Last Updated on November 26, 2025 by Bilal Hasdemir
For those dealing with heart disease, knowing about coronary stenting is key. At Liv Hospital, we offer expert care and personalized advice. How many stents can be placed in one artery? Get the expert answer on safety limits and what factors doctors consider for your heart.
The number of stents safely placed in one artery or heart varies. It depends on the disease’s complexity, the heart’s shape, and a doctor’s evaluation.
Some might need 2, 3, or even 4 heart stents. Our team looks at each case closely to find the right treatment.
Key Takeaways
- The number of stents that can be placed depends on the complexity of coronary artery disease.
- Individual anatomy plays a key role in deciding where stents can go safely.
- Doctors must evaluate each case to figure out how many stents are needed.
- Depending on their health, patients might need more than one stent.
- Getting care that’s tailored to you is important for treating heart disease.
Understanding Coronary Stents and Their Purpose
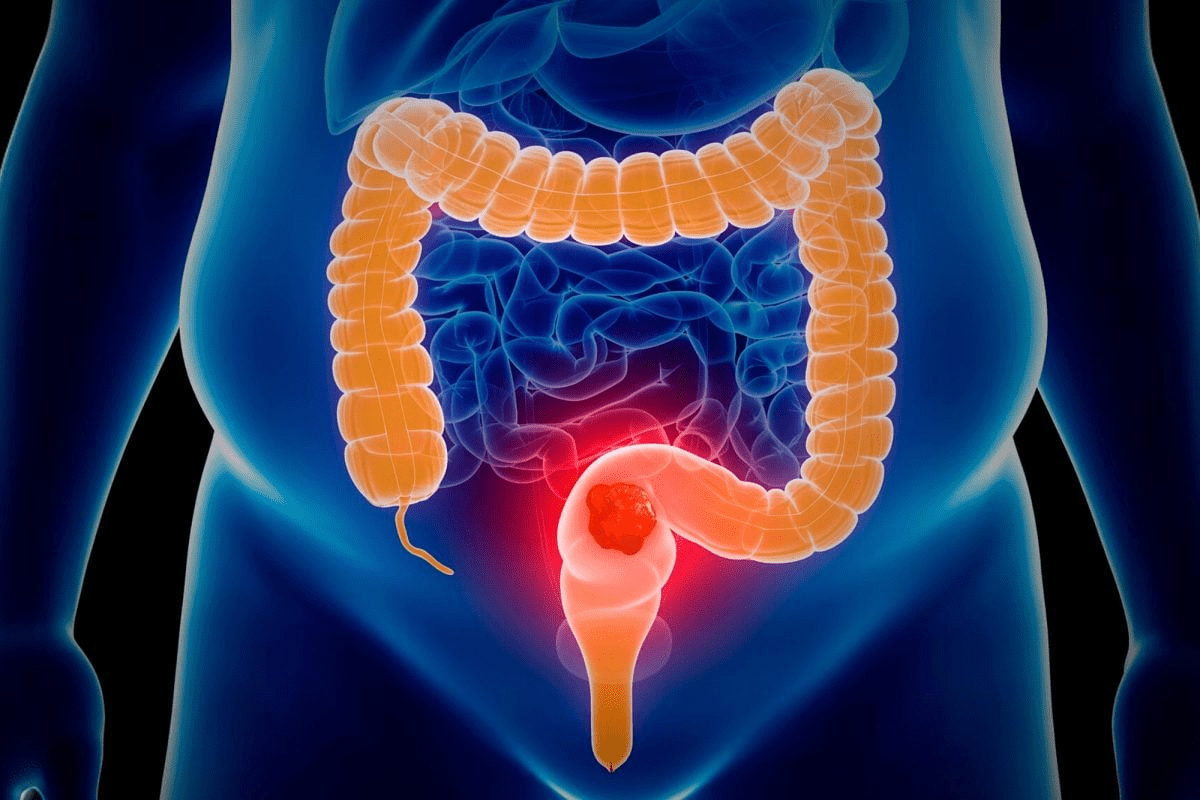
Coronary stents are small, expandable tubes that help keep arteries open. They ensure healthy blood flow to the heart. Used to treat coronary artery disease, they relieve symptoms like chest pain and shortness of breath. They also prevent heart attacks.
