Last Updated on December 2, 2025 by Bilal Hasdemir
Every year, millions of children worldwide need blood transfusions for many reasons. This could be due to medical conditions, surgeries, or injuries. It’s very important to get the transfusion volume just right for their treatment to be safe and effective. Explaining the calculation methods used in pediatrics to determine How much blood is in a transfusion for a child’s safe dose.
Figuring out the right amount of blood for kids is not easy. It depends on their age, weight, and health. Blood volume calculations are complex. Healthcare providers must use certain rules and formulas to make sure the right amount of blood is given.
Key Takeaways
- Getting the blood transfusion volume right is very important for kids.
- The patient’s age, weight, and health are key in figuring out the right amount.
- There are specific rules and formulas to help find the right volume for kids.
- Pediatricians must think about the type of blood product and how sick the patient is.
- Safe and effective blood transfusions are key for good care outcomes.
Understanding Blood Transfusion Basics
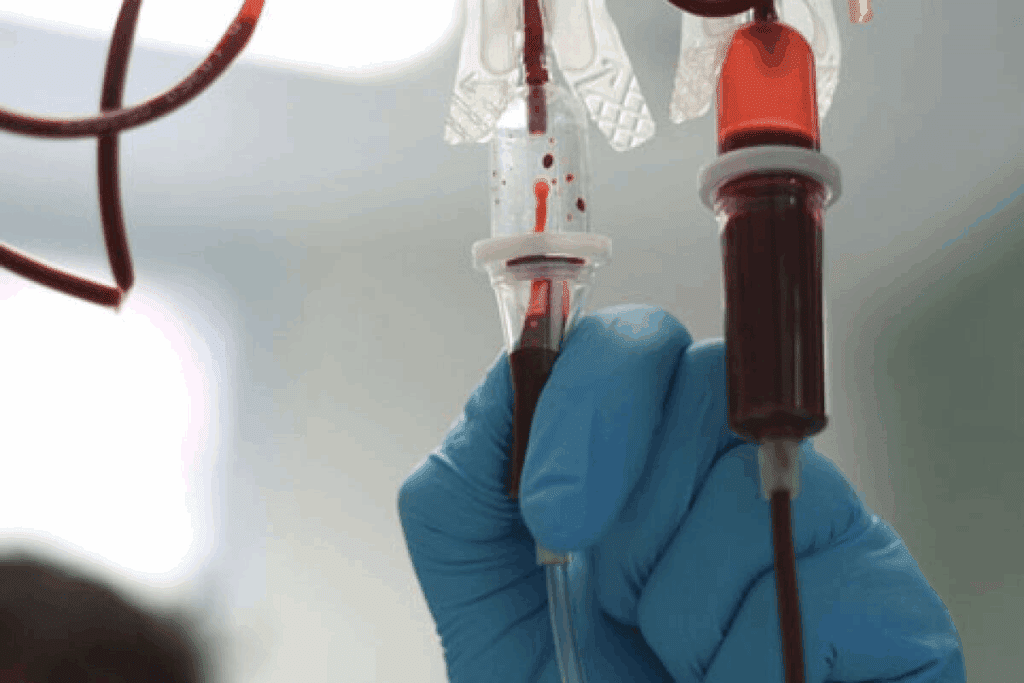
Blood transfusions move blood or parts of it into a patient’s blood to help with health issues. We’ll look at the basics of blood transfusions. This includes the types of blood products and why they’re needed.
What is a Blood Transfusion?
A blood transfusion adds blood or parts of it to a patient’s blood. It’s key for patients in surgery, with injuries, or with anemia or autoimmune hemolytic anemia (AIHA). AIHA makes the immune system attack the patient’s own red blood cells.
AIHA needs careful handling, and blood transfusions can save lives. We’ll dive into blood transfusions to see their role in patient care.
Types of Blood Products Available
Blood banks break down whole blood into parts like red blood cells, platelets, plasma, and cryoprecipitate. Each part helps with different health issues. For example, red blood cells boost oxygen to tissues, and platelets stop bleeding in cases of low platelets.
| Blood Component | Primary Use |
| Red Blood Cells | To increase oxygen delivery to tissues |
| Platelets | To prevent or treat bleeding due to thrombocytopenia |
| Plasma | To replace clotting factors and manage bleeding disorders |
| Cryoprecipitate | To replace fibrinogen and other clotting factors |
Why Are Transfusions Needed?
