Last Updated on November 26, 2025 by Bilal Hasdemir

Many people with heart disease wonder about the limits of stents. At Liv Hospital, we get these questions a lot. The answer isn’t simple because it depends on many things. How many stents can you get in your heart? Get the surprising facts on safety limits, risks, and what you critically need to know.
Things like how your heart’s blood vessels are shaped and how bad the disease is. We look at each case carefully to decide the best plan.
The severity and where the disease is in your heart’s arteries matter a lot. Our team uses the latest research and works together to make sure every treatment is safe and right for you.
Key Takeaways
- The number of stents a person can have is not strictly limited.
- Individual anatomy and the extent of coronary artery disease are key factors.
- Safety and technical feasibility guide the placement of each stent.
- A multidisciplinary approach ensures patient-centered care.
- The latest medical evidence supports our treatment decisions.
Understanding Coronary Stents and Their Purpose
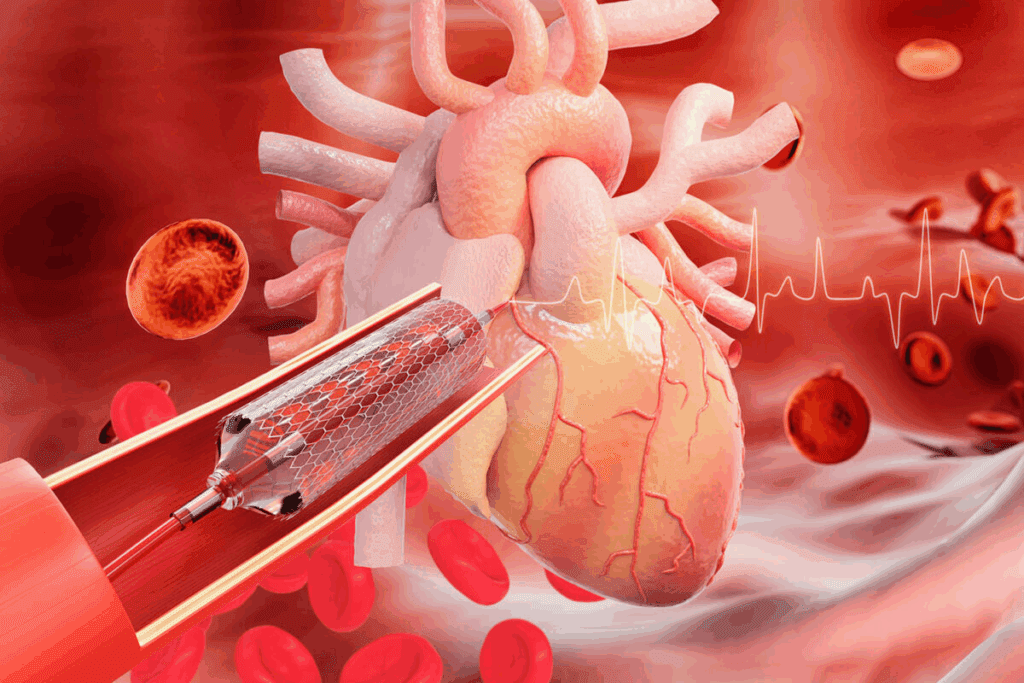
Heart stents are small, expandable tubes that help keep arteries open. They ensure blood flows well to the heart. These devices have changed how we treat coronary artery disease, a condition that can cause heart attacks.
By knowing what coronary stents are and how they work, patients can understand their treatment options better.
What Are Heart Stents?
Heart stents are small, expandable metal mesh tubes put into narrowed or blocked arteries. They keep the arteries open, improving blood flow to the heart. This is often done during an angioplasty, where the stent is placed to keep the artery open.
