Last Updated on November 26, 2025 by Bilal Hasdemir
At Liv Hospital, we know patients often ask about heart stent limits. The number of heart stents a person can have varies. It depends on their heart’s anatomy, health, and medical condition. How many heart stents can a person have? Get the key facts on the safety limits, medical considerations, and risks of multiple stents.
Heart stents help treat heart disease and other conditions. The need for stents depends on the condition’s complexity and the person’s health. We aim for safe, effective treatments, focusing on each patient’s needs.
Our team looks at each patient’s unique situation. We aim to boost heart health while reducing risks from stent placement.
Key Takeaways
- The number of heart stents a person can have varies based on individual coronary anatomy and medical condition.
- Heart stents are used to treat coronary artery disease and other heart conditions.
- Our medical team takes a personalized approach to determine the right treatment.
- Safety and optimal outcomes are our top priorities.
- The complexity of the condition and overall health determine the number of stents required.
Understanding Heart Stents and Their Purpose
Heart stents are key in treating blocked arteries. They help restore blood flow. For those with coronary artery disease, heart stents are a vital treatment.
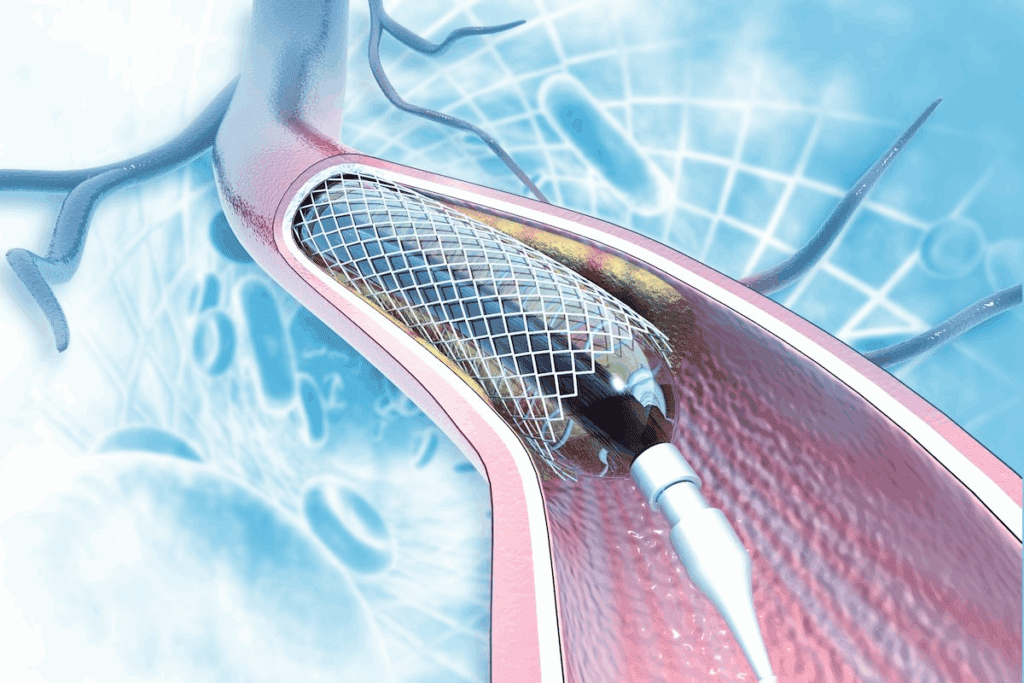
What Are Heart Stents?
Heart stents are small, metal mesh tubes. They are placed in arteries to keep them open. This improves blood flow.
How Heart Stents Work to Improve Blood Flow
Heart stents expand in the artery. They push aside blockages, restoring blood flow. This helps reduce symptoms like chest pain.
By keeping the artery open, stents improve overall heart health. They ensure the heart muscle gets the oxygen it needs.
| Function | Description |
| Keeping Arteries Open | Stents expand to push aside plaque, keeping the artery open. |
| Improving Blood Flow | By keeping the artery open, stents improve blood flow to the heart. |
| Reducing Symptoms | Restored blood flow helps alleviate symptoms like chest pain. |
Understanding heart stents helps patients see their importance. The goal is to restore safe blood flow. We consider many factors to choose the best treatment.
Medical Conditions Requiring Heart Stents
Heart stents are often needed for certain heart conditions. They are a key treatment for many heart diseases. This includes conditions that narrow or block coronary arteries.
Coronary Artery Disease and Blockages
Coronary artery disease (CAD) happens when coronary arteries narrow or block. This is due to plaque buildup. It can cause heart pain, shortness of breath, and other symptoms.