Blood transfusions help with severe anemia, trauma, surgery, and bleeding disorders. The choice to transfuse depends on the patient’s health, lab results, and their condition. Knowing why transfusions are needed helps doctors make better decisions for patients.
Understanding blood transfusions shows their complexity and importance. We’ll keep exploring their details in the next sections.
Factors Influencing Transfusion Volume
Pediatric blood transfusions need careful calculations. This is because each patient is different. The right amount of blood to give depends on many factors.
Patient’s Age and Weight
The age and weight of a child are key in figuring out how much blood they need. Weight-based calculations are very important. They help us guess how much blood a child has, which is vital for the transfusion.
A study found that kids have about 70-80 mL of blood for every kilogram of their weight. This helps doctors know exactly how much blood a child needs.
Medical Condition and Severity
The type of medical issue and how serious it is also matter. Kids with severe anemia or those having surgery might need more or less blood. The severity of the condition often dictates the urgency and volume of the transfusion.
“The severity of anemia in patients with COVID-19 is associated with the risk of in-hospital mortality,” highlighting the importance of accurate transfusion practices in critical care.
Guidelines from Organizations
Many healthcare groups have rules for blood transfusions, including for kids. These rules tell us how much blood to give and what to consider. We follow these guidelines to make sure our care is up-to-date and based on the latest research.
| Organization | Guideline | Recommended Volume |
| AABB | Pediatric Transfusion Guidelines | 10-15 mL/kg |
| American Academy of Pediatrics | Blood Transfusion in Children | Variable based on condition |
How Much Blood is Typically Used?
The amount of blood used in transfusions varies a lot between adults and kids. This is because their needs are different. Doctors must think about the patient’s age, weight, and health when deciding how much blood to give.
Standard Volumes for Adults vs. Children
Adults usually get about 1 unit of blood, which is 450-500 mL. But kids get blood based on their weight, about 10-15 mL/kg. This shows why kids need special care with blood transfusions.
For kids, figuring out how much blood to give is very important. Weight-based calculations help make sure they get the right amount.
Differences in Pediatric Transfusions
Kids need special attention when it comes to blood transfusions. Their age, weight, and health all play a part. For example, babies and toddlers need different amounts of blood than older kids. Hematological reference intervals also change with age and gender in teens, making it even more complex.
Understanding Unit Requirements
A unit of blood is a standard, but the actual amount can vary a bit. Knowing this is key for both adults and kids to make sure transfusions are safe and effective. Below is a table showing typical blood volumes for different age groups.
| Age Group | Typical Blood Volume (mL/kg) | Example Volume for a 10 kg Child |
| Neonates | 80-100 | 800-1000 mL |
| Infants | 70-80 | 700-800 mL |
| Children | 70-80 | 700-800 mL |
| Adults | N/A | 450-500 mL (1 unit) |
By knowing these differences and using the right calculations, doctors can make sure patients get the right amount of blood for their needs.