What Are Coronary Stents?
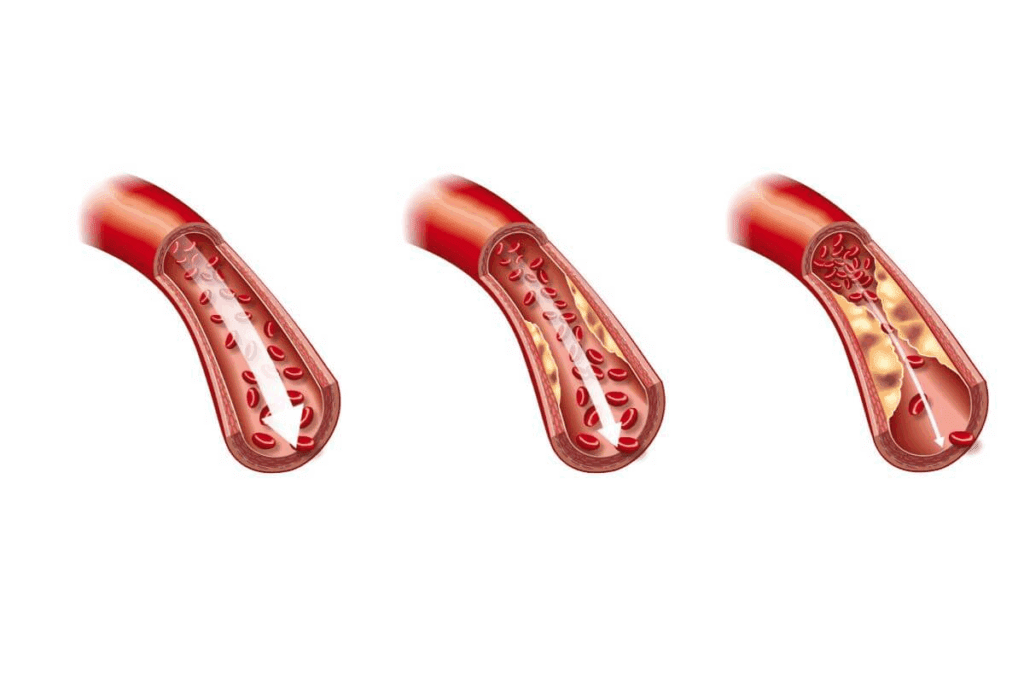
Coronary stents are made from metal mesh. They support the walls of the arteries, preventing them from narrowing again after angioplasty. A catheter guides them through an artery to the blocked area, expanding them to keep the artery open.
How Stents Work to Treat Coronary Artery Disease
Stents mechanically keep the artery open, improving blood flow to the heart muscle. This relieves symptoms and reduces the risk of heart attack. The procedure to place a stent is quick and often done on an outpatient basis.
Types of Stents Available Today
There are several types of coronary stents, each with its own benefits. The main types include:
- Bare-metal stents
- Drug-eluting stents
- Bioresorbable stents
Each stent type has its advantages. They are chosen based on the patient’s specific condition and needs.
| Stent Type | Description | Benefits |
| Bare-metal | Made from stainless steel or other metals | Less expensive, simpler design |
| Drug-eluting | Coated with medication to prevent re-narrowing | Reduced risk of restenosis |
| Bioresorbable | Made from materials that dissolve over time | Restores natural artery function, reduces long-term complications |
Understanding the different types of coronary stents is key. It helps healthcare providers and patients make the best choice. The right stent can greatly improve outcomes and quality of life.
Factors Determining Stent Placement Decisions
Many factors influence stent placement, like the patient’s health and artery details. We look at several key points to make sure treatment is safe and works well.
Arterial Anatomy and Size Considerations
The artery’s size and shape are very important. Larger arteries can handle bigger stents. Smaller ones need smaller stents or special placement methods. We also think about how twisted the artery is, as twists can make stent placement harder.