How Stents Work to Treat Coronary Artery Disease
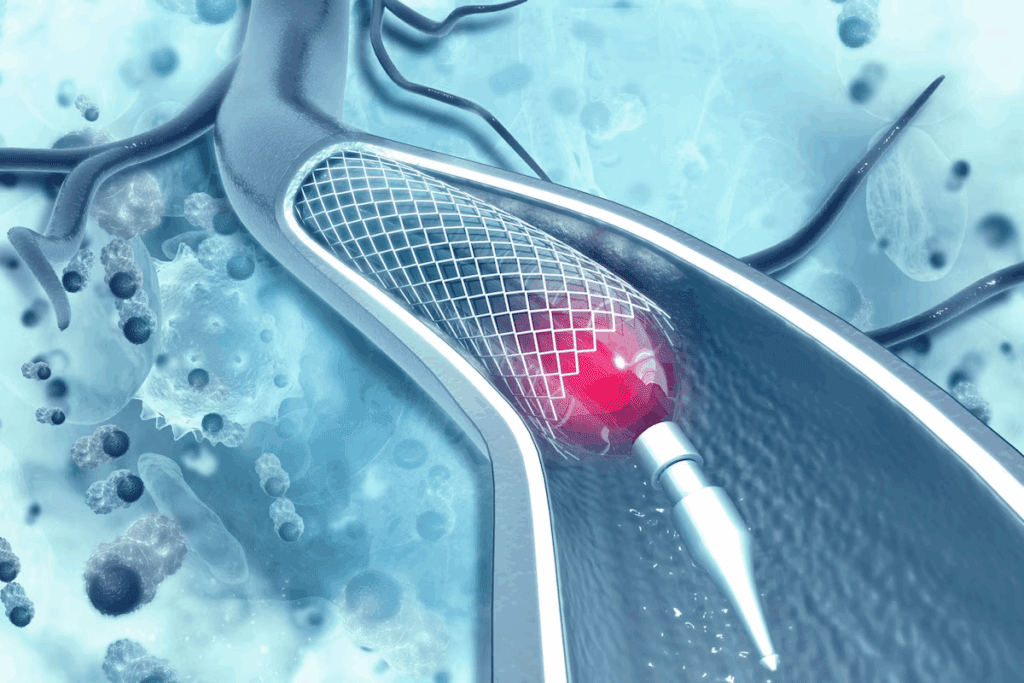
Coronary stents mechanically keep the artery open, restoring blood flow to the heart. They open up the blocked area and reduce symptoms like chest pain (angina). Over time, the stent becomes part of the artery wall.
Drug-eluting stents release medication to prevent the artery from narrowing again.
Types of Cardiac Stents Available Today
There are mainly two types of cardiac stents: bare-metal stents and drug-eluting stents. Bare-metal stents are made of metal mesh and physically hold the artery open. Drug-eluting stents are coated with medication that prevents new tissue growth, keeping the artery open.
The choice between these types depends on the patient’s health, the blockage’s location and severity, and the risk of complications.
How Many Stents Can You Get? The Truth About Numerical Limits
The number of stents a person can get varies. It depends on the patient’s health and the disease’s severity. This flexibility is key because everyone’s body is different.
The Absence of a Strict Numerical Ceiling
Unlike some treatments, stent placement isn’t limited by a strict number. There is no one-size-fits-all answer. The decision to use more stents depends on the patient’s health, disease severity, and the procedure’s success.
What Medical Literature Says About Multiple Stents
Cardiology research shows that many people have multiple stents. Studies have found cases with 5 stents in heart or more. This shows that treatment can vary a lot.
A study in a top cardiology journal found that patients with many stents do well. This is if their other health factors are good.
Having 4 stents in heart is also common. Doctors decide on this based on the disease’s extent and how well the patient responds to stents.
Factors That Influence Maximum Numbers
Several things affect how many stents a person can have. These include:
- The extent and location of arterial blockages
- The patient’s overall health status
- The technical feasibility of placing additional stents
- Individual coronary anatomy considerations
| Factor | Influence on Stent Number |
| Extent of Arterial Blockages | More extensive blockages may require more stents |
| Patient’s Overall Health | Healthier patients may tolerate more stents |
| Technical Feasibility | Complex anatomy may limit stent placement |
| Coronary Anatomy | Unique anatomy may influence stent number |
Knowing these factors helps doctors decide how many stents are right for each patient.
Remarkable Cases: Patients with Numerous Heart Stents
Patients with many heart stents show us the challenges of treating coronary artery disease. These cases help us understand the limits of stenting and how to manage complex disease.
