Getting a stem cell transplant is a big step in fighting serious diseases. People often wonder about the hospital stay after stem cell transplant and how long they’ll remain under medical care following the procedure. The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
Key Takeaways
- The hospital stay duration varies depending on individual patient needs.
- Close monitoring is essential during the recovery period.
- Understanding the stem cell transplant recovery process helps in managing expectations.
- Factors influencing hospital stay include the type of transplant and patient health.
- Our medical team is dedicated to providing complete care throughout the hospital stay after stem cell transplant.
The Stem Cell Transplant Procedure: An Overview
For many patients, a stem cell transplant is a life-saving option. We’ll explain the basics of this complex procedure.
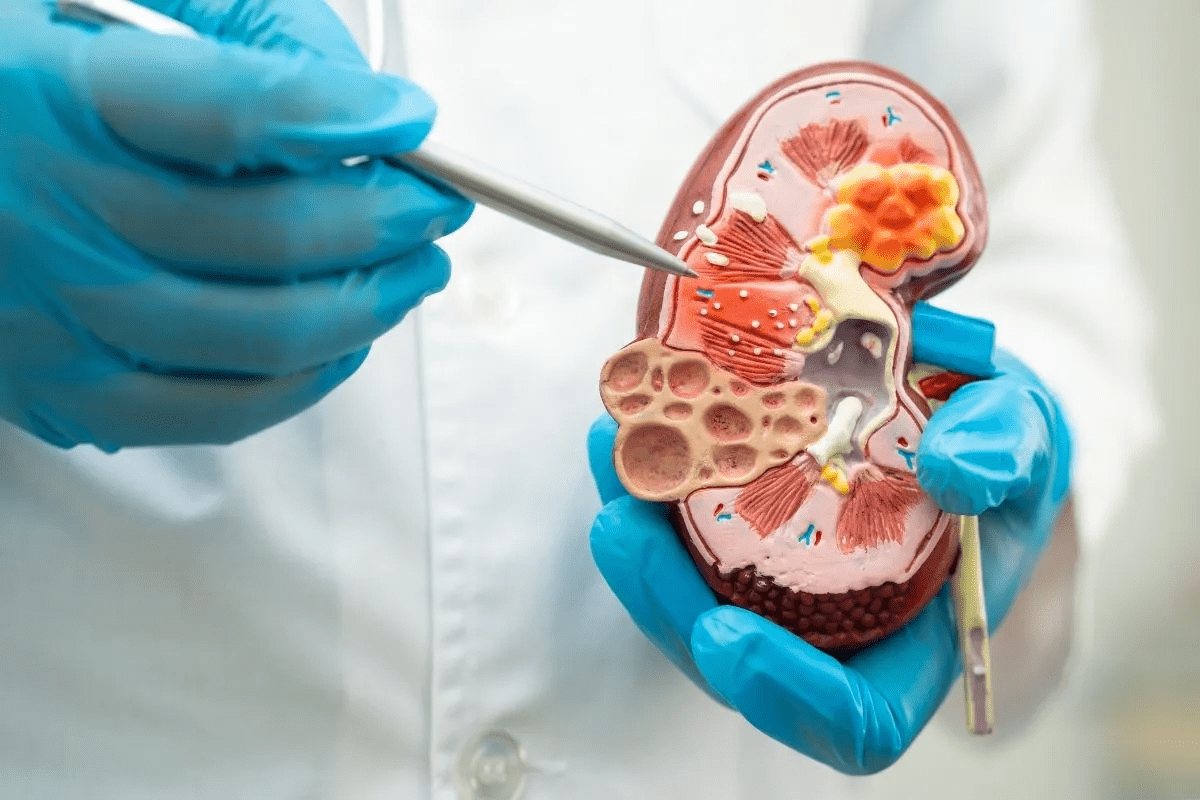
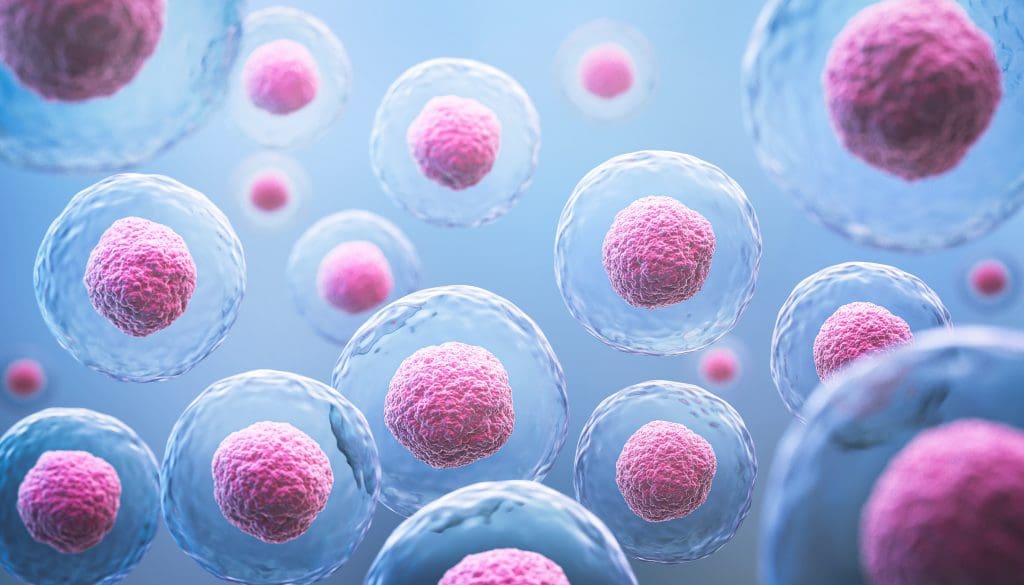
What Is a Stem Cell Transplant?
A stem cell transplant replaces damaged or diseased stem cells with healthy ones. Stem cells can become many different cell types in the body, like blood and bone cells. The goal is to help the body make healthy cells again.
It treats many conditions, including some cancers and autoimmune diseases. The process uses strong chemotherapy and radiation to weaken the immune system. Then, healthy stem cells are infused into the body.
Types of Stem Cell Transplants
There are two main types: autologous and allogeneic. Autologous transplants use the patient’s own stem cells, collected and stored for later use. Allogeneic transplants use stem cells from a donor.
Autologous transplants are common for certain cancers and autoimmune diseases. Allogeneic transplants are often used for leukemia and blood disorders.
When Is a Stem Cell Transplant Necessary?
A stem cell transplant is needed when other treatments fail. The decision is based on the disease type, stage, and the patient’s health. For some, it’s the best chance for a cure.
Medical experts say, “Stem cell transplantation is key for treating life-threatening diseases. It gives patients a chance at a longer, healthier life.” This highlights the importance of understanding this procedure.
Pre-Transplant Preparation and Evaluation
The journey to a successful stem cell transplant starts with careful preparation and evaluation. This important step makes sure patients are ready for the transplant. It helps reduce risks and increases the chance of a good outcome.
Medical Assessments and Testing
Before a stem cell transplant, patients get a full medical check-up. This check-up looks at their overall health and finds any issues that might make the transplant harder. These checks include:
- Cardiac evaluations to check the heart’s function and make sure it can handle the transplant.
- Pulmonary function tests to see how well the lungs are working.
- Infectious disease screening to find and treat any infections before the transplant.
