Last Updated on December 2, 2025 by Bilal Hasdemir

Every year, thousands of kids in the U.S. get pediatric blood transfusions that save their lives. These transfusions are key for kids with health issues like anemia, cancer, and after surgery. Providing the typical duration and factors that influence How long does a blood transfusion take for pediatric patients.
As a parent or caregiver, the idea of your child getting a blood transfusion might worry you. The time it takes can change based on the child’s health and the hospital’s rules.
Key Takeaways
- Pediatric blood transfusions are vital for treating many health problems in kids.
- The time needed for a blood transfusion varies, depending on the type and the child’s health.
- Hospitals have strict rules to make sure blood transfusions are safe and work well.
- Knowing about the transfusion process and what affects its length can ease worries for parents and caregivers.
- Pediatric blood transfusions are a common and lifesaving medical treatment.
Understanding Blood Transfusion Basics

Pediatric blood transfusions need a deep understanding of medical basics. They are key in medical care, mainly for kids in surgery, with anemia, or other blood cell issues.
What is a Blood Transfusion?
A blood transfusion is when blood or its parts are given to a patient. This is lifesaving in many cases, like severe injuries, surgeries, and diseases that harm blood cell making.
We give blood transfusions to help kids get better from many health issues. The blood types must match to avoid problems.
Why are Pediatric Transfusions Necessary?
Pediatric transfusions are needed for many reasons. Kids in major surgeries or with anemia or leukemia need them. Premature babies also need them because their blood cells aren’t fully made yet.
- Replacing red blood cells to improve oxygen delivery to tissues
- Providing platelets to prevent or treat bleeding
- Administering plasma to correct clotting disorders
These transfusions are vital for kids’ recovery and health.
Common Types of Blood Products Used
The main blood products used are red blood cells, plasma, and platelets. Each has a special role:
- Red Blood Cells: Treat anemia and boost oxygen to body tissues.
- Plasma: Fixes clotting issues and gives important proteins.
- Platelets: Stops or treats bleeding from low platelet counts.
Knowing about these products helps understand transfusions better.
Factors Influencing Transfusion Duration

Knowing what affects transfusion duration is key in pediatric care. The time it takes to give a blood transfusion to kids depends on several important things.
Patient’s Age and Weight
A child’s age and weight are big factors in how long a blood transfusion takes. Younger patients and those who weigh less need more careful planning for the transfusion rate. This can make the transfusion take longer. We make sure to consider these factors to keep the transfusion safe and effective.
Type of Blood Product
The type of blood product being given also affects how long the transfusion lasts. Different parts of blood, like red blood cells, platelets, or plasma, need different rates for transfusion. For example, platelets might be given faster than red blood cells.
Pre-Transfusion Testing
Pre-transfusion testing is also very important for the duration of a pediatric blood transfusion. This testing checks if the donor blood is compatible with the recipient’s blood. The time needed for these tests can vary, sometimes causing a delay in starting the transfusion. We stress the need for thorough pre-transfusion testing to reduce risks and ensure a good transfusion outcome.
Understanding these factors helps healthcare providers predict how long a pediatric blood transfusion will take. This knowledge also helps families and caregivers know what to expect during the transfusion. It makes the process clearer for everyone involved.
Typical Duration of Pediatric Blood Transfusions
Knowing how long a pediatric blood transfusion lasts is important for parents and caregivers. The time it takes can change based on several things. These include the type of blood product and the child’s specific needs.
Average Time for Different Blood Types
The time for different blood products can vary. For example, a transfusion of red blood cells, used for anemia or blood loss, usually takes 2-4 hours.
Platelet transfusions, used to prevent or treat bleeding, are often quicker. They can be given in 1-2 hours.
Comparison with Adult Transfusions
Pediatric transfusions are different from adult ones. Children’s smaller size and varying blood volumes make the process more complex.
The dose and rate of transfusion are carefully planned. They are based on the child’s weight and medical needs. This affects how long the procedure lasts.
Steps Involved in a Blood Transfusion
For kids, blood transfusions are done with great care at every step. We make sure the transfusion is safe and works well.
Pre-Transfusion Preparation
Before starting a blood transfusion, we do a lot of important things. It’s key to make sure the blood matches the patient’s. Here’s what we do:
- We check the patient’s identity and medical history.
