Last Updated on November 27, 2025 by Bilal Hasdemir

At Liv Hospital, we understand the challenges posed by endometriosis, a condition affecting an estimated 10% of reproductive-age women worldwide. This chronic condition can cause severe pain and sometimes infertility, significantly impacting the quality of life.
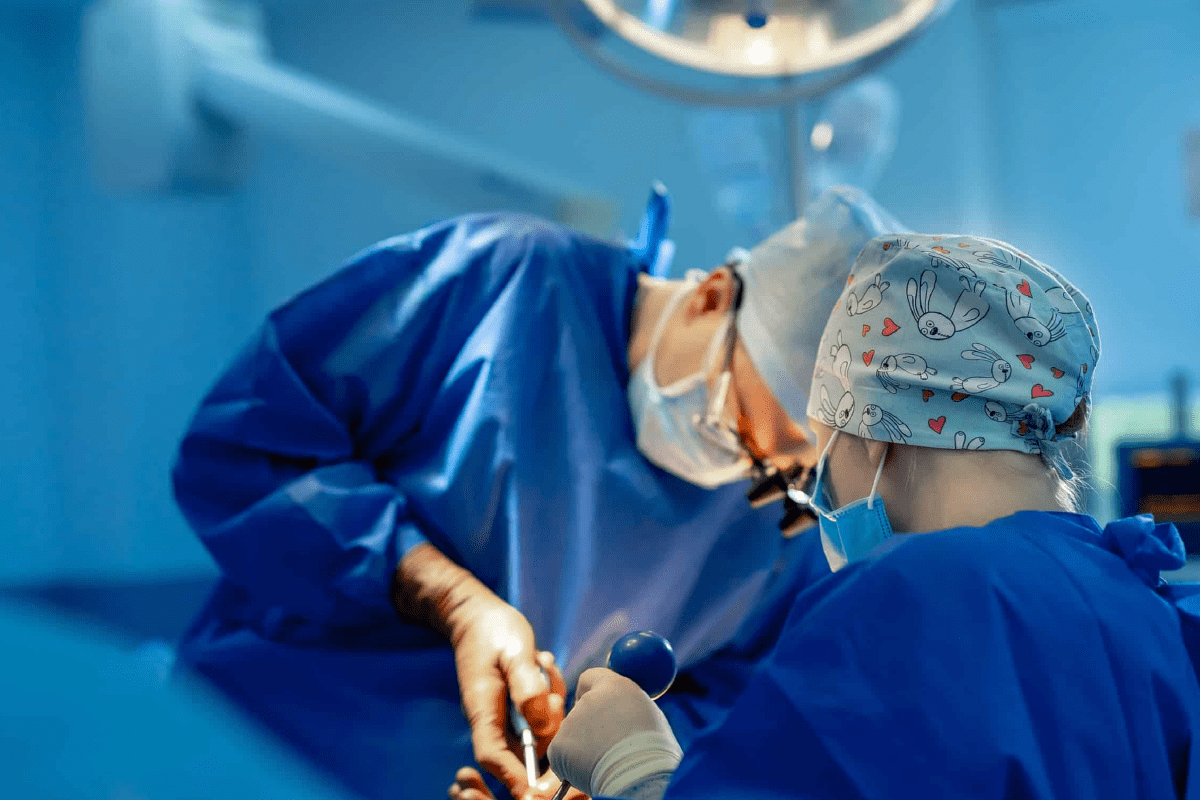
Laparoscopic surgery for endometriosis treatment is a crucial method for both diagnosing and treating this condition. As a minimally invasive surgery, it offers a faster recovery time and less scarring compared to traditional surgical methods.
We are committed to delivering advanced medical care with a focus on patient comfort and successful outcomes. Our team of experts is dedicated to providing world-class healthcare with complete support for international patients.
Key Takeaways
- Laparoscopic surgery is a gold standard for diagnosing and treating endometriosis.
- Liv Hospital provides world-class healthcare with a focus on patient comfort.
- Minimally invasive surgery offers faster recovery and less scarring.
- Endometriosis affects a significant portion of reproductive-age women worldwide.