Heart stents help by opening blocked arteries. This improves blood flow to the heart. When there are severe or multiple blockages, it’s important to know how many stents can be placed in one artery.
The choice of stent number depends on the disease’s extent and complexity.
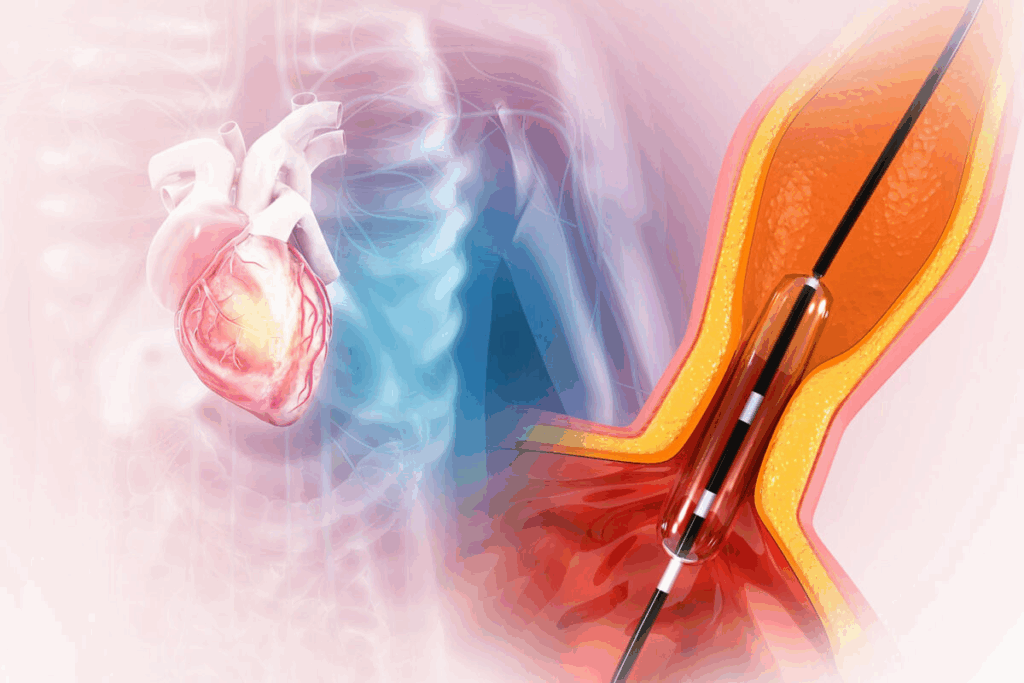
Acute Situations vs. Planned Interventions
Heart stents are used in emergencies and planned treatments. In emergencies, like heart attacks, stents quickly open blocked arteries.
For planned treatments, doctors decide after tests like angiography. The number of stents needed varies. Some patients might need 3 stents in heart or more, depending on the blockages.
| Condition | Treatment Approach | Stent Placement |
| Acute Myocardial Infarction (Heart Attack) | Emergency Angioplasty and Stenting | 1 or more stents as needed |
| Stable Coronary Artery Disease | Planned Angioplasty and Stenting | 1 or more stents based on blockage assessment |
| Multi-vessel Disease | Complex Angioplasty and Stenting | Multiple stents, potentially in multiple arteries |
It’s important for patients to understand why they need heart stents. The complexity of CAD and blockages determines the need for stents and how many heart stents can be put in.
How Many Heart Stents Can a Person Have?
To figure out how many heart stents a person can have, we need to look at their heart’s structure and past health. We’ll explore what affects the number of stents and if there’s a limit.
Is There a Maximum Limit?
There’s no exact limit on the number of heart stents a person can get. Some have had 4, 5, or even 6 stents. The choice to use more stents depends on the person’s health and how complex their heart disease is.
Key considerations include:
- The extent and severity of coronary artery blockages
- The patient’s overall health and medical history
- The presence of any comorbid conditions
- The technical feasibility of stent placement
Factors That Determine Stent Quantity
Several factors decide how many stents a person can have. These include:
- Coronary Anatomy: The shape and health of the coronary arteries are key.
- Severity of Blockages: Severe blockages might need more stents for good blood flow.
- Medical Condition: Patients with complex health issues might need more stents.
A medical expert says, “The number of stents a patient can have varies a lot. It depends on a detailed check of their heart health.”
“The goal is always to restore optimal blood flow while minimizing risks and complications.”
Having multiple heart stents can seem scary. But, thanks to new medical tech and care tailored to each person, many live well with stents. Our team is here to support and guide you through treatment.