- We run blood tests to find out the patient’s blood type and any antibodies.
- We pick the right blood product for the patient’s needs.
- We check the blood product for damage or contamination.
We also make sure all equipment is ready. We want the patient to be comfortable and know what’s happening.
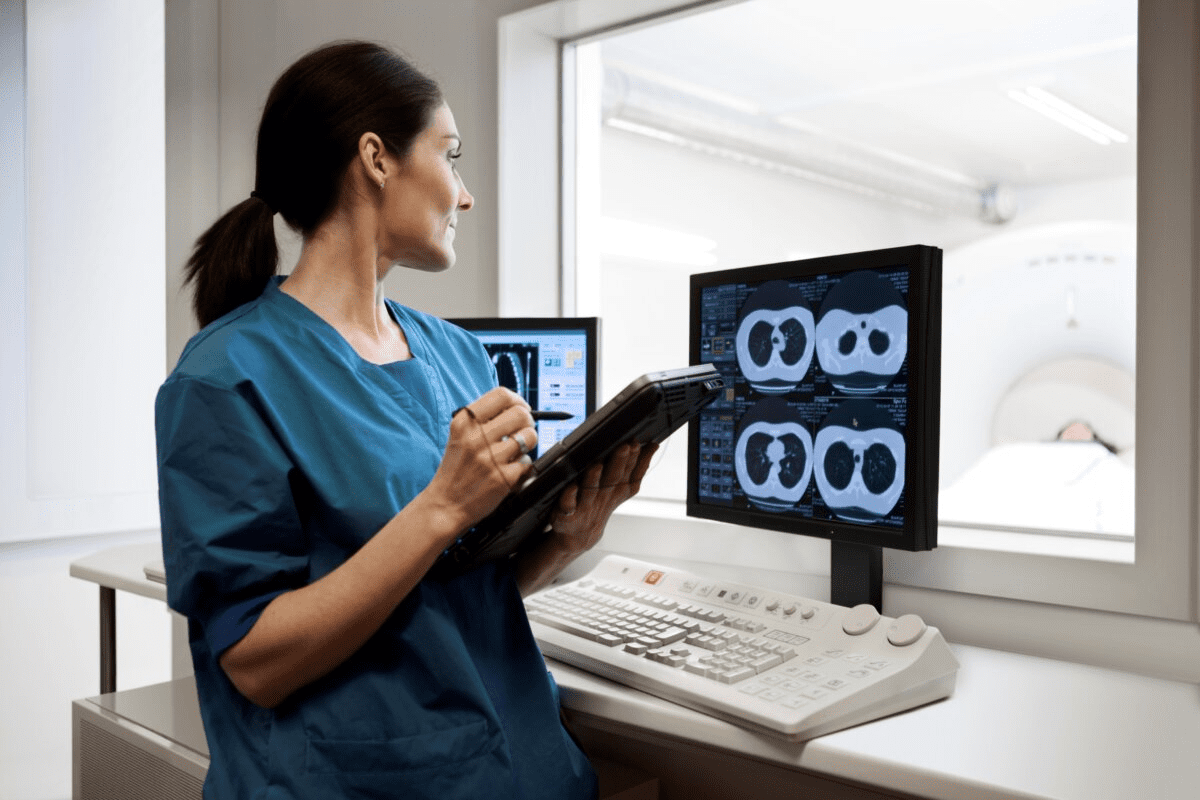
Monitoring During Transfusion
While the transfusion is happening, we watch the patient closely. We check their temperature, heart rate, and blood pressure often. We also control how fast the blood is given to avoid problems.
Here are some things we keep an eye on:
- The patient’s overall health and any symptoms.
- The amount of blood given and how fast it’s given.
- Any signs of a reaction, like fever or rash.
By sticking to a strict transfusion protocol, we lower risks. This helps our pediatric patients get the best care.
Risks and Considerations in Pediatric Transfusions
Pediatric blood transfusions are lifesaving but carry risks. Parents and healthcare providers need to know about these risks. It’s important to understand how to reduce them for the best results.
Common Reactions to Transfusions
Blood transfusions are generally safe but can cause reactions. Allergic reactions like urticaria (hives) and pruritus (itching) can be treated with medicine. Rare but serious reactions include hemolytic transfusion reactions, which can be very dangerous.