- Our team is dedicated to delivering advanced medical care.
Understanding Endometriosis and Its Impact
Endometriosis is a complex condition that affects millions of women worldwide, causing significant discomfort and impacting their quality of life. It is a chronic and often painful condition where tissue similar to the lining inside the uterus is found outside the uterus, leading to various symptoms and complications.
What Is Endometriosis?
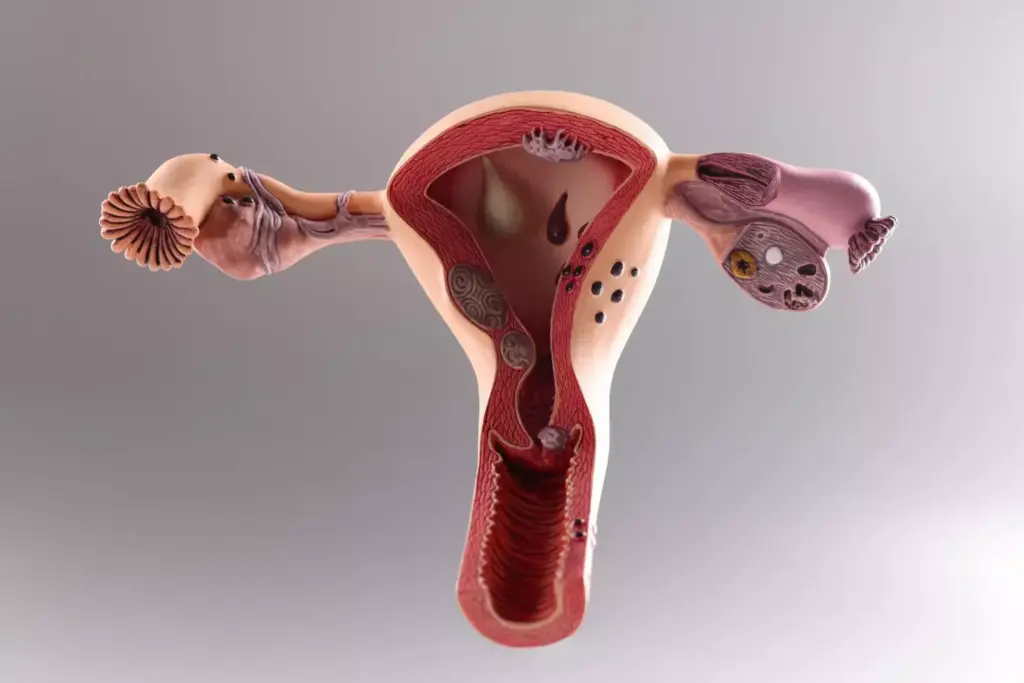
Endometriosis occurs when endometrial-like tissue grows outside the uterus, often on the ovaries, fallopian tubes, and the pelvic tissue. This misplaced tissue acts as it would inside the uterus, thickening and bleeding with each menstrual cycle, leading to inflammation, scarring, and adhesions. We know that understanding the nature of endometriosis is crucial for patients to make informed decisions about their treatment. For more detailed information on laparoscopy and endometriosis.
Common Symptoms and Complications
The symptoms of endometriosis can vary widely among women but commonly include severe pelvic pain, heavy or irregular menstrual bleeding, and infertility. Some women may also experience painful urination or bowel movements during their periods. If left untreated, endometriosis can lead to complications such as ovarian cysts, adhesions, and increased risk of infertility.
Impact on Quality of Life
Endometriosis significantly impacts a woman’s quality of life, affecting not just her physical health but also her mental well-being. Chronic pain and heavy bleeding can lead to anemia, fatigue, and depression. The condition can also affect relationships and daily activities, making it essential to manage symptoms effectively. We recognize the importance of a comprehensive approach to treating endometriosis, including pelvic pain management, to improve the overall quality of life for those affected.
Laparoscopy and Endometriosis Excision: The Gold Standard

For women suffering from endometriosis, laparoscopic excision surgery has emerged as the gold standard treatment. This minimally invasive surgical technique has revolutionized the management of endometriosis, offering a precise and effective solution for removing endometrial lesions.