The Patient with 67 Coronary Stents
A patient received 67 coronary stents, a record in medical history. This case makes us wonder about the reasons behind such extensive stenting and its long-term effects on health.
Managing this patient was a complex task. It involved a lot of testing, decision-making, and skill. Learning from this case can help us understand how cardiologists treat patients with many stents.
Other Documented Cases of Extensive Stenting
While the 67-stent case is rare, there are others with many stents. These cases also teach us about the outcomes of extensive stenting.
These cases often involve complex coronary artery disease with many blockages. Doctors decide on multiple stents based on the patient’s health, disease extent, and procedure feasibility.
| Case Study | Number of Stents | Key Findings |
| Patient A | 4 | Successful management of multivessel disease with minimal complications |
| Patient B | 6 | Required staged procedures due to complexity of disease |
| Patient C | 67 | Extensive stenting over multiple procedures, with ongoing management |
What We Can Learn from Extreme Cases
Extreme cases like the 67-stent patient teach us a lot. They show us how complex and varied coronary artery disease can be. They also stress the need for a personalized treatment plan.
These cases also highlight the importance of a team effort in managing complex coronary disease. By studying these cases, we can better understand what affects treatment outcomes and how to improve patient care.
Factors That Determine How Many Stents Can Be Placed
Choosing the right number of stents for a patient is complex. We’ll look at the key factors involved.
Individual Coronary Anatomy Considerations
Every patient’s coronary arteries are different. Variations in artery size, shape, and branching impact stent placement.
Extent and Location of Arterial Blockages
The size and location of blockages are critical. Larger or more critical blockages might need more stents.
Technical Feasibility of Placement
It’s important to consider if stents can be placed. This includes how easy it is to reach the blockage and if the artery is suitable.
Overall Health Status of the Patient
A patient’s overall health is also a factor. Other medical conditions can affect how many stents are safe to use.
| Factor | Description | Impact on Stent Placement |
| Coronary Anatomy | Unique variations in artery size, shape, and branching | Affects feasibility and number of stents |
| Blockage Extent and Location | Extent and location of arterial blockages | Determines necessity for multiple stents |
| Technical Feasibility | Accessibility and suitability for stenting | Influences decision on stent placement |
| Patient Health Status | Presence of other medical conditions | Affects safety and number of stents |
Healthcare professionals weigh these factors to decide on the right number of stents. They aim to balance the benefits and risks for each patient.
Typical Scenarios: Common Numbers of Heart Stents
Knowing how many heart stents a patient might get is key. It helps manage expectations and understand treatment results. We’ll look at common scenarios for heart stent use in treating coronary artery disease.
Single Stent
Many patients get just one stent. This happens when a blockage is small and can be fixed with one stent. A single stent procedure is simpler and often means a quicker recovery.
Multiple Stents in One Procedure (2-4 Stents)
Some patients get more than one stent at once. This can be 2 to 4 stents, depending on the blockages. If a patient has blockages in different places, multiple stenting is needed to fix blood flow.
Research shows that getting 2 to 4 stents at once can lead to good results. But, each case is different. Doctors consider the patient’s health and the procedure’s chances of success.
Accumulating Stents Over a Lifetime (5+ Stents)
Some patients get 5 or more stents over time. This can happen if their disease gets worse or new blockages form. While it’s safe, managing multiple stents is important to avoid problems.
- Patients with 5 or more stents need regular check-ups.
- Changing lifestyle and taking medicine as directed is key to managing the condition.
- Doctors use special strategies to reduce risks with many stents.
Understanding these scenarios helps patients make informed choices about their treatment. It prepares them for what to expect from their heart stent procedure.
Safety Considerations with Multiple Stents
Multiple stents can save lives but also bring unique safety challenges. Several key factors need to be managed carefully when considering safety with multiple stents.
Risk of Restenosis (Re-narrowing)
Restenosis, or artery narrowing, is a big worry with multiple stents. It happens when the body grows new tissue around the stent, narrowing the artery again. This risk is a major safety concern.
Thrombosis (Blood Clot) Concerns
Thrombosis, or blood clotting, is another serious issue. It can cause heart attacks or strokes. With more stents, the risk of thrombosis goes up, making careful monitoring key.