Extent and Location of Blockages
The size and where blockages are in the arteries matter a lot. Big blockages or those in key spots might need more than one stent. For example, blockages in the left main coronary artery are risky and need careful planning.
Patient-Specific Health Factors
Each patient’s health, like heart health, diabetes, and kidney function, affects stent placement. Some health issues might mean a different treatment plan, including how many stents can be used.
| Factor | Consideration | Impact on Stent Placement |
| Arterial Size | Larger vs. smaller arteries | Larger arteries can accommodate larger stents |
| Blockage Extent | Length and location of blockages | More extensive blockages may require multiple stents |
| Patient Health | Presence of diabetes, kidney function | Certain conditions may limit the number of stents |
We carefully check these factors to find the best stent placement plan for each patient. This balance helps us avoid risks while getting the most benefit from stenting.
How Many Stents Can Be Placed in One Artery
Deciding how many stents to put in one artery is complex. It depends on the artery’s size and the blockages’ extent. Cardiologists must think carefully to get the best results for patients.
There are several technical things to consider when deciding on stent placement. Let’s look at these in more detail.
Technical Limitations of Single Artery Stenting
Stenting a single artery has its limits. Cardiologists must consider:
- The size and shape of the artery
- The size and location of blockages
- The type of stent used (bare-metal, drug-eluting, or bioresorbable)
Artery size is key because it sets the maximum stent size. Larger arteries can handle bigger stents. But, the stent must fit well to avoid harming the artery wall.
Overlapping Stents: Benefits and Risks
At times, overlapping stents are needed for long or multiple blockages. This method can work well but also has risks, such as:
- Higher risk of stent thrombosis
- Possible more neointimal growth
- More complex future interventions
But, overlapping stents also have benefits, like:
- Full coverage of long or complex lesions
- Improved symptoms for patients with extensive disease
The “Full Metal Jacket” Approach in Long Lesions
For very long lesions, some doctors use the “full metal jacket” method. This involves placing stents end-to-end to cover the diseased area. While it can work, it’s not without controversy due to possible complications.
Important things to think about with the “full metal jacket” method include:
| Consideration | Description |
| Lesion Length | The longer the lesion, the more stents needed |
| Stent Type | Drug-eluting stents are often chosen for their lower restenosis risk |
| Patient Factors | Health conditions and how well they respond to antiplatelet therapy |
By carefully considering these factors, doctors can decide on the right number of stents. They aim to balance the benefits of opening up the artery with the risks and complications.
Common Multiple Stent Scenarios
Coronary artery disease sometimes needs more than one stent. This is true for complex or widespread disease. We’ll look at scenarios where more than one stent is used, like dual placement, managing multiple blockages, and complex disease.
2 Heart Stents: Common Dual Placement Cases
Putting in 2 heart stents is common. It happens when there are big blockages in different parts of the heart’s arteries. These blockages can be in the same or different arteries.
The decision to use two stents depends on the blockages’ size and location. Our team decides the best approach for each patient.
3 Stents in the Heart: Managing Multivessel Disease
When there are blockages in multiple arteries, 3 stents in the heart might be needed. This is for patients with blockages in different arteries. Stenting multiple areas requires careful planning to avoid risks.
Adding three stents is more complex than one or two. It might involve other treatments like medicine or lifestyle changes.
4 Stents in Heart: Approaching Complex Coronary Disease
For complex disease, 4 stents in heart might be the best choice. This is for patients with widespread disease in many arteries. The decision to use four stents is based on detailed evaluations.
Using four stents is a detailed process. Our team works closely with patients to manage their disease well.
Maximum Stent Placement: Pushing the Boundaries
In the field of heart treatments, we’re exploring new limits with stent placement. As we learn more about heart disease, we’re wondering how many stents are safe for a heart.
Now, doctors are placing more stents than before. This change comes from better stent technology and new ways of doing procedures.
5 Stents in Heart: Managing Diffuse Disease
When heart disease spreads, doctors might use up to 5 stents. This is common in patients with widespread disease in many arteries or long parts of one artery.
Deciding on 5 stents depends on the patient’s health, disease extent, and procedure possibility. Our cardiologists look at each patient’s unique situation to choose the best treatment.