We recognize the importance of understanding why laparoscopy is preferred for endometriosis treatment. The benefits of this approach are multifaceted, ranging from reduced recovery time to fewer complications.
Why Laparoscopy Is Preferred
Laparoscopy is favored for endometriosis treatment due to its minimally invasive nature, which results in less tissue damage and trauma compared to traditional open surgery. This approach leads to quicker recovery times and reduced risk of complications.
“Laparoscopic surgery has become the cornerstone in the treatment of endometriosis, providing a clear visual and therapeutic advantage.”
Excision vs. Ablation Techniques
When it comes to treating endometriosis laparoscopically, two primary techniques are employed: excision and ablation. Excision involves the surgical removal of endometrial lesions, whereas ablation focuses on destroying the lesions using heat or cold.
| Technique | Description | Advantages |
|---|---|---|
| Excision | Surgical removal of endometrial lesions | Precise removal, potentially lower recurrence rates |
| Ablation | Destruction of lesions using heat or cold | Less invasive, quicker procedure |
Benefits of Minimally Invasive Approach
The benefits of laparoscopic surgery for endometriosis are numerous. This approach not only reduces postoperative pain and recovery time but also minimizes scarring and complications. Furthermore, the precision of laparoscopy allows for a more thorough removal of endometrial lesions, potentially reducing the risk of recurrence.
By choosing laparoscopic excision, patients can benefit from a more effective and less invasive treatment option. As we continue to advance in our understanding and techniques, the management of endometriosis through laparoscopy is likely to become even more refined.
The Laparoscopic Procedure Explained
Laparoscopic surgery represents a significant advancement in the surgical management of endometriosis, offering a balance between diagnostic accuracy and therapeutic intervention. This procedure involves making small incisions in the abdomen to insert a laparoscope and specialized instruments, allowing surgeons to visualize the pelvic region and remove endometrial lesions.
Preparation and Anesthesia
Preparation for laparoscopic surgery typically involves a thorough medical evaluation, including a review of the patient’s medical history and any necessary preoperative testing. The procedure is usually performed under general anesthesia to ensure patient comfort and safety during the surgery.
Key aspects of preparation include:
- Preoperative counseling to discuss the risks and benefits of the procedure
- Instructions on preoperative care, such as fasting requirements
- Arrangements for postoperative care and support
Surgical Technique and Tools
The laparoscopic procedure for endometriosis involves the use of a laparoscope, which is a thin, lighted tube with a camera, and specialized surgical instruments. These tools enable surgeons to visualize the pelvic organs and perform precise dissections to remove endometrial implants.
The surgical technique may vary depending on the extent and location of the endometriosis. Surgeons may employ various techniques, including excision or ablation, to treat the condition effectively.
Typical Recovery Timeline
The recovery timeline following laparoscopic surgery for endometriosis can vary among individuals. Generally, patients can expect to resume normal activities within a few weeks after the procedure.
Common recovery milestones include:
- Immediate postoperative recovery, typically involving a short hospital stay or outpatient care
- Gradual return to normal activities over the course of 1-3 weeks
- Follow-up appointments to monitor healing and address any concerns
By understanding the laparoscopic procedure, patients can better prepare themselves for the surgical experience and the subsequent recovery process.
Diagnostic Laparoscopy for Endometriosis
We utilize diagnostic laparoscopy as a definitive method for diagnosing endometriosis and assessing its severity. This minimally invasive surgical procedure allows us to directly visualize the pelvic organs and identify endometrial lesions.
The Visual Confirmation Process
During diagnostic laparoscopy, a laparoscope is inserted through a small incision near the navel, providing a clear view of the pelvic cavity. This visual examination enables us to identify endometrial implants, adhesions, and other abnormalities associated with endometriosis. The visual confirmation process is crucial for determining the extent and location of the disease.
Biopsy and Tissue Analysis
In addition to visual inspection, we may perform a biopsy to collect tissue samples for further analysis. This involves removing small samples of suspected endometrial tissue for histological examination. The biopsy and tissue analysis provide a definitive diagnosis, helping us differentiate endometriosis from other conditions with similar symptoms.