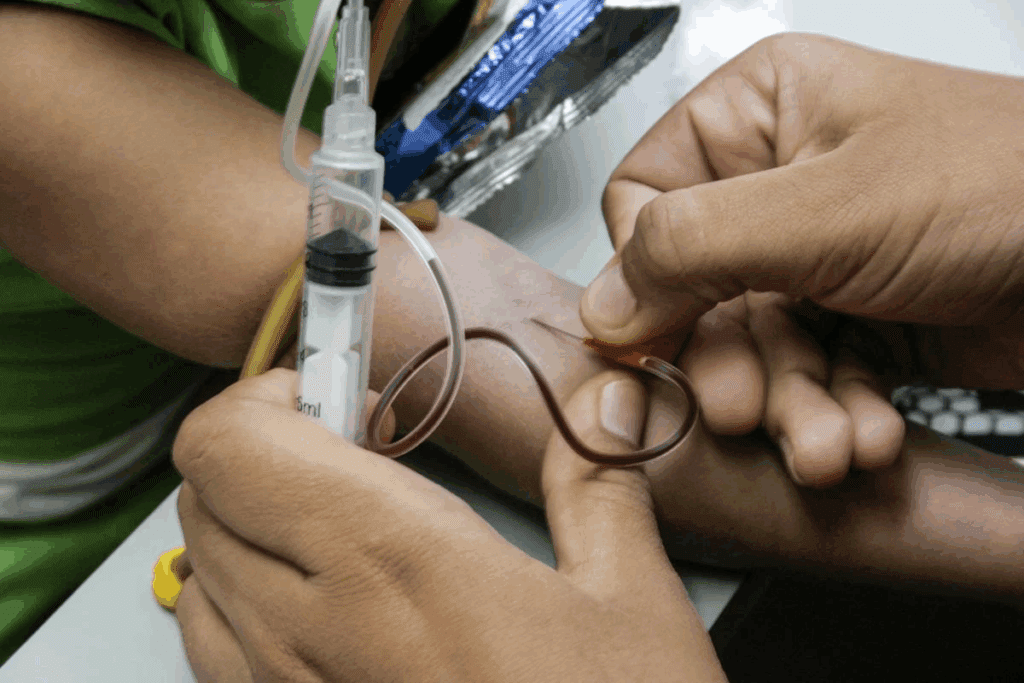
Calculating Blood Transfusion for Children
Getting blood transfusions right is key in kids’ care to avoid problems. We must think about several things to make sure the right amount is given.
Weight-Based Calculations
Weight-based calculations are very important for kids. They help us figure out how much blood they need. The formula uses the kid’s weight in kilograms. It looks like this: Transfusion Volume (mL) = Weight (kg) x Desired Hemoglobin Increment (g/dL) x Factor. The factor changes based on the blood type.
Formula for Determining Volume
The formula for blood transfusion volume considers the kid’s weight and the needed hemoglobin level. For red blood cells, it’s: Volume (mL) = Weight (kg) x 3-4 mL/kg per g/dL of desired hemoglobin increment. This helps keep the hemoglobin level right without giving too much blood.
Example Calculation:
| Weight (kg) | Desired Hemoglobin Increment (g/dL) | Transfusion Volume (mL) |
| 10 | 3 | 90-120 |
| 20 | 2 | 120-160 |
Adjustments for Special Needs
Some kids might need special calculations because of their health. For example, kids with heart problems might need careful fluid management. We look at each kid’s needs and health history carefully.
“The key to successful blood transfusion in pediatric patients lies in meticulous calculation and careful monitoring.”
– Expert in Pediatric Hematology
By using these guidelines and weight-based calculations, we can make sure kids get the right amount of blood. This helps keep them safe and improves their treatment results.
Monitoring During Blood Transf Page Page transfusions
Monitoring blood transfusions closely is key to avoiding and handling bad reactions. We know that keeping a close eye on our pediatric patients is essential. It ensures their safety and well-being during transfusions.
Importance of Close Observation
Watching closely helps healthcare teams spot issues fast. They can then act quickly. This means checking vital signs like temperature, blood pressure, and heart rate often. They also look out for any signs of a bad reaction.
Key aspects of close observation include:
- Continuous monitoring of vital signs
- Regular assessment of the patient’s overall condition
- Prompt reporting of any changes or concerns
Recognizing Signs of Reactions
Spotting signs of bad reactions is vital for managing them well. Common issues include allergic reactions, febrile non-hemolytic transfusion reactions, and transfusion-related acute lung injury (TRALI). We stress the need to know these to care for patients quickly.
“Early detection of adverse reactions can significantly improve patient outcomes.”
— American Society of Hematology
Timing and Duration of Infusion
The timing and how long the infusion lasts are also very important. The transfusion rate must be controlled carefully to avoid problems. We stick to guidelines to set the right rate based on the patient’s health and the blood product.
Factors influencing infusion timing include:
- The patient’s cardiovascular stability
- The volume of blood being transfused
- The presence of any underlying medical conditions
Risks and Page Page szemp Complications of Transfusions
Blood transfusions in kids come with risks and complications. They are vital in medical care but can have side effects.