Can You Have 6 Stents in Your Heart? Examining Rare Cases
Though rare, some patients have had 6 stents. These cases often involve complex disease or previous stent failures.
Putting in 6 stents depends on the patient’s heart function, other health issues, and procedure challenges. Sometimes, a team of doctors and surgeons works together to find the best treatment.
Record-Breaking Cases and Their Outcomes
There have been cases where patients got a very high number of stents. These unusual cases help us understand the limits of stenting.
Results for these cases vary a lot. They depend on the patient’s health, procedure complexity, and care after the procedure. We keep a close eye on these patients to ensure the best outcome and manage any issues.
How Many Stents Can Be Placed at One Time
Deciding how many stents to use at once is complex. It depends on the patient’s health, the disease’s severity, and the procedure’s details.
Single-Session vs. Staged Procedures
Choosing between a single-session or staged procedure is key. A single session means placing many stents at once. This can help those with many blockages but might raise risks. Staged procedures, done in parts, let doctors check how each stent works.
A study in the Journal of the American College of Cardiology found staged procedures safer than single-session ones for many patients.
“The decision to perform a single-session or staged procedure should be based on individual patient characteristics and clinical judgment.” says an Interventional Cardiologist
Emergency vs. Elective Stent Placements
Procedure urgency matters a lot. Emergency stents, used during heart attacks, often need multiple to quickly restore blood flow. Planned elective stents, on the other hand, allow for more careful planning.
| Procedure Type | Typical Number of Stents | Considerations |
| Emergency | 1-3 | Restoring blood flow, managing acute myocardial infarction |
| Elective | 1-2 | Careful planning, assessment of lesion complexity |
Recovery Considerations After Multiple Stent Placement
Recovery after multiple stents is important. Patients usually take antiplatelet therapy to avoid stent clotting. The therapy’s length depends on the stent count and type.
Key recovery considerations include:
- Monitoring for signs of stent thrombosis or restenosis
- Managing antiplatelet therapy
- Lifestyle modifications to reduce cardiovascular risk
In conclusion, the number of stents depends on many factors. Understanding these helps doctors make the best choices for patients.
Safety Considerations for Multiple Stent Placements
When we talk about safety with multiple stent placements, several important factors come up. The choice to use more than one stent in a heart is complex. It involves technical, anatomical, and patient-specific considerations.
Short-Term Risks and Complications
There are several short-term risks and complications with multiple stents. These include:
- Increased risk of bleeding due to antiplatelet therapy
- Potential for stent thrombosis, a blood clot inside the stent
- Risk of coronary artery perforation during the procedure
- Possible complications at the access site, like hematoma or pseudoaneurysm
Careful patient selection and precise procedural technique are key to reducing these risks. A study in the Journal of the American College of Cardiology shows that proper planning and execution can significantly lower complication risks.
Long-Term Outcomes with Multiple Stents
Long-term outcomes for patients with multiple stents are vital. Research indicates that while they manage complex coronary artery disease well, they carry a higher risk of:
- Restenosis (re-narrowing of the arteries)
- Stent failure
- Need for ongoing antiplatelet therapy
A study in the New England Journal of Medicine found that patients with multiple stents need more frequent follow-up procedures than those with single stents.
“The use of multiple stents in complex coronary artery disease requires a delicate balance between the benefits of complete revascularization and the risks of increased complexity.”
Balancing Benefits Against Possible Risks
When deciding on multiple stent placements, weighing benefits against risks is essential. This means:
- Thorough evaluation of the patient’s health and coronary anatomy
- Assessment of the extent and complexity of the coronary artery disease
- Exploring alternative treatment options, like CABG
By taking a detailed and personalized approach, healthcare providers can improve outcomes for patients needing multiple stent placements.
Alternatives When Multiple Stents May Not Be Ideal
When multiple stents aren’t the best choice for coronary artery disease, other treatments can be considered. The decision to use multiple stents depends on several factors. These include the size and location of blockages, the artery’s shape, and the patient’s health.