Common Scenarios for Multiple Stent Placement
Multiple stents are needed in many cases, mainly for those with widespread blockages. This is true for complex coronary artery disease or when there are blockages in different arteries.
There are several scenarios where we need to use multiple stents. These include patients with blockages in different arteries and those with long lesions that can’t be treated with one stent.
Patients with 2-3 Heart Stents
Having 2 or 3 heart stents is common, mainly in patients with multi-vessel coronary artery disease. These patients often have blockages in multiple arteries, needing multiple stents to ensure blood flow.
For example, a patient might have a stent in the left anterior descending artery and another in the right coronary artery. Sometimes, a third stent is needed in a different branch or to cover a long lesion.
Studies show that patients with 2-3 stents can have good outcomes. They see significant improvements in symptoms and quality of life. But, they need close monitoring because of the higher risk of complications like restenosis or stent thrombosis.
Cases Requiring 4 or More Stents
Cases needing 4 or more stents are less common but can happen in patients with very complex coronary artery disease. These patients often have disease in multiple arteries and long segments of narrowing.
Having more than 4-6 stents increases the risk of complications and requires careful monitoring. The decision to use multiple stents is made based on the patient’s health, the extent of their disease, and the procedure’s technical feasibility.
| Number of Stents | Common Indications | Potential Risks |
| 2-3 Stents | Multi-vessel coronary artery disease, multiple blockages | Restenosis, stent thrombosis |
| 4 or More Stents | Complex, diffuse coronary artery disease | Increased risk of complications, need for close monitoring |
In conclusion, while multiple stents are a viable option for many, each case must be carefully assessed. Close monitoring is essential to minimize risks.
Placement of Multiple Stents in a Single Artery
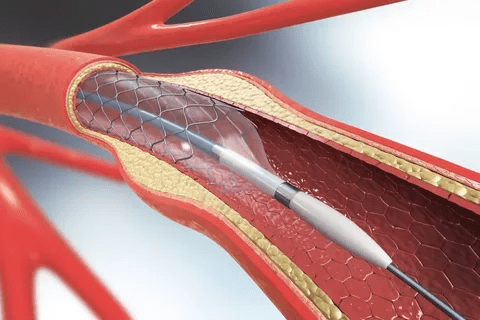
Putting multiple stents in one artery is a detailed process. It needs careful planning. When there are many blockages in one artery, doctors must think hard about how to place the stents.
Technical Considerations
When placing multiple stents, we look at the blockages’ length and severity. We also check the artery’s condition. Advanced imaging helps us see the artery and plan the stent placement.
Key factors considered during the procedure include:
- The length of the blockage
- The diameter of the artery
- The presence of any calcification or tortuosity
We use these factors to figure out the best stent placement.
Overlapping Stents and Special Techniques
Sometimes, we need to use overlapping stents to cover the blockage fully. This method needs careful planning to avoid problems like stent thrombosis or restenosis.
We also use special techniques, such as:
- Using stents of varying lengths and diameters
- Deploying stents with drug-eluting coatings to reduce restenosis
| Technique | Benefits | Potential Risks |
| Overlapping Stents | Ensures complete coverage of blockage | Increased risk of stent thrombosis |
| Drug-Eluting Stents | Reduces risk of restenosis | Requires prolonged antiplatelet therapy |
By understanding the technical aspects and using special techniques, we can place multiple stents effectively. This improves blood flow and patient outcomes.
Risks and Complications of Multiple Heart Stents
Multiple heart stents can save lives but also come with risks. Understanding these risks is key to giving patients the best care. This is true for treating coronary artery disease.
Restenosis and Stent Thrombosis
Restenosis and stent thrombosis are major concerns with multiple stents. Restenosis is when arteries narrow again after stents are placed. This can cause symptoms to come back or even heart attacks. Stent thrombosis is worse, where a blood clot forms in the stent, leading to heart attacks.
Key factors that increase the risk of restenosis and stent thrombosis include:
- Multiple stents placed in close proximity
- Stents placed in smaller arteries
- Presence of diabetes
- Incomplete stent expansion
A study in a top cardiology journal found that stent thrombosis risk is highest in the first year. This highlights the need for dual antiplatelet therapy during this time.
“The use of drug-eluting stents has significantly reduced the incidence of restenosis compared to bare-metal stents, but the risk remains, particular in complex cases.”
Long-term Medication Requirements
Patients with multiple stents need long-term antiplatelet therapy to prevent stent thrombosis. This usually means taking aspirin and a P2Y12 inhibitor like clopidogrel. The length of time for this therapy depends on the stent type and patient risk factors.
