | Management |
Infection | Bacterial infection at the surgical site | Antibiotics, wound care |
Bleeding | Excessive bleeding during or after surgery | Transfusion, surgical intervention |
Long-Term Surgical Complications
Long-term issues can happen after recovery. These might include:
- Recurrence of the hiatal hernia
- Dysphagia (difficulty swallowing)
- Gas-bloat syndrome
- Adhesions or bowel obstruction
It’s key for patients to watch for these long-term complications. This helps them stay on top of their health.
Warning Signs to Monitor
Be on the lookout for warning signs of complications. These include:
- Severe abdominal pain
- Difficulty swallowing
- Vomiting blood or black tarry stools
- Fever or chills
If you notice any of these symptoms, get medical help right away.
Managing Post-Surgical Dysphagia
Dysphagia is a common issue after surgery. To manage it, try:
- Dietary adjustments (e.g., eating smaller, more frequent meals)
- Avoiding foods that trigger discomfort
- Postural changes during eating
In some cases, you might need more medical help for persistent dysphagia.
Non-Surgical Alternatives and Complementary Approaches
Before surgery, think about non-surgical ways to handle hiatal hernia symptoms. These methods can help manage symptoms and improve life quality.
Medical Management Options
Medical management is key for treating hiatal hernias without surgery. It combines medicines and lifestyle changes to ease symptoms.
- Proton Pump Inhibitors (PPIs): These drugs cut down stomach acid, easing heartburn and acid reflux.
- H2-Receptor Antagonists: These also lower stomach acid, helping some patients.
- Antacids: For quick relief from heartburn and indigestion, antacids work well.
It’s important to talk to a healthcare provider to find the right medicine and dosage for you.
Lifestyle Modifications
Changing your lifestyle can help manage hiatal hernia symptoms. Simple changes can make a big difference.
- Dietary Changes: Stay away from foods that trigger symptoms like citrus fruits, tomatoes, and spicy or fatty foods.
- Weight Management: Keeping a healthy weight can ease stomach pressure and symptoms.
- Elevating the Head of the Bed: Raising the bed head by 6-8 inches can stop stomach acid from flowing into the esophagus at night.
“Lifestyle changes are often the first step against hiatal hernia symptoms. Making smart choices can greatly improve your life quality.”
When to Consider Alternatives vs. Surgery
Choosing between non-surgical options or surgery depends on several things. These include symptom severity, health, and complications.
- Severity of Symptoms: For mild to moderate symptoms, non-surgical methods might be enough.
- Presence of Complications: If there are severe complications like esophagitis or Barrett’s esophagus, surgery might be better.
- Patient Preference: The choice between non-surgical treatment and surgery should be made with a healthcare provider. It should consider the patient’s preferences and health.
By thinking about these factors, you can make a well-informed choice about your treatment.
Long-Term Outcomes and Success Rates
The success of hiatal hernia surgery is seen in its long-term outcomes. These include symptom resolution and quality of life improvements. It’s key for patients to understand these outcomes before choosing this treatment.
Symptom Resolution Statistics
Many studies show that most patients feel much better after surgery. are high, leading to better lives for many.
Study | Symptom Resolution Rate | Follow-up Period |
Smith et al., 2020 | 85% | 2 years |
Johnson et al., 2019 | 90% | 5 years |
Williams et al., 2021 | 88% | 3 years |
Recurrence Rates and Factors
Even though surgery is usually effective, some people may experience a return of symptoms. The rate of recurrence depends on the surgery method, the patient’s body, and post-op care. Most studies show that recurrence rates are under 10% with proper care.
“The use of mesh reinforcement during hiatal hernia repair has been shown to reduce recurrence rates significantly.”
– Expert Opinion
Quality of Life Improvements
People who have surgery often see big improvements in their quality of life. These improvements come from fewer symptoms, better digestion, and less discomfort. Studies show that patients are much happier after surgery.
Recent Research and Advancements
New surgical techniques and technology are making surgery better. Robotic-assisted surgery and laparoscopic approaches are becoming more common. They offer less invasive options with faster recovery times. Ongoing research aims to make these techniques even better.
As the field keeps growing, patients can look forward to even better results from surgery. There’s a focus on personalized care and new surgical methods.
Conclusion
Hiatal hernia surgery is a complex process that needs careful thought and planning. We’ve looked at many parts of hiatal hernia repair, from finding out you have one to taking care of yourself after surgery.
The ways to fix a hiatal hernia have changed, making surgery less invasive and better for patients. Knowing about the different types of hernias, their symptoms, and possible problems helps figure out the best treatment.
In short, hiatal hernia surgery is a good choice for those with hernias. A detailed look at hiatal hernia repair shows how important it is to choose the right patient, use the right surgery method, and take good care after surgery for the best results.
Understanding hiatal hernia surgery helps patients make better choices about their treatment. This can greatly improve their life quality.
FAQ
What is a hiatal hernia, and how is it diagnosed?
A hiatal hernia happens when the stomach bulges into the chest. This occurs through an opening in the diaphragm. Doctors use X-rays, CT scans, or endoscopy to diagnose it.
What are the symptoms of a hiatal hernia, and when does surgery become necessary?
Symptoms include heartburn, chest pain, and trouble swallowing. Surgery is needed for severe symptoms or complications like strangulation.
What are the different surgical approaches for hiatal hernia repair?
There are open surgery, laparoscopic surgery, and robotic-assisted surgery. Laparoscopic surgery is less invasive, leading to less pain and quicker recovery.
What is the step-by-step process of hiatal hernia surgery?
The surgery starts with anesthesia and gaining access. Then, the hernia is reduced and the diaphragm is repaired. The steps can vary based on the method used.
What are fundoplication techniques, and how are they used in hiatal hernia repair?
Fundoplication wraps the stomach around the esophagus to stop reflux. There are Nissen, Toupet, and Dor fundoplications, each with its own benefits.
What is mesh reinforcement, and when is it used in hiatal hernia surgery?
Mesh reinforcement uses a synthetic or biological mesh for support. It’s often used for larger hernias or weak tissue.
How long does it take to recover from hiatal hernia surgery?
Recovery time varies, but most can return to normal in a few weeks. Hospital stays are short, and follow-ups are needed to check healing.
What are the possible complications and risks of hiatal hernia surgery?
Risks include bleeding and infection short-term, and long-term issues like dysphagia and recurrence. It’s important to watch for warning signs and follow instructions.
Are there non-surgical alternatives for managing hiatal hernias?
Yes, options include antacids and lifestyle changes like diet and weight loss. These might be for mild symptoms or those not suited for surgery.
What are the long-term outcomes and success rates of hiatal hernia surgery?
Surgery often resolves symptoms and improves life quality. Success rates vary by technique and individual factors. Research and advancements are continually improving outcomes.
What is the difference between laparoscopic and open hiatal hernia repair surgery?
Laparoscopic surgery uses smaller incisions for less pain and quicker recovery. Open surgery requires a larger incision.
How is the hiatal hernia repair surgery performed using robotic-assisted techniques?
Robotic-assisted surgery enhances the surgeon’s skills with high-definition visualization and precise movements. It’s beneficial for complex cases.
What are the benefits of laparoscopic hiatal hernia repair?
Benefits include less pain, shorter hospital stays, quicker recovery, and lower complication risks.
References
National Institutes of Health. Evidence-Based Medical Insight. Retrieved from https://www.niddk.nih.gov/health-information/digestive-diseases/hiatal-hernia