Other reactions include febrile non-hemolytic transfusion reactions (FNHTR) and transfusion-related acute lung injury (TRALI). Knowing about these reactions helps us act fast if they happen.
Mitigating Possible Risks
We use several ways to lower the risks of pediatric blood transfusions. Pre-transfusion testing checks for blood type and screens for infections. Leukoreduction removes white blood cells to lessen the chance of some reactions.
| Risk Mitigation Strategy | Description | Benefit |
| Pre-transfusion testing | Thorough checks for blood type compatibility and screening for infectious agents | Reduces risk of hemolytic reactions and transmission of infectious diseases |
| Leukoreduction | Removing white blood cells from donated blood | Decreases risk of FNHTR and HLA alloimmunization |
| Careful monitoring during transfusion | Continuous observation for signs of adverse reactions | Enables prompt intervention in case of a reaction |
By knowing the risks and using these strategies, we can make pediatric blood transfusions safer and more effective.
Importance of Timing in Pediatric Care
Timing is key in pediatric care, like with blood transfusions. It greatly affects how well a patient does. Deciding to give a blood transfusion is a big choice, and when to do it is very important.
In kids, the timing of blood transfusions can make a big difference. It can mean the difference between a good outcome and problems. As doctors, we must think carefully about when to give a transfusion.
Understanding When Transfusions are Urgent
Urgent transfusions are needed right away because of severe anemia or blood loss. In these cases, every second matters. We make sure these transfusions happen fast to help our young patients.
Some reasons for urgent transfusions include:
- Severe trauma or injury resulting in significant blood loss
- Life-threatening anemia or low blood count
- Surgical complications that require immediate transfusion
Scheduled vs. Emergency Transfusions
Scheduled transfusions are planned ahead. They help manage ongoing conditions or prepare for surgery. These transfusions are part of the patient’s treatment plan to reduce risks and improve outcomes.
Emergency transfusions, as the name implies, are unplanned and urgent. They are needed for unexpected complications or sudden changes in the patient’s condition. We know emergency transfusions can be scary for families. We promise to keep them informed and supported every step of the way.
Knowing the difference between scheduled and emergency transfusions helps us prepare families better. It ensures our patients get the best care possible.
Follow-Up Care After Transfusion
The time after a blood transfusion in kids is very important. We need to watch them closely and help them feel better. This is why follow-up care is so key.
Right after the transfusion, monitoring for side effects is a must. Blood transfusions are usually safe, but there can be risks. We need to catch any problems early.
Monitoring for Side Effects Page h3>
Side effects in kids can include fever, chills, and allergic reactions. Sometimes, serious issues like anaphylaxis or TRALI can happen. We keep a close eye on the child’s health to spot any issues fast.
To see how the child is doing, we have a plan:
- Check temperature regularly
- Monitor for signs of allergic reactions, such as rash or itching
- Observe for any changes in breathing or heart rate
| Monitoring Parameter | Normal Range | Action if Abnormal |
| Temperature | 36.5°C – 37.5°C | Notify healthcare provider if above 38°Cتام or below 36°C |
| Heart Rate | 80-120 beats per minute | Notify healthcare provider if outside range |
| Respiratory Rate | 20-30 breaths per minute | Notify healthcare provider if outside range |
Counseling with Healthcare Providers
Along with watching for side effects, counseling with healthcare providers is key. We help families take care of their child after the transfusion.
We talk about:
- Post-transfusion care instructions
- Potential complications and when to seek medical attention
- Follow-up appointment schedules
With good follow-up care, kids can do well after a blood transfusion. Our team is here to support families. We offer expert advice and care when they need it most.
Support for Families During Transfusions
When a child gets a blood transfusion, the family’s emotional health is just as key as the medical treatment. We know this time can be tough for families. So, we’re here to offer all the support we can.
Resources for Emotional Support
Families going through pediatric transfusions need emotional help. We offer counseling, support groups, and educational tools. These help families deal with the emotional side of transfusions.