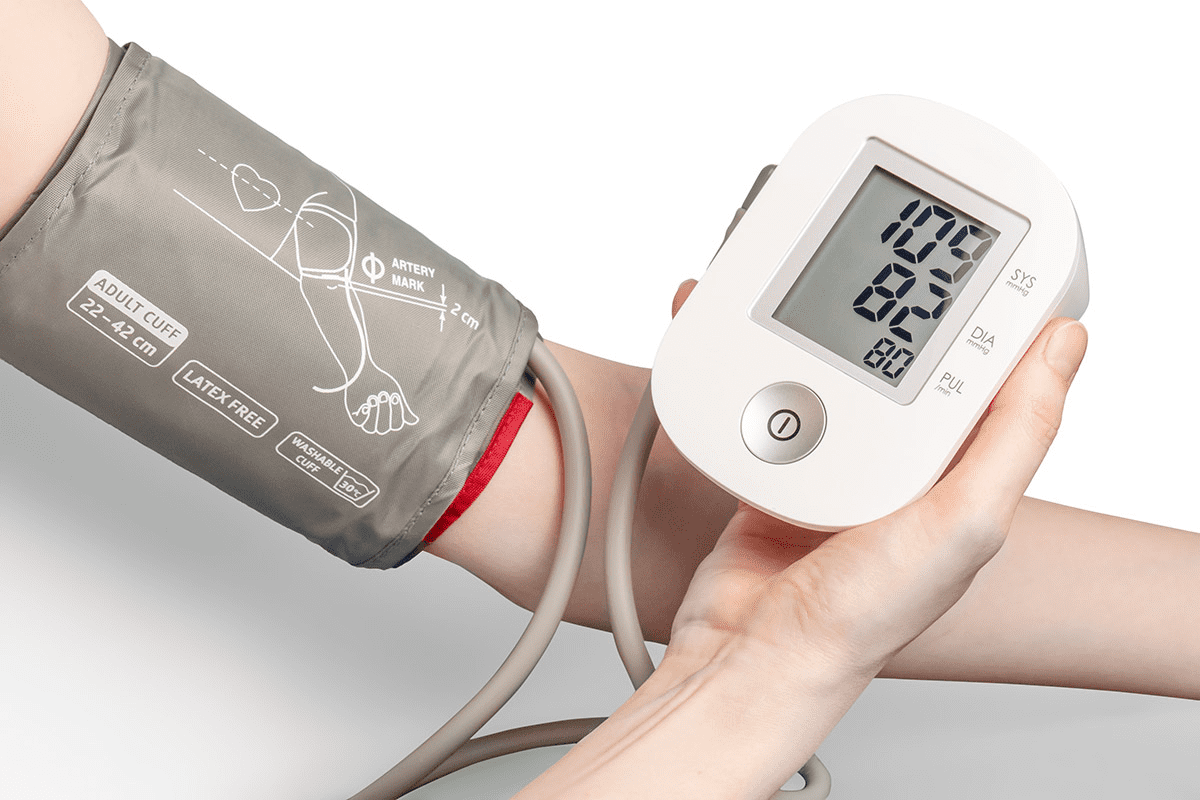
- Blood tests to check how well organs are working and the blood cell counts.
Psychological Preparation
Getting ready mentally is just as important as the medical checks. We know that a stem cell transplant can be tough on the mind. So, patients are encouraged to:
- Go to counseling sessions to talk about any worries or fears.
- Join support groups to meet others who have gone through the same thing.
- Learn coping strategies to deal with stress and keep their mind strong during and after the transplant.
Financial and Considerations
Getting ready financially is also key. Patients should:
- Check their insurance coverage to know what’s covered and what might extra.
- Look into financial assistance programs that can help with transplant .
- Plan for post-transplant care, including any treatments or rehab needed after.
By focusing on these areas, we make sure patients are ready for their stem cell transplant. This helps them have a better chance of a successful recovery.
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
To make a stem cell transplant work, a special process is needed. This process gets rid of bad cells and stops the body from rejecting the new cells. It’s a key step to get the body ready for the new stem cells.
Chemotherapy and Radiation Regimens
The process often includes high-dose chemotherapy and radiation. These treatments kill cancer cells and weaken the immune system. This makes room in the bone marrow for the new stem cells. The exact treatment depends on the disease, the patient’s health, and the transplant type.