Medication Requirements with Multiple Stents
Patients with multiple stents need long-term medication to prevent clots. This medicine is vital but can also cause bleeding. Managing these medications gets more complicated with more stents.
Cumulative Risks with Each Additional Stent
Each extra stent adds to the risks. Studies show more stents mean more chances of restenosis and thrombosis. Knowing these risks helps in making better stent placement decisions.
To understand the risks of multiple stents, let’s look at some data:
| Complication | Single Stent | Multiple Stents |
| Restenosis | 5-10% | 15-25% |
| Thrombosis | 1-2% | 3-5% |
| Bleeding Complications | 2-5% | 5-10% |
In conclusion, while multiple stents are valuable, safety must be carefully considered. Understanding the risks of restenosis, thrombosis, and medication management helps in making informed decisions about stent placement.
Placement Locations: Where Can Stents Be Inserted?
Coronary stents can be placed in different parts of the heart. The choice depends on several factors. They are mainly put in native coronary arteries and bypass grafts. Knowing these spots and their needs is key for good treatment.
Stenting Native Coronary Arteries
Native coronary arteries supply blood to the heart muscle. Stenting these arteries is a common treatment for heart disease. The decision to use a stent depends on the blockage’s severity and the artery’s health.
“Stents in native coronary arteries have changed how we treat heart disease,” says a top cardiologist. “It helps restore blood flow to the heart with little invasion.”
Stenting Bypass Grafts
Bypass grafts are put in to bypass blocked or narrowed coronary arteries. Over time, they can get diseased too. Stenting these grafts is a less invasive option compared to repeat surgery.
When thinking about stenting bypass grafts, the graft’s condition and the patient’s health are key. The graft’s type and location also matter in deciding if stenting is right.
Limitations in Certain Arterial Locations
Stenting is versatile but not for all arteries. Very small or large arteries, or those with complex shapes, might not get stents. Heavy calcification or widespread disease can also make stenting hard.
Choosing where to put a stent requires careful thought. Advanced imaging and tests help doctors pick the best treatment for each patient.
In summary, stents can be a good treatment for heart disease in both native arteries and bypass grafts. But, the decision on where to place stents must consider the patient’s specific situation. This includes the arteries’ characteristics and the patient’s overall health.
When Multiple Stents May Not Be the Best Option
For some patients, using multiple stents might not be the best choice. Stenting is a common way to treat heart disease. But, certain conditions might need different treatments.
Indications for Coronary Bypass Surgery Instead
When patients have complex heart disease, surgery might be better than stents. Coronary artery bypass grafting (CABG) is a surgery that bypasses blocked arteries. It uses grafts from the patient’s leg or chest.
This surgery is often recommended for:
- Multiple blockages in different coronary arteries
- Complex lesions that are hard to stent
- Diabetes, as CABG has better long-term results for diabetics
A heart team decides if CABG is better than stenting. They look at the patient’s health, the extent of heart disease, and other factors.
Medical Management Alternatives
For some, managing heart disease with medicine might be the best choice. This approach controls symptoms and slows disease growth. It’s good for patients with:
- Mild symptoms that are well-controlled with medication
- Small vessel disease that can’t be treated with stents or surgery
- Significant comorbidities that raise the risk of complications
Medical management includes lifestyle changes and medicines. It aims to manage cholesterol, blood pressure, and other heart risks.
The Stent vs. Surgery Decision for Multivessel Disease
Choosing between stenting and CABG for multivessel disease is complex. Stenting is less invasive and has a quicker recovery. But, CABG might offer better long-term results, even for complex cases or diabetes.
The decision depends on the patient’s heart anatomy, left ventricular function, and overall health. Advanced imaging, like coronary angiography and cardiac CT scans, helps in this evaluation.
In the end, the choice between stenting, CABG, or medical management depends on the patient’s specific situation. It considers their preferences, lifestyle, and health.
The Decision-Making Process for Additional Stents
Deciding on more stents is complex and tailored to each person. A team of healthcare experts carefully evaluates each case.