It’s vital to stick to this medication regimen. Stopping it too soon can greatly increase the risk of stent thrombosis. We help patients understand the importance of their meds and check on their adherence.
Managing patients with multiple heart stents requires a detailed approach. This includes careful stent placement and long-term management to reduce risks.
Alternatives When Multiple Stents May Not Be Ideal
For some patients, there are better options than using multiple stents. When looking at treatments for coronary artery disease, it’s key to explore all options.
Coronary Artery Bypass Grafting (CABG)
CABG is a surgery that bypasses blocked arteries with grafts. These grafts usually come from the patient’s own veins or arteries. It’s a good choice for those with complex or multiple blockages.
CABG has many benefits. It improves blood flow to the heart and may lead to better long-term results for some. The choice to have CABG depends on the patient’s health, the extent of their disease, and other factors.
Medical Management Options
Medical management for coronary artery disease includes lifestyle changes and medications. It’s effective for those with mild or stable disease.
Key parts of medical management are:
- Medications to control cholesterol, blood pressure, and blood sugar
- Lifestyle changes like diet, exercise, and quitting smoking
- Regular check-ups with healthcare providers
These strategies can lower the risk of complications and enhance quality of life.
Choosing between CABG and medical management depends on several factors. These include the disease’s severity, the patient’s health, and personal preferences.
We help patients choose the best treatment plan. We consider all options and tailor our approach to each person’s needs.
Living with Multiple Heart Stents
Living with multiple heart stents requires careful care and lifestyle changes. We know managing multiple stents can be tough. But with the right care, patients can live active and happy lives.
Follow-up Care and Monitoring
Patients with multiple stents need regular check-ups to keep stents working well. Regular visits to a cardiologist are key for checking stent function and heart health. The cardiologist might do tests like echocardiograms or stress tests.
It’s also smart to keep a medical history record. This includes info on stents, meds, and any symptoms. This record helps doctors make better care plans during visits.
Lifestyle Modifications for Stent Longevity
Some lifestyle changes can help stents last longer and keep your heart healthy. Eating a heart-healthy diet is important. This means lots of fruits, veggies, whole grains, and lean proteins. Try to avoid foods high in saturated fats, trans fats, and cholesterol.
Regular exercise is also key. Doing moderate-intensity activities like walking, cycling, or swimming for 150 minutes a week is good. It helps your heart and reduces stent risks.
Managing stress and getting enough sleep are also important. Stress and not enough sleep can harm your heart. Try meditation or yoga to manage stress.
By following up with doctors and making healthy lifestyle choices, people with multiple heart stents can stay healthy. This helps avoid complications and keeps the heart well.
Conclusion
The number of heart stents a person can have depends on their medical condition. Heart stents are used to treat coronary artery disease. The goal is to ensure blood flows safely, not to set a limit on stent use.
Coronary artery disease often requires stents to clear blockages. The number needed depends on the disease’s severity and the patient’s health. We’ve looked at cases where more than one stent is needed and the risks involved.
Deciding on the number of stents is unique for each patient. It’s based on the latest medical research and the patient’s condition. This understanding helps patients make informed decisions and work with their doctors for the best results.
FAQ
What are heart stents and how do they work?
Heart stents are small, mesh tubes used in the coronary arteries. They help improve blood flow to the heart. By expanding, they keep the artery open for safe blood flow.
How many heart stents can a person have?
The number of heart stents varies based on medical needs and condition complexity. There’s no strict limit.
What determines the number of stents a person needs?
Factors like coronary anatomy, medical condition, and overall health influence stent numbers.
Can multiple stents be placed in a single artery?
Yes, but it requires careful planning and execution.
What are the risks associated with multiple heart stents?
Risks include restenosis, stent thrombosis, and long-term medication needs.
Are there alternative treatments to multiple heart stents?
Yes, options include Coronary Artery Bypass Grafting (CABG) and medical management.
How can patients promote stent longevity and overall cardiovascular health?
Patients can promote stent longevity and cardiovascular health through lifestyle changes and regular healthcare provider visits.
Can you have 4 or more stents in your heart?
Yes, some patients may need 4 or more stents based on their condition’s complexity.
How many stents can be placed at one time?
The number of stents placed at once varies by individual case and procedure complexity.
What is the importance of follow-up care for patients with multiple stents?
Follow-up care is key for patients with multiple stents. It helps monitor their condition and adjust treatment plans as needed.
Reference
- Fröhlich, G. M., et al. (2023). Long stent implantation on the left anterior descending artery: Long-term outcomes. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC10779530