Last Updated on November 26, 2025 by Bilal Hasdemir
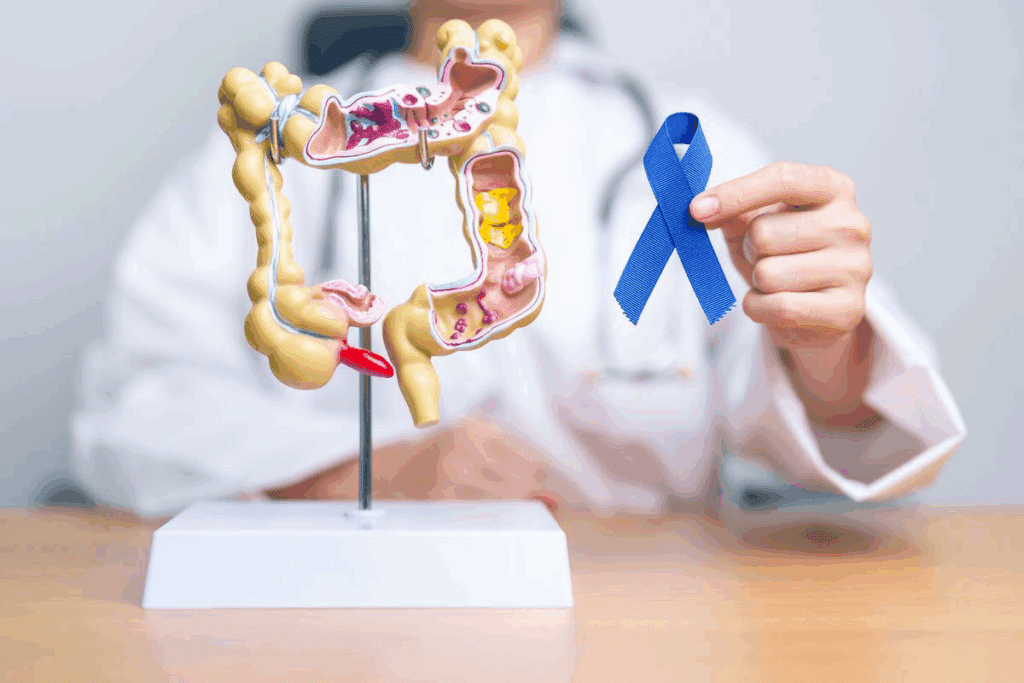
Learn how often should you get a colonoscopy based on age, risk, and medical recommendations.
How often you need a colonoscopy varies. It depends on your age, family history, and past colonoscopy results. The US Preventive Services Task Force suggests screening for adults aged 45 to 75.
At Liv Hospital, we focus on your safety and the latest care for your colon health. Knowing when to get a colonoscopy is vital for stopping colorectal cancer.
Key Takeaways
- Colonoscopy is a critical tool in preventing colorectal cancer.
- The frequency of colonoscopy depends on individual risk factors.
- Guidelines recommend starting screenings at age 45.
- Liv Hospital prioritizes patient safety and up-to-date care.
- Regular screenings can significantly improve colorectal health outcomes.
The Critical Role of Colonoscopy in Colorectal Cancer Prevention
Colonoscopy is a key tool in the battle against colorectal cancer. It’s a screening method that finds cancer early and stops it by removing polyps before they turn cancerous.