The Heart Team Approach
A team of cardiologists, surgeons, and specialists is key in this decision. They work together to explore all treatment options.
They discuss the patient’s medical history, symptoms, and test results.
Diagnostic Tests That Guide Decisions
Several tests help decide if more stents are needed. These include:
- Coronary angiography to see the arteries
- Stress tests to check the heart’s function
- Cardiac imaging tests like echocardiography or MRI
Patient-Specific Factors in Consideration
Each patient’s health, other conditions, and past treatments are considered. Their lifestyle, preferences, and values are also important.
Shared Decision-Making with Patients
Healthcare teams and patients work together in shared decision-making. This ensures the patient is informed and involved.
Together, we make choices that meet the patient’s needs and wishes.
Living with Multiple Heart Stents
Having multiple heart stents means more than just the surgery. It also means ongoing care and changes in lifestyle. It’s important to know how to manage with multiple stents for good heart health.
Long-Term Medication Requirements
People with multiple stents need to take medicine for a long time to stop blood clots. Sticking to the medication is key to avoiding serious problems like stent blockage. Doctors usually prescribe two medicines for a while, then one for life.
- Aspirin is often used to prevent blood clots.
- P2Y12 inhibitors like clopidogrel might be added to aspirin.
Follow-Up Care and Monitoring
Regular check-ups are important to keep an eye on the stents and heart health. Tests like stress tests and echocardiograms help check how well the heart is working and spot any problems early.
“Regular monitoring is key to managing patients with multiple stents effectively.” – A well known Cardiologist
Lifestyle Modifications for Stent Longevity
Changing your lifestyle can help your stents last longer. Eating well, exercising, and quitting smoking are good steps. A heart-healthy diet with lots of fruits, veggies, and whole grains is advised. Regular exercise, like walking fast, also helps your heart.
Managing Expectations and Quality of Life
It’s important to manage your expectations and keep a good quality of life. Know the signs of trouble, like chest pain or trouble breathing, and when to get help. By staying informed and careful, people with multiple stents can live well.
For example, someone with 4 stents can live a good life by following the right diet and medicine. The main thing is to stay informed and take care of your heart.
Conclusion: Understanding Your Heart Stent Journey
Understanding heart stents is key for those dealing with coronary artery disease. We’ve looked at how many stents you can have. It depends on your heart’s shape and size.
The number of stents needed can vary a lot. Some people might have 3 stents, while others need more. Doctors decide based on tests and a team approach.
Managing multiple stents is important. Patients need to take medicine and make lifestyle changes. This helps keep the stents working well and keeps the heart healthy.
Knowing about stents helps patients make better choices. It’s all about getting the best care for those with heart disease and stents.
FAQ
How many stents can be placed in the heart?
The number of stents in the heart depends on several things. These include the heart’s anatomy, the blockages’ extent and location, and the patient’s health.
Is there a limit to the number of stents a person can have?
There’s no exact number limit for stents. But, doctors consider many factors, like the disease’s severity and the patient’s health, before adding more stents.
How many stents can be placed at one time?
During one procedure, usually one to four stents are placed. This depends on the case’s complexity and the patient’s condition.
Can you have multiple stents in the same artery?
Yes, it’s possible to have multiple stents in one artery. This choice is made based on the blockage’s length and severity.
What are the risks associated with having multiple stents?
More stents mean higher risks. These include restenosis, thrombosis, and needing long-term medication.
How many stents can a person have in their lifetime?
There’s no limit to the number of stents over a lifetime. Each case is evaluated based on the patient’s health and disease severity.
Can you have 6 stents in your heart?
Having six stents is possible but complex. The decision depends on the patient’s health and disease severity.
What is the maximum number of stents that can be placed?
There’s no set maximum for stents. It varies based on the patient’s anatomy and disease extent.
How many stents can be put in heart arteries?
The number of stents varies by case. It considers blockage severity, location, and patient health.
Are there any alternatives to having multiple stents?
Yes, alternatives like coronary bypass surgery or medical management are considered. They depend on disease severity and complexity.
Reference
- Fröhlich, G. M., et al. (2023). Long stent implantation on the left anterior descending artery: Long-term outcomes. PMC.