Chemotherapy regimens vary a lot. Some use one strong drug, while others mix several. Choosing the right drugs is very important and is based on the patient’s condition and history.
Radiation therapy might be added to chemotherapy. Total Body Irradiation (TBI) is sometimes used. It kills cancer cells and weakens the immune system.
Side Effects of Conditioning
The conditioning process can cause many side effects. These include:
- Fatigue and weakness
- Nausea and vomiting
- Mucositis (inflammation of the mucous membranes)
- Hair loss
- Increased risk of infections
These side effects are usually short-term but can be serious. It’s important to manage them well to help the patient feel better and for the transplant to succeed.
Duration of Conditioning Treatment
The length of the conditioning treatment varies. It can last from a few days to a couple of weeks. The treatment’s intensity and length are carefully planned. This is to make it as effective as possible while keeping side effects down.
| Conditioning Regimen | Typical Duration | Common Side Effects |
| Chemotherapy alone | 5-7 days | Nausea, hair loss, fatigue |
| Radiation therapy alone | 1-3 days | Fatigue, skin reactions |
| Combined chemotherapy and radiation | 7-14 days | Mucositis, increased infection risk, nausea |
It’s important for patients to understand the conditioning process and its effects. By knowing what to expect, we can make their experience better and improve their chances of success.
Stem Cell Collection Methods
There are several ways to collect stem cells for transplants. Each method has its own benefits and things to consider. The choice depends on the type of transplant, the patient’s health, and if a donor is available.
Bone Marrow Harvesting
Bone marrow harvesting is a traditional way to get stem cells. It takes stem cells directly from the bone marrow, usually from the hip. This is done under anesthesia to reduce pain.
To do this, a small cut is made in the hip to insert a needle into the bone marrow. The marrow is then sucked into a syringe. The stem cells are taken out for processing.
Advantages:
- Can be used for both autologous and allogeneic transplants
Potential Complications:
- Pain and discomfort at the harvest site
- Infection or bleeding risks
Peripheral Blood Stem Cell Collection
Peripheral blood stem cell collection is more common today. It uses growth factors to move stem cells from the bone marrow into the blood. Then, they are collected through apheresis.
Apheresis is a non-surgical process. It draws the patient’s blood into a device that separates stem cells. The rest of the blood is returned to the patient.
| Method | Description | Advantages |
| Bone Marrow Harvesting | Extracting stem cells directly from the bone marrow | Rich source of stem cells, can be used for autologous and allogeneic transplants |
| Peripheral Blood Stem Cell Collection | Mobilizing stem cells into the bloodstream and collecting through apheresis | Less invasive, quicker recovery |
Each method has its own benefits and risks. The right method is chosen based on the patient’s needs. This ensures the best transplant outcome.
The Day of Transplant: What to Expect
The day of the stem cell transplant is a big step in a patient’s journey. It marks the start of a new phase in their treatment. We’ll guide you through this day to ease any worries you might have.
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
The stem cell infusion is like a blood transfusion. We give the stem cells through a special catheter. This usually takes about 30 minutes to an hour. Our team watches you closely for any signs of trouble during the infusion.
Key aspects of the infusion process include:
- Careful preparation of the stem cells
- Monitoring of vital signs
- Administration of pre-medications to prevent reactions
Immediate Post-Infusion Monitoring
Right after the infusion, we keep a close eye on you for any immediate reactions or side effects. This is key to keeping you safe and handling any issues quickly.
The following table outlines the typical monitoring protocol post-infusion:
| Monitoring Parameter | Frequency | Duration |
| Vital Signs | Every 15 minutes | First hour |
| Blood Counts | Daily | Until engraftment |
| Symptom Assessment | Continuous | Throughout stay |
We keep watching your progress and offer the care and support you need. This helps you manage side effects and recover smoothly. Knowing what happens during a stem cell transplant makes you feel more ready and confident.