Staging Endometriosis During Diagnosis
During diagnostic laparoscopy, we also stage the endometriosis based on the extent of the disease. Staging involves assessing the number, size, and location of endometrial implants, as well as the presence of adhesions and ovarian endometriomas. This information is critical for developing an effective treatment plan tailored to the patient’s specific needs.
By combining visual confirmation, biopsy, and staging, diagnostic laparoscopy provides a comprehensive understanding of endometriosis in each patient. This approach enables us to offer personalized care and improve treatment outcomes.
Treatment Options During Laparoscopic Surgery
Laparoscopic treatment of endometriosis encompasses a range of surgical options, including excision, diathermy, and ablation. The choice of treatment depends on various factors, including the extent and location of the endometriosis, as well as the patient’s overall health and surgical history.
Excision Techniques and Outcomes
Excision is a highly effective technique used during laparoscopic surgery to remove endometriotic lesions. This method involves surgically cutting out the affected tissue, ensuring that the root cause of the symptoms is addressed. The outcomes of excision are generally favorable, with many patients experiencing significant relief from symptoms.
The success of excision depends on the skill of the surgeon and the extent of the disease. Studies have shown that thorough excision can lead to improved quality of life and reduced recurrence rates.
Diathermy and Ablation Methods
Diathermy and ablation are alternative techniques used to treat endometriosis during laparoscopic surgery. Diathermy involves using electrical energy to destroy the endometriotic lesions, while ablation uses various energy sources to achieve a similar effect. These methods can be effective, especially for superficial lesions.
However, the choice between excision, diathermy, and ablation depends on the specific characteristics of the endometriosis and the patient’s condition. A comprehensive evaluation by a skilled surgeon is crucial to determine the most appropriate treatment approach.
Addressing Different Locations of Endometriosis
Endometriosis can occur in various locations within the pelvic cavity, including the ovaries, fallopian tubes, and bowel. Laparoscopic surgery allows for the treatment of endometriosis in these different locations, tailoring the approach to the specific needs of the patient.
The versatility of laparoscopic surgery means that surgeons can address complex cases involving multiple sites of endometriosis, providing comprehensive care in a single procedure.
Specialized Approaches for Complex Endometriosis
Endometriosis that involves other organs, such as the bowel or bladder, necessitates a tailored surgical strategy. At Liv Hospital, we have developed expertise in managing complex endometriosis cases, ensuring the best possible outcomes for our patients.
Laparoscopy for Bowel Endometriosis
Bowel endometriosis is a challenging condition that requires precise surgical techniques. Laparoscopic surgery offers a minimally invasive approach, allowing for the removal of endometrial lesions from the bowel without major incisions. This technique not only reduces recovery time but also minimizes the risk of complications.
We utilize advanced laparoscopic tools and techniques to dissect and remove endometriotic nodules from the bowel. The procedure is performed under general anesthesia, ensuring patient comfort throughout the surgery.
Bladder and Urinary Tract Involvement
Endometriosis affecting the bladder or urinary tract requires a multidisciplinary approach, involving both gynecological and urological expertise. Laparoscopic surgery is employed to carefully dissect and remove endometrial implants from the bladder and urinary tract, preserving organ function.
Our surgeons work closely with urologists to ensure comprehensive care for patients with urinary tract endometriosis. This collaborative approach enables us to address complex cases effectively.
Deep Infiltrating Endometriosis Management
Deep infiltrating endometriosis (DIE) is a severe form of endometriosis that penetrates deep into the tissue. Managing DIE requires advanced surgical skills and a thorough understanding of pelvic anatomy. We use laparoscopic techniques to excise DIE lesions, often involving multiple pelvic structures.
The goal of surgical management for DIE is to remove all visible endometriotic lesions while preserving surrounding healthy tissue and organ function. This approach helps in reducing symptoms and improving the quality of life for our patients.
At Liv Hospital, we are committed to providing world-class care for complex endometriosis cases. Our team of experts is dedicated to delivering personalized treatment plans, ensuring the best possible outcomes for each patient.