Key resources include:
- Counseling services tailored to the needs of families
- Support groups connecting families with others who have experienced similar situations
- Educational materials explaining the transfusion process and its effects
Educating Families on the Process
Teaching families about transfusions is a big part of our support. We think knowing what’s happening helps families support their kids better.
| Educational Topic | Description |
| Pre-transfusion preparation | Guidance on preparing the child for the transfusion |
| Transfusion procedure | Detailed explanation of what happens during the transfusion |
| Post-transfusion care | Instructions on caring for the child after the transfusion |
We want to make transfusions easier for families. Our team is here to support families every step of the way.
Recent Advances in Transfusion Medicine
Transfusion medicine has grown a lot in recent years. This growth is thanks to new ideas that make transfusions safer and more effective. These changes are very important, but they’re even more critical for kids. Kids need precise care because their health can change quickly.
Innovations Improving Safety and Efficacy
New technology is a big part of these changes. Automated systems help prepare blood components. This makes transfusions safer by reducing mistakes. Also, pathogen reduction technologies help fight off infections that can spread through blood.
Personalized medicine is another big step forward. It means treatments are made just for each patient. This considers their genes and health history. It’s shown to make patients do better and have fewer bad reactions.
| Innovation | Description | Benefit |
| Automated Systems | Technology used for separating and processing blood components | Reduces human error, increases safety |
| Pathogen Reduction Technologies | Methods to inactivate pathogens in blood products | Minimizes risk of transfusion-transmissible infections |
| Personalized Medicine Approaches | Tailoring transfusion therapies to individual patient needs | Improves patient outcomes, reduces adverse reactions |
Research on Pediatric Transfusion Protocols
There’s a lot of research on how to best transfuse kids. Scientists are looking at what works best for different ages and health issues. They want to make sure kids get the best care possible.
There’s also interest in transfusion simulation models. These models can predict how patients will react to different treatments. This could change how doctors decide on treatments, making care even better.
“Research into pediatric transfusion medicine is key for better care. By trying new tech and methods, we can give kids the best treatment.”
—Transfusion Medicine Specialist
Conclusion: What to Expect
As we wrap up our talk on pediatric blood transfusions, it’s key for parents and caregivers to know what’s ahead. We’ve covered the basics, how long transfusions take, and the steps in the process.
Key Considerations for Families
Families need to understand the importance of pre-transfusion tests and the risks of transfusions. They also need to know about follow-up care. Knowing these things helps families handle the transfusion better.
Effective Communication with Healthcare Providers
Talking well with healthcare teams is vital for a child’s success with blood transfusions. Parents should ask questions, clear up doubts, and follow their child’s doctor’s advice.
Being informed and involved helps families make the transfusion process smoother. It meets their child’s needs and expectations.
FAQ
How long does a pediatric blood transfusion typically take?
The time for a pediatric blood transfusion varies. It depends on the patient’s age, weight, and the blood product type. Transfusions can last from a few hours to several hours.
What are the common types of blood products used in pediatric transfusions?
Pediatric transfusions often use red blood cells, platelets, plasma, and cryoprecipitate. The choice depends on the patient’s condition and the transfusion’s purpose.
How is the rate of a blood transfusion determined?
The transfusion rate is based on the patient’s condition, age, and weight. It also depends on the blood product type. The rate starts slow and increases as the patient can handle it.
What is the typical transfusion rate for platelets in pediatric patients?
Platelet transfusions usually have a rate of 10-20 mL/min. This rate can change based on the patient’s health and the doctor’s orders.
How long does it take to transfuse a unit of blood?
Transfusing a unit of blood can take 2-4 hours. But, this time can adjust based on the patient’s health and the blood product type.
What are the possible risks of pediatric blood transfusions?
Risks include allergic reactions, TRALI, and TACO. Close monitoring during the transfusion helps reduce these risks.
How are possible risks during a pediatric blood transfusion managed?
Risks are managed through careful monitoring, proper testing before transfusion, and following protocols. Healthcare providers also ensure the right blood product is given to the right patient.
Why is pre-transfusion testing important?
Pre-transfusion testing is key to ensure the donor blood matches the patient’s blood. This reduces the risk of adverse reactions.
How do families get support during the transfusion process?
Families receive support through education, emotional support, and resources. This helps them understand and cope with the experience.
What recent advances have improved pediatric blood transfusions?
Advances include better screening for infectious diseases and improved blood matching. There’s also ongoing research to optimize transfusion protocols for kids.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10940419/