Average Hospital Stay Duration for Autologous Transplants
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
Typical Timeline for Hospital Discharge
The hospital stay for these patients usually lasts from a few days to a couple of weeks. It depends on how fast their blood counts get back to normal and their health improves.
We keep a close eye on how patients are doing. They usually go home when they’re stable and can take care of themselves at home.
Factors That May Extend Your Stay
Some things can make a patient stay longer, like infections or bad side effects from treatment. We work hard to avoid these problems and help patients recover smoothly.
Key factors that may extend hospital stay include:
- Infections or sepsis
- Severe graft-versus-host disease (though rare in autologous transplants)
- Organ dysfunction
- Slow recovery of blood counts
Recovery Milestones Before Discharge
Before leaving the hospital, patients must reach certain recovery goals. These include stable vital signs, enough blood count recovery, and being able to handle their symptoms and meds at home.
We also make sure patients have support at home and know when to get medical help if needed.
| Recovery Milestone | Description | Typical Timeline |
| Stable Vital Signs | Patient’s temperature, blood pressure, and other vital signs are within normal ranges. | 1-3 days post-transplant |
| Adequate Blood Count Recovery | White blood cell count and other blood parameters show signs of recovery. | 7-14 days post-transplant |
| Symptom Management | Patient can manage symptoms such as pain, nausea, and fatigue with medication. | Varies, typically improves within 2 weeks |
Average Hospital Stay Duration for Allogeneic Transplants
Understanding the average hospital stay for allogeneic stem cell transplants is key. These transplants use stem cells from a donor. They often need a longer hospital stay than autologous transplants.
Why Allogeneic Transplants Require Longer Hospitalization
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
We keep a close eye on patients for GVHD and other issues. We adjust treatments as needed to help them recover well.
Typical Timeline for Hospital Discharge
The time it takes to leave the hospital after an allogeneic transplant varies. Patients usually go home when they’re stable and don’t need constant care.
Our team looks at many things. This includes the patient’s health, any complications, and if they can take care of themselves at home.
Engraftment and Its Impact on Hospital Stay
Engraftment is when the new stem cells start making blood cells. How fast this happens can affect how long a patient stays in the hospital.
We check engraftment with blood tests. These results tell us when it’s safe for a patient to go home.
| Transplant Type | Average Hospital Stay | Factors Influencing Stay Duration |
| Allogeneic Transplant | 3-4 weeks | Engraftment rate, GVHD, overall health |
| Autologous Transplant | 1-2 weeks | Recovery rate, complications |
Factors Affecting Length of Hospital Stay
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
Age and Overall Health
A patient’s age and health are key in figuring out how long they’ll stay in the hospital. Older patients or those with health issues might need to stay longer. We look at these factors when deciding when a patient can go home.
Type of Disease Being Treated
The disease being treated with a stem cell transplant also affects how long a patient stays in the hospital. For example, patients with leukemia or lymphoma might recover differently than others. Our team watches each patient closely to adjust their care as needed.
Donor Compatibility
For transplants from another person, how well the donor and recipient match is very important. A better match can mean a quicker recovery and possibly a shorter hospital stay. We check the match before the transplant.
Complications During Treatment
Any problems that come up during or after the transplant can also change how long a patient stays. Issues like infections or graft-versus-host disease might need more treatment and watching, making the stay longer. Our team knows how to handle these problems well.
Understanding these factors helps patients and their families know what to expect. Our team works hard to give each patient the care they need for the best recovery.
Common Complications That May Extend Hospitalization
The time after a stem cell transplant is filled with risks. Infections and graft-versus-host disease are big concerns. Knowing about these issues helps us manage them better and improve patient outcomes.
Infections and Immune System Recovery
Infections are a big risk after a stem cell transplant. The treatment before the transplant weakens the immune system. We watch for infections closely and use medicines to prevent them.
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
Graft-Versus-Host Disease
Graft-versus-host disease (GVHD) happens when the donor cells attack the recipient’s body. GVHD can be acute or chronic. We manage GVHD with careful donor selection and medicines.