In cases where stents aren’t ideal, doctors look at other ways to manage coronary artery disease. These alternatives can lead to better results for patients with complex disease.
Coronary Artery Bypass Grafting (CABG)
Coronary Artery Bypass Grafting, or CABG, is a surgery that bypasses blocked or narrowed arteries. It uses a graft, often from the patient’s leg or chest, to redirect blood flow.
CABG is recommended for patients with:
- Multiple blockages in different arteries
- Complex lesions not good for stenting
- Diabetes and multivessel disease
- Failed stenting procedures before
The benefits of CABG include:
- Improved survival in certain patients
- Lower risk of future heart attacks
- Potential for full revascularization
Medical Management Options
For some, a medical management plan is the best choice. This includes lifestyle changes, medications, and regular check-ups to manage the disease.
Key parts of medical management are:
- Controlling risk factors like high blood pressure and cholesterol
- Antiplatelet therapy to prevent clots
- Medications to reduce heart workload
- Lifestyle changes like diet and exercise
A study compared medical management to revascularization strategies. It found:
| Treatment Approach | 1-Year Mortality | 5-Year Mortality |
| Medical Management | 5.2% | 18.9% |
| PCI with Stenting | 4.8% | 17.3% |
| CABG | 4.2% | 15.6% |
Hybrid Approaches to Complex Coronary Disease
Hybrid approaches have become a viable option for complex coronary disease. They combine different treatments, like CABG and PCI, for better results.
Hybrid revascularization may include:
- CABG for certain areas
- PCI with stenting for others
- Minimally invasive surgical techniques
The benefits of hybrid approaches are:
- Lower risk of CABG complications
- Flexibility in treating complex disease
- Potential for faster recovery
In conclusion, while stenting is valuable, other treatments are sometimes better. CABG, medical management, and hybrid approaches can be tailored to meet individual needs. This can lead to better long-term outcomes.
Conclusion: The Personalized Approach to Coronary Stenting
The number of stents in the heart varies greatly from person to person. There’s no single answer to how many stents a heart can have. Each person’s heart, health, and disease type are key in choosing the best treatment.
Deciding on the number of stents involves weighing their benefits against risks. We’ve seen that some patients get multiple stents successfully. Yet, others might need CABG or just medication.
It’s clear that a personalized approach to stenting is essential. Tailoring treatments to each patient’s needs can greatly improve their life quality. Whether it’s 2, 3, or more stents, the goal is to provide the best care for each unique case.
FAQ
How many stents can be placed in one artery?
The number of stents in one artery varies. It depends on the blockage’s length and complexity and the patient’s health. Sometimes, more than one stent is needed to improve blood flow.
What is the maximum number of stents that can be placed in the heart?
There’s no fixed limit on heart stents. Doctors decide based on each patient’s condition and disease complexity. It’s a case-by-case decision.
Can you have 6 stents in your heart?
Yes, in rare cases, patients might get 6 stents. This is usually for very complex cases where other treatments don’t work.
How many stents can be placed at one time?
The number of stents in one procedure varies. It depends on the patient’s health and the procedure’s complexity. Sometimes, more than one stent is used in one session. Other times, procedures are done in stages.
What are the risks associated with having multiple stents?
Stenting is generally safe, but multiple stents carry risks. These include bleeding, restenosis, and stent thrombosis. Patients should talk to their doctors about these risks.
Are there alternatives to having multiple stents?
Yes, there are alternatives. These include coronary artery bypass grafting (CABG), medical management, and hybrid approaches. The best option depends on the patient’s condition.
How many stents can a person have in their heart?
The number of heart stents varies by individual. It depends on their condition and disease complexity. Patients should discuss treatment options with their healthcare provider.
What is a “full metal jacket” approach in stenting?
The “full metal jacket” approach involves using many stents for long or complex blockages. While effective, it carries more risks. It should be used carefully.
Can stents be placed in multiple arteries?
Yes, stents can be used in multiple arteries. This is common in patients with multivessel disease. It depends on the disease’s extent and complexity.
Reference
- U.S. National Library of Medicine. (2004). Patient with recent coronary artery stent requiring major surgery. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2900091