How Often Can Laparoscopic Surgery Be Repeated?
The need for repeat laparoscopic surgeries is a significant consideration in the treatment plan for endometriosis patients. We understand that the frequency of these procedures can vary based on several factors, including the severity of the disease, the effectiveness of the initial surgery, and individual patient characteristics.
Average Frequency in Clinical Practice
In clinical practice, the average frequency of laparoscopic surgeries for endometriosis can range from one to multiple procedures over several years. Studies have shown that some patients may require repeat surgeries within 2-5 years after the initial procedure, depending on the extent of the disease and the surgical technique used.
We have observed that the decision to perform repeat surgeries is typically based on the recurrence of symptoms and the patient’s overall health condition. It’s a complex decision that involves evaluating the risks and benefits of additional surgery.
Factors That Necessitate Repeat Surgeries
Several factors can necessitate repeat laparoscopic surgeries for endometriosis. These include:
- The severity and extent of the initial disease
- Incomplete removal of endometrial lesions during the initial surgery
- Recurrence of symptoms due to new or residual endometriotic growths
- Changes in the patient’s reproductive plans or hormonal status
Understanding these factors is crucial for managing patient expectations and developing an effective treatment plan. We work closely with our patients to monitor their condition and adjust their treatment strategy as needed.
Statistical Data on Multiple Procedures
Statistical data on the frequency of repeat laparoscopic surgeries for endometriosis provide valuable insights into the long-term management of the condition. Research indicates that up to 50% of patients may require a second surgery within 5 years of the initial procedure.
We analyze such data to refine our treatment approaches and improve patient outcomes. By understanding the patterns and predictors of repeat surgeries, we can better support our patients through their treatment journey.
Factors Determining the Need for Repeat Surgeries
Understanding the factors that necessitate repeat surgeries is crucial for effective endometriosis management. The decision to undergo repeat laparoscopic surgery is influenced by multiple critical elements.
Disease Severity and Progression Rate
The severity of endometriosis and its progression rate play significant roles in determining the need for repeat surgeries. Patients with more severe endometriosis or those whose disease progresses rapidly are more likely to require additional surgical interventions. Disease severity is often assessed through diagnostic laparoscopy, which allows surgeons to visualize the extent of endometrial implants and adhesions.
The progression rate of endometriosis can vary significantly among individuals, influenced by factors such as hormonal fluctuations and the effectiveness of previous treatments. Regular monitoring is essential to identify those at higher risk of disease progression.
Surgical Technique and Surgeon Experience
The surgical technique employed during laparoscopy and the experience of the surgeon are crucial factors that influence the need for repeat surgeries. Techniques such as excision versus ablation can impact recurrence rates, with some studies suggesting that excision may offer more durable results.
Surgeon experience is also a critical determinant, as more experienced surgeons may achieve more complete excisions, potentially reducing the need for future surgeries. The use of advanced technologies and specialized training can further enhance surgical outcomes.
Patient Age and Fertility Considerations
Patient age and fertility considerations are additional factors that influence the decision for repeat surgeries. Younger patients, particularly those with a desire for future fertility, may be more likely to undergo repeat surgeries to maximize their chances of conception.
Fertility preservation is a key consideration in the management of endometriosis, especially in younger patients. The potential impact of repeat surgeries on ovarian reserve and overall fertility must be carefully weighed against the benefits of surgical intervention.
Risks Associated with Multiple Laparoscopic Procedures
The risks associated with repeated laparoscopic procedures for endometriosis are a critical concern for both patients and healthcare providers. While laparoscopy is considered a safe and effective treatment, understanding the potential complications is essential for informed decision-making.
Formation of Adhesions
One of the significant risks associated with multiple laparoscopic surgeries is the formation of adhesions. Adhesions are bands of fibrous tissue that can form between organs or between an organ and the abdominal wall. They are a common complication of any surgical procedure, including laparoscopy. Adhesions can lead to chronic pain, bowel obstruction, and infertility, significantly impacting a patient’s quality of life.
We have observed that the risk of adhesion formation increases with the number of surgical procedures a patient undergoes. Therefore, it’s crucial to discuss the potential for adhesions with your healthcare provider and explore strategies to minimize this risk.
Potential Organ Injury and Complications
Another risk associated with multiple laparoscopic procedures is the potential for organ injury. During laparoscopy, there is a risk of damaging nearby organs such as the bowel, bladder, or ureters. The risk of organ injury is higher in patients who have undergone previous surgeries, as adhesions from previous operations can make it more challenging to navigate the surgical site.
Complications from organ injury can be severe and may require additional surgery to repair. It’s essential for patients to be aware of these risks and to discuss them with their surgeon.
Cumulative Anesthesia Exposure
Cumulative anesthesia exposure is another concern for patients undergoing multiple laparoscopic procedures. While modern anesthetics are generally safe, repeated exposure can have cumulative effects. Some studies suggest that repeated anesthesia exposure may affect cognitive function, particularly in older adults or those with certain pre-existing conditions.
We recommend that patients discuss their anesthesia options and any concerns with their anesthesiologist. This can help minimize risks associated with cumulative anesthesia exposure.
Strategies to Extend Time Between Surgeries
For many patients, the key to managing endometriosis lies in strategies that extend the time between surgical interventions. By adopting a multifaceted approach to treatment, we can potentially reduce the frequency of surgeries and improve the quality of life for those affected.
Hormonal Suppression Therapies
Hormonal suppression therapies play a crucial role in managing endometriosis by reducing the growth and activity of endometrial lesions. These therapies can include:
- Gonadotropin-releasing hormone (GnRH) agonists: These medications create a menopausal state, reducing estrogen production and thereby decreasing the growth of endometrial tissue.
- Progestin-only therapies: Progestins can help in reducing the symptoms of endometriosis by thinning the endometrial lining and preventing the growth of new lesions.
- Combined hormonal contraceptives: Birth control pills, patches, or rings can help manage symptoms by regulating hormonal fluctuations.
As noted by doctor “Hormonal therapies are a cornerstone in the management of endometriosis, offering symptom relief and potentially delaying the need for further surgical intervention.”
“The use of hormonal therapies can significantly impact the quality of life for patients with endometriosis.”
Comprehensive Pain Management
Effective pain management is essential for improving the quality of life for patients with endometriosis. This can involve a combination of:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These are often used as a first-line treatment for pain relief.
- Nerve pain medications: Medications like gabapentin can be effective for managing neuropathic pain associated with endometriosis.
- Hormonal treatments: As mentioned earlier, hormonal therapies can also contribute to pain reduction.
Comprehensive pain management strategies can help alleviate symptoms, making it easier for patients to manage their condition between surgeries.
Integrative and Lifestyle Approaches
In addition to medical therapies, integrative and lifestyle approaches can play a significant role in managing endometriosis. These may include:
- Dietary changes: Certain diets, such as those low in processed foods and high in omega-3 fatty acids, may help reduce symptoms.
- Physical therapy: Pelvic physical therapy can help alleviate pain and improve pelvic floor function.
- Stress management techniques: Practices like mindfulness, yoga, and meditation can help reduce stress, which is known to exacerbate endometriosis symptoms.
By incorporating these strategies into their treatment plan, patients can potentially extend the time between surgeries and improve their overall well-being.
Advanced Techniques That May Reduce Recurrence Rates
The latest advancements in surgical technology are offering new hope for reducing endometriosis recurrence rates. As we continue to explore innovative approaches, several advanced techniques have emerged that show promise in improving patient outcomes.
Robotic-Assisted Laparoscopy
Robotic-assisted laparoscopy represents a significant advancement in the field of minimally invasive surgery. This technique offers enhanced precision, flexibility, and control, allowing surgeons to perform complex procedures with greater ease. Studies have shown that robotic-assisted laparoscopy can lead to reduced recovery times and fewer complications.