The severity of GVHD can vary a lot. It’s a big factor in how long a patient stays in the hospital.
Organ Damage from Treatment
The treatment before a stem cell transplant can harm organs like the liver, lungs, and heart. This damage comes from the high-dose chemotherapy and radiation. We work with specialists to manage this damage.
The extent of organ damage affects recovery. It can make the hospital stay longer.
Nutritional Challenges
Nutritional challenges are common after a stem cell transplant. Side effects like mucositis, nausea, and diarrhea make eating hard. We create personalized nutrition plans with dietitians.
In some cases, we use supplements or intravenous nutrition. Meeting nutritional needs helps prevent complications and supports recovery.
Differences in Hospital Stays: Adult vs. Pediatric Patients
Hospital stays for stem cell transplant patients differ a lot between kids and adults. Age is a big factor in how long someone stays in the hospital. Each age group has its own needs and ways of getting better.
Age-Specific Considerations
Age-specific factors greatly affect care and hospital stay for stem cell transplant patients. Kids and adults have different recovery times and support needs.
We look at the patient’s health, the disease being treated, and donor match for hospital stay. For kids, family support is key. We involve family in the care process.
Family Support Requirements
Family support is very important for kids having stem cell transplants. We encourage family to help with care, giving emotional support and daily help.
Adults might need different kinds of support, like from friends, family, or professional caregivers. We help patients and families plan for their support needs.
Recovery Patterns by Age Group
Recovery after stem cell transplants is different for adults and kids. Kids usually recover faster because of their health and strength.
Here’s a comparison of hospital stays for adults and kids:
| Age Group | Average Hospital Stay | Common Complications |
| Pediatric (0-18 years) | 2-4 weeks | Infections, Graft-Versus-Host Disease |
| Adult (19-65 years) | 3-6 weeks | Infections, Organ Damage |
| Geriatric (65+ years) | 4-8 weeks | Organ Damage, Nutritional Challenges |
Knowing these differences helps us tailor care for each patient. This way, we can ensure the best results for both kids and adults having stem cell transplants.
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
Protective Isolation Measures
Hospitals take steps to prevent infections for stem cell transplant patients. These steps include:
- Putting you in a private room with special air filters to cut down on germs.
- Ensuring all healthcare workers and visitors wash their hands often.
- Limiting who can visit and asking visitors to wear masks and gowns.
These steps are vital when your immune system is weak. They help keep you safe during a risky time.
Daily Medical Routines
A team of and nurses will watch over you every day. Your routine will include:
- Checking your vital signs like temperature and blood pressure often.
- Doing blood tests to keep an eye on your health.
- Giving you medicine to help you get better and manage side effects.
- Doing physical checks to see how you’re doing.
These daily checks are important to catch and fix any problems quickly.
Visitor Policies and Restrictions
Hospitals have strict rules for visitors to keep you safe. These rules might be:
- Only letting a few people visit at a time.
- Stopping visits during treatments or procedures.
- Asking visitors to wear protective clothes and wash their hands.
These rules might seem strict, but they help make a safe space for you to heal.
Transitioning from Hospital to Home Care
Getting ready to leave the hospital is a big step. It’s important to know how to smoothly move to home care. This step is key for your recovery and health after a stem cell transplant.
Discharge Criteria
Before you go home, you must meet certain criteria. These ensure you’re ready for home care. They include:
- Stable vital signs and overall health condition
- Adequate blood cell counts
- Ability to manage your medication regimen
- Arrangements for follow-up care and support at home
We help you meet these criteria. This makes the transition smooth.
Setting Up Your Home Environment
Creating a good home environment is key for recovery. This means:
- Preparing a clean and comfortable space for rest and recovery
- Ensuring easy access to necessary supplies and medications
- Arranging for someone to be available to assist with daily tasks and medication management
Tip: Have a special area for your medications and supplies. This helps avoid confusion and keeps everything within reach.