Common Risks Associated
There are several risks with blood transfusions. These include transfusion-related acute lung injury (TRALI) and transfusion-associated circulatory overload (TACO). TRALI causes lung problems due to antibodies in the blood. TACO happens when the body can’t handle the extra blood.
Allergic reactions and infections are also risks. Though infections are rare, thanks to strict screening. Iron overload is a concern for kids needing many transfusions.
Managing Adverse Reactions
Quick action is key when managing blood transfusion reactions. We watch patients closely for signs of trouble. If a reaction is seen, we stop the transfusion right away and start treatment.
For allergic reactions, we might give antihistamines or steroids. Severe reactions like anaphylaxis need epinephrine. TRALI and TACO are treated with supportive care like oxygen and diuretics.
Preventive Measures and Best Practices
We take steps to reduce risks with blood transfusions. This includes choosing the right blood and giving it at the right rate. We also focus on safe blood handling and storage.
Monitoring patients during and after transfusions is critical. This helps catch any problems early. By following these steps, we make blood transfusions safer for kids.
Emotional Support for Pediatric Patients
Blood transfusions can be scary for kids. That’s why emotional support is key. We know it’s tough for both the kids and their families. Giving them the best emotional support is vital for their health.
Preparing Young Patients for Transfusions
Explaining blood transfusions to kids is important. We use simple words they can understand. For instance, we tell them it’s like getting a special medicine to make them feel better.
Child life specialists are also a big help. They know how to support kids during medical procedures. They teach parents how to prepare their child and help them cope.
Involving Families in the Process
It’s important to involve families in the transfusion process. We encourage parents to be there for their child. Their presence can really help the child feel more secure.
Working together with families makes the experience better. It helps reduce anxiety and makes the whole thing more positive.
Resources for Emotional Well-being
Emotional support doesn’t stop after the transfusion. We offer many resources to help kids and families deal with their feelings. This includes counseling, support groups, and educational materials.
As one expert said,
“The emotional care of pediatric patients is just as important as their medical treatment. By providing complete support, we can enhance their outcomes and quality of life.”
We aim to give this level of care to every child who needs a blood transfusion.
Follow-Up Care Post-Transfusion
The time after a blood transfusion is very important. We must watch how the patient is doing to see if the transfusion worked. This helps us catch any problems early.
Importance of Monitoring Recovery
Watching how a patient recovers after a blood transfusion is key. It lets doctors know if the transfusion helped and if there are any bad reactions. We check the patient’s vital signs and adjust treatment as needed.
Important things to watch during recovery include:
- Vital signs like temperature, blood pressure, and heart rate
- Laboratory results, including hemoglobin and hematocrit levels
- Signs of possible complications, like allergic reactions or TRALI
Assessing Hemoglobin Levels
Checking hemoglobin levels is a big part of follow-up care. We do this to make sure the transfusion works and the patient is getting better. We also use a formula to make sure we don’t give too much or too little blood.
| Parameter | Pre-Transfusion | Post-Transfusion |
| Hemoglobin (g/dL) | 8.0 | 12.0 |
| Hematocrit (%) | 25 | 35 |
Recognizing Long-Term Impacts
It’s important to think about the long-term effects of blood transfusions. We look for possible problems like iron overload or graft-versus-host disease. Our follow-up care aims to protect the patient’s health in the long run.
Some long-term effects to watch for include:
- Iron overload from getting transfusions too often
- Graft-versus-host disease, a serious but rare issue
- Immunosuppression, which can lead to more infections
Collaborating with Healthcare Teams
Collaboration is key to safe and effective blood transfusions in healthcare. Healthcare providers work together to ensure the best care for patients.
Roles of Nurses and Doctors
Nurses and doctors are vital in blood transfusions. Nurses watch over patients closely, ready to act if needed. Doctors order transfusions and oversee the whole process.
Both roles need clear communication and teamwork. This ensures transfusions are done safely and right.
| Professional | Key Responsibilities |
| Nurses | Monitoring transfusions, patient care, and reacting to adverse reactions |
| Doctors | Ordering transfusions, assessing need, overseeing the process |
Importance of Communication
Good communication among healthcare teams is critical. It helps avoid mistakes and ensures blood transfusions are done right. We use electronic health records and direct talk to keep everyone informed.