Specialized Imaging Technologies
Specialized imaging technologies, such as high-definition laparoscopy and fluorescence imaging, are being increasingly used to improve surgical outcomes. These technologies provide surgeons with real-time, detailed visuals, enabling more accurate identification and removal of endometrial lesions.
| Imaging Technology | Benefits |
|---|---|
| High-Definition Laparoscopy | Enhanced visualization of endometrial lesions |
| Fluorescence Imaging | Real-time identification of lesions |
Emerging Surgical Innovations
Emerging surgical innovations, including the use of nanotechnology and advanced energy devices, are being explored for their potential to reduce endometriosis recurrence rates. These cutting-edge technologies aim to provide more precise and effective treatments, ultimately improving patient quality of life.
- Nanotechnology for targeted therapy
- Advanced energy devices for precise lesion removal
By embracing these advanced techniques, we can potentially reduce the need for repeat surgeries and improve long-term outcomes for patients with endometriosis.
Conclusion
Effective management of endometriosis through laparoscopy and endometriosis excision is crucial for improving the quality of life for women affected by this condition. At Liv Hospital, we have highlighted the importance of minimally invasive surgery in diagnosing and treating endometriosis, emphasizing the benefits of laparoscopic procedures.
Our discussion has underscored the complexities of endometriosis treatment and the need for personalized care. With ongoing advancements in women’s health surgery, we are committed to delivering world-class healthcare that addresses the unique needs of our patients. By leveraging the latest techniques in laparoscopy and endometriosis excision, we aim to provide successful outcomes and comprehensive support.
At Liv Hospital, our commitment to providing exceptional care is unwavering. We strive to make a positive impact on the lives of women affected by endometriosis, ensuring they receive the highest standard of treatment and compassion. Through our dedication to advancing endometriosis treatment and women’s health surgery, we continue to push the boundaries of what is possible in minimally invasive surgery.
FAQ
What is endometriosis and how is it diagnosed?
Endometriosis is a chronic condition where tissue similar to the lining of the uterus grows outside the uterus, causing pain and discomfort. It is diagnosed through a combination of medical history, physical examination, imaging tests, and laparoscopy, which allows for visual confirmation and biopsy.
Why is laparoscopy preferred for treating endometriosis?
Laparoscopy is preferred because it is a minimally invasive procedure that allows for precise removal of endometrial lesions, reducing recovery time and complications. It also enables surgeons to visualize the extent of the disease and perform excision or ablation as needed.
What is the difference between excision and ablation techniques in laparoscopic surgery for endometriosis?
Excision involves surgically removing the endometrial lesions, while ablation involves destroying the lesions using heat or cold. Excision is often considered more effective, as it allows for complete removal of the affected tissue.
How often can laparoscopic surgery be repeated for endometriosis?
The frequency of repeat laparoscopic surgeries depends on various factors, including disease severity, surgical technique, and patient age and fertility considerations. On average, some patients may require repeat surgeries every few years, while others may not need additional procedures.
What are the risks associated with multiple laparoscopic procedures?
Risks include the formation of adhesions, potential organ injury, and cumulative anesthesia exposure. However, these risks can be minimized by choosing an experienced surgeon and following proper post-operative care.
Can hormonal suppression therapies help extend the time between surgeries?
Yes, hormonal suppression therapies can help manage symptoms and slow disease progression, potentially extending the time between surgeries. These therapies can be used in conjunction with other treatments, such as pain management and lifestyle modifications.
What are some advanced techniques that may reduce recurrence rates?
Techniques such as robotic-assisted laparoscopy, specialized imaging technologies, and emerging surgical innovations may improve patient outcomes and reduce recurrence rates. These advancements are continually being developed and refined to provide better care for patients with endometriosis.
How can I prepare for laparoscopic surgery for endometriosis?
Preparation involves following the surgeon’s instructions, which may include dietary changes, stopping certain medications, and arranging for post-operative care. It’s also essential to discuss any concerns or questions with your healthcare provider.
What can I expect during the recovery period after laparoscopic surgery?
The recovery period typically involves some discomfort, which can be managed with pain medication. Most patients can return to normal activities within a few weeks. It’s essential to follow the surgeon’s instructions for post-operative care to ensure a smooth recovery.