Caregiver Requirements
A caregiver is often needed during the early recovery at home. They help with:
- Medication administration
- Monitoring your health and reporting any concerns
- Assisting with daily activities such as bathing, dressing, and eating
We suggest caregivers get training. This helps them support you well during recovery. They learn to recognize and manage complications.
Transitioning to home care after a stem cell transplant needs careful planning. Knowing the discharge criteria, setting up a supportive home, and having a good caregiver are key. With these steps, you can successfully move to home care and keep on the path to recovery.
Post-Discharge Follow-Up Schedule
After leaving the hospital after a stem cell transplant, patients start a critical recovery phase. This period is tough, but our team is here to help. We aim to make your transition to home care as smooth as possible.
The follow-up care plan is key to tracking your recovery. It helps manage any issues and answers your questions. Sticking to this plan is vital for a good recovery.
Frequency of Clinic Visits
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
Our team will do detailed checks during these visits. This includes blood tests to watch for engraftment and manage side effects. They also look for any complications.
Monitoring for Complications
Watching for complications is a big part of post-discharge care. Complications like infections, graft-versus-host disease (GVHD), and others can happen. We’ll teach you what to look out for and when to get help fast.
When Emergency Care Is Needed
Knowing when to get emergency care is important. If you have high fever, severe pain, trouble breathing, or other serious symptoms, call us or go to the emergency room. We’re here 24/7 to help and offer advice.
By sticking to the follow-up plan and knowing about possible complications, you can reduce risks. Our team is committed to helping you through this journey.
Variation in Hospital Protocols Between Medical Centers
Stem cell transplant protocols vary a lot between hospitals. These differences affect patient care, recovery, and results. It’s important for patients and families to understand these variations when going through stem cell transplantation.
Transplant Center Accreditation Standards
Accreditation standards are key in setting hospital protocols for stem cell transplants. Bodies like the Foundation for the Accreditation of Cellular Therapy (FACT) set strict standards. These ensure centers follow best practices in patient care and transplant procedures.
Accredited centers often have better processes and patient results. The accreditation process includes regular audits and following guidelines. These cover patient evaluation to post-transplant care.
| Accreditation Criteria | Description | Impact on Patient Care |
| Patient Evaluation | Rigorous assessment of patient suitability for transplant | Ensures that patients receive appropriate care tailored to their condition |
| Stem Cell Collection | Standards for the collection, processing, and storage of stem cells | Enhances the quality and safety of stem cells used for transplant |
| Transplant Procedures | Guidelines for the transplantation process, including conditioning regimens | Standardizes care and improves outcomes by minimizing variability |
Innovative Approaches to Reducing Hospital Stays
Transplant centers are now using new ways to shorten hospital stays. They use enhanced recovery after transplantation (ERAT) protocols. These aim to reduce complications and speed up recovery.
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
Choosing a Transplant Center
Choosing the right transplant center is very important. Look at the center’s accreditation, experience with your transplant type, and care quality.
Ask centers about their protocols, success rates, and how they handle complications. Also, consider their patient support and care coordination.
- Check for accreditation by recognized bodies like FACT
- Inquire about the center’s experience with your specific transplant type
- Evaluate the quality of care and support services offered
By carefully considering these factors, patients can make informed decisions. This can help improve their outcomes.
Outpatient Stem Cell Transplant Programs
Outpatient stem cell transplants are a new way to treat some patients. They offer more flexibility and might lower the chance of getting sick in the hospital. We’ll look at what makes outpatient stem cell transplants work, including who can get them, their benefits, risks, and how they compare to staying in the hospital.
Eligibility Criteria for Outpatient Transplants
Not every patient can have an outpatient stem cell transplant. look at several things to decide:
- Overall Health: Patients need to be pretty healthy, except for their illness.
- Disease Status: The disease’s stage and type matter a lot.
- Support System: Having a good support system at home is key for outpatient care.