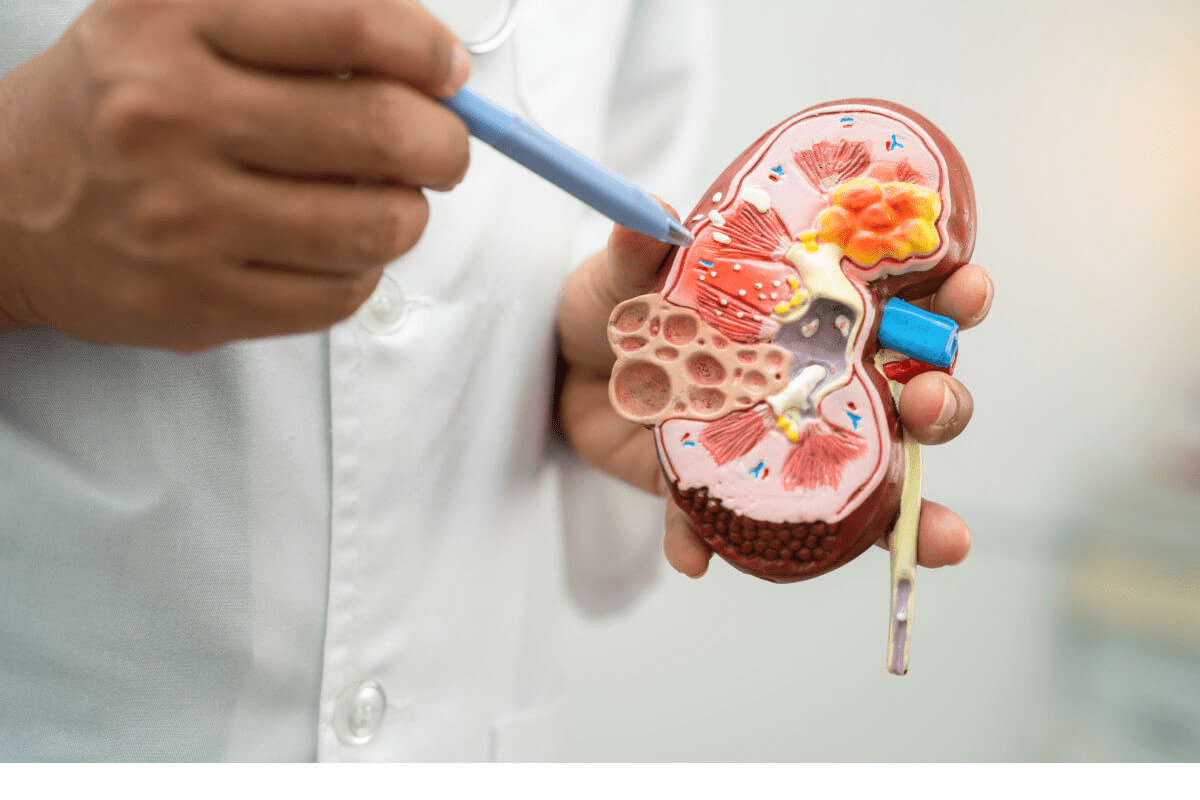
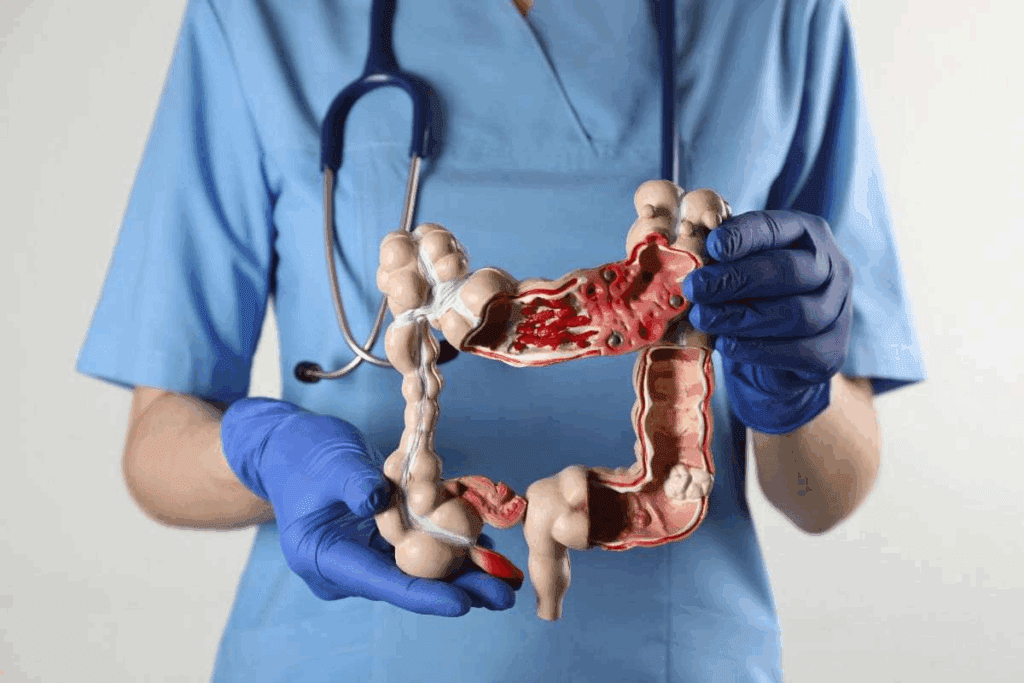
What Happens During a Colonoscopy Procedure
A gastroenterologist uses a flexible tube with a camera and light to look inside the colon and rectum. This lets them see the whole colon. They can spot polyps, cancer, and other issues.