- Clear instructions for transfusion procedures
- Regular updates on patient status
- Prompt reporting of any adverse reactions
Team Protocols for Safety
Healthcare teams follow strict protocols for blood transfusions. They check the blood product against the patient’s identity and watch the patient closely.
- Verifying patient and blood product identity
- Monitoring vital signs during transfusion
- Having emergency protocols in place
Advances in Blood Transfusion Practices
Recent changes in blood transfusion have greatly improved patient care. We’re in a new era of transfusion medicine. This is thanks to new tech, better safety rules, and a deeper understanding of patient needs.
Innovations in Blood Type Matching
Blood type matching has seen big improvements. Precision medicine helps us understand blood types better. New tech makes matching more accurate and quick, lowering the chance of bad reactions.
- Advanced genotyping finds rare blood types, making sure patients get the right blood.
- Automated systems for blood typing and cross-matching cut down on mistakes, making patients safer.
Reduced Risks of Transfusion-Related Conditions
Complications from blood transfusions can be serious. But, new screening and processing methods have cut down these risks. We now have better ways to find pathogens and contaminants in blood donations.
| Risk Factor | Previous Rate | Current Rate |
| Transfusion-transmitted infections | 1 in 100,000 | 1 in 500,000 |
| Adverse reactions | 5% | 2% |
Future Trends in Pediatric Care
Pediatric care is set to get even better with personalized medicine. Blood transfusions will be made to fit each child’s needs. We expect to see even fewer risks and better results.
- New artificial blood substitutes could change how we do transfusions.
- Gene therapy might help treat conditions that need frequent transfusions.
As we keep improving blood transfusion, our main goal is to make care safer and better. We want to help our young patients and their families with compassion and care.
Educational Resources for Parents
Understanding blood transfusions for kids can be tough for parents. We know how important it is to help them care for their children. That’s why we provide educational resources.
Trusted Information Sources
Parents can find reliable info on blood transfusions from trusted organizations. These sources give a lot of knowledge. They help parents make good choices for their child’s health.
Support through Workshops and Groups
Workshops and support groups are great for parents. They connect with others who know what they’re going through. It’s a place to share stories and get advice.
Advocating for Your Child
It’s key to know how to speak up for your child. Learning about blood transfusions helps. This way, parents can talk to doctors better. They can make sure their child gets the best care.
FAQ
How is blood transfusion volume calculated in pediatric patients?
We figure out how much blood kids need based on their weight and health needs. We use special guidelines and formulas to get it right.
What factors influence the amount of blood used in transfusions for children?
The amount of blood kids get depends on their age, weight, and how sick they are.
How do blood transfusions differ between adults and children?
Blood transfusions for kids are different from those for adults. Kids need their blood volume calculated based on their weight and health. This ensures they get the right amount of blood.
What are the risks associated with blood transfusions in pediatric patients?
Blood transfusions can have risks for kids. We watch them closely to keep them safe and treat any problems quickly.
How can parents support their children undergoing blood transfusions?
Parents can help by being there for their kids. They should understand what’s happening and watch for any signs of trouble.
What is the importance of follow-up care after a blood transfusion?
After a blood transfusion, it’s key to check how the patient is doing. We look at their hemoglobin levels and watch for any lasting effects.
How do healthcare teams collaborate to ensure safe blood transfusions?
Our teams work together to make sure blood transfusions are safe. We communicate well, follow rules, and know what each patient needs.
What advances are being made in blood transfusion practices?
New advances are making blood transfusions safer and more effective. These include better matching of blood types and reducing risks of complications.
Where can parents find reliable information and support for their children undergoing blood transfusions?
We offer resources and support for parents. This includes trusted information, workshops, and support groups to help them support their child.
How is total blood volume calculated?
We calculate total blood volume using formulas that consider the patient’s weight and other factors. This helps us choose the right amount for transfusions.
What is the formula for determining blood transfusion volume?
We use formulas like weight-based calculations to figure out how much blood kids need for transfusions.
References
Centers for Disease Control and Prevention. Evidence-Based Medical Insight. Retrieved from https://www.cdc.gov/blood/diseases/transfusion/faq.html**