Benefits and Risks of Outpatient Procedures
Outpatient stem cell transplants have some big advantages:
- The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
- Effectiveness: They can be cheaper than long hospital stays.
- Increased Comfort: Recovering at home is often more comfortable for patients.
But, there are also some downsides:
- Complications: Handling problems at home can be tough.
- Monitoring: It’s important to keep an eye on patients closely, and outpatient settings might not offer the same level of care as hospitals.
Comparing Outcomes with Inpatient Stays
Research shows that for some patients, outpatient stem cell transplants can work just as well as inpatient ones. Important factors include:
- Patient Selection: Choosing the right patients based on criteria.
- Caregiver Support: The importance of caregivers in managing care at home.
- Follow-Up Care: Regular check-ups are vital for tracking recovery and solving any issues quickly.
We keep watching and studying outpatient stem cell transplants to understand their role in treatment better.
Conclusion: Preparing for Your Stem Cell Transplant Journey
Going through a stem cell transplant is a big deal. It needs careful planning and understanding. From the start to the end, every step is important for success.
Getting ready for a stem cell transplant means more than just medical checks. It also includes mental preparation and planning for daily life. Knowing what to expect helps you face the challenges ahead.
Success in a stem cell transplant depends on being well-prepared and having support. Work with your healthcare team to make a plan that fits your needs. This way, you can increase your chances of a good outcome and a smooth recovery.
By following these steps, you can make your stem cell transplant journey as successful as possible. This leads to the best results for your health.
FAQ
What is the role of a caregiver after a stem cell transplant?
Caregivers support patients after a stem cell transplant by managing medications, monitoring for complications, and providing emotional support. Caregivers should be prepared to take on these responsibilities and have the necessary resources and support.
How does a bone marrow transplant work?
A bone marrow transplant replaces the patient’s bone marrow with healthy stem cells, from the patient or a donor. The new stem cells help rebuild the bone marrow and restore the immune system.
Is it painful to be a stem cell donor?
The discomfort of being a stem cell donor varies by collection method. Bone marrow harvesting can be painful, while peripheral blood stem cell collection may cause fatigue and other side effects. Discuss risks and discomforts with your healthcare provider.
How do I choose a transplant center?
When choosing a transplant center, look at accreditation standards, experience, innovative care approaches, and support services. Research and compare centers to find the best fit for your needs.
What are the benefits and risks of outpatient stem cell transplant programs?
Outpatient transplant programs offer reduced hospital stay and a more comfortable environment. But, they require careful patient selection and monitoring. Risks include complications that may require hospitalization.
How often should patients visit the clinic after discharge?
The clinic visit frequency depends on the patient’s condition and the transplant center’s protocols. Patients are usually seen frequently in the first few weeks to months after discharge.
What are the criteria for discharge after a stem cell transplant?
Discharge criteria include stable vital signs, adequate blood counts, and no severe complications. Patients must also have a suitable home environment and caregiver support.
How is engraftment related to hospital stay?
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
What is graft-versus-host disease?
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
How does the type of disease being treated affect hospital stay?
The type and severity of the disease can impact hospital stay. Patients with more complex or advanced diseases may need longer hospitalization.
What are the common complications after a stem cell transplant?
Common complications include infections, graft-versus-host disease, organ damage, and nutritional challenges. These can prolong hospital stay and require careful management.
How are stem cells collected for a transplant?
Stem cells are collected through bone marrow harvesting, peripheral blood stem cell collection, or umbilical cord blood collection. Each method has its own benefits and risks.
What is the conditioning process before a stem cell transplant?
Conditioning involves chemotherapy and/or radiation to prepare the body for the transplant. It can last from a few days to several weeks. This process is key for the transplant’s success.
How long does a patient typically stay in the hospital after a stem cell transplant?
The duration of the hospital stay can vary depending on the type of transplant and the patient’s overall health.
What is a stem cell transplant?
A stem cell transplant replaces damaged or diseased stem cells with healthy ones. This can be done using the patient’s own stem cells or those from a donor.