The doctor can take out polyps and get biopsies if needed. The whole thing is done under sedation to make it as comfortable as possible.
How Colonoscopies Detect and Prevent Cancer
Colonoscopy finds cancer by looking directly at the colon. It stops cancer by taking out polyps that could turn into cancer later.
Research shows colonoscopy cuts down on colorectal cancer cases. By removing polyps before they turn cancerous, it’s a big help in preventing cancer.
Effectiveness of Colonoscopy in Reducing Cancer Mortality
Colonoscopy is proven to lower death rates from colorectal cancer. It finds cancer early and removes polyps, which helps a lot.
Getting regular screenings is important to get the most benefits. People with a family history or other risk factors might need to go more often.
How Often Should You Get a Colonoscopy: Current Medical Guidelines
Medical guidelines help figure out how often you should get a colonoscopy. These rules are based on the latest science and expert opinions. They aim to prevent colorectal cancer effectively.
American Cancer Society Recommendations
The American Cancer Society says adults should start screening at 45 if they’re at average risk. If you have a family history or other risk factors, you might need to start earlier. For those at average risk, colonoscopies should be done every 10 years.
U.S. Preventive Services Task Force Guidelines
The U.S. Preventive Services Task Force (USPSTF) also suggests starting screening at 45. They recommend different screening methods, including colonoscopy. They stress the need for screening between 45 and 75 years old.
Recent Changes in Screening Age Recommendations
Guidelines have recently changed, lowering the starting age for screening from 50 to 45. This change is due to more cases of colorectal cancer in younger people.
Comparing Guidelines Across Medical Organizations
While most agree on starting screening at 45, there are some differences. The table below shows the main guidelines:
| Organization | Starting Age | Recommended Interval |
| American Cancer Society | 45 | 10 years |
| U.S. Preventive Services Task Force | 45 | Various options, including every 10 years for colonoscopy |
| Multi-Society Task Force | 45 | 10 years for colonoscopy |
Key Takeaway: Most major medical groups say start screening at 45. For those at average risk, a colonoscopy every 10 years is recommended.
Average Risk Individuals: Understanding the 10-Year Interval
Experts say people at average risk should get a colonoscopy every 10 years. This helps prevent colorectal cancer. It’s based on lots of research and knowing how colorectal cancer grows.
Defining “Average Risk” Criteria
People at average risk have no history of colorectal cancer or polyps. They also don’t have a family history of colorectal cancer. And they shouldn’t have inflammatory bowel disease.
Key factors that determine average risk include:
- No personal history of colorectal cancer
- No family history of colorectal cancer
- No known genetic syndromes like Lynch syndrome or Familial Adenomatous Polyposis (FAP)
- No history of adenomatous polyps
- No inflammatory bowel disease
Scientific Evidence Supporting the 10-Year Screening Interval
Many studies show that the risk of colorectal cancer is low after 10 years of a normal colonoscopy. This supports the 10-year screening rule for average-risk people.
The 10-year rule works because most colorectal cancers grow slowly from polyps. It takes about 10 years for a polyp to turn into cancer. This gives enough time for early detection and removal.
What Makes the Decade Rule Effective for Most People
The 10-year rule is effective because it balances early detection benefits with procedure risks. For most average-risk people, the benefits of colonoscopy in preventing cancer are greater than the risks.
| Risk Category | Recommended Screening Interval | Rationale |
| Average Risk | 10 years | Slow growth of most colorectal cancers allows for effective screening within this timeframe. |
| High Risk | More frequent than 10 years | Increased risk factors necessitate more frequent monitoring. |
Knowing what makes you at average risk and the evidence for the 10-year rule helps you make smart choices about screening for colorectal cancer.
High-Risk Individuals: When More Frequent Screening Is Necessary
Some people need to get colonoscopies more often because of certain risk factors. This is to catch and prevent colorectal cancer early.
Family History of Colorectal Cancer or Polyps
Having a family history of colorectal cancer or polyps means you need to watch your health closely. If a first-degree relative (like a parent or sibling) had it, you’re at higher risk.
Key Considerations:
- Age of diagnosis of the relative
- Number of affected relatives
- Degree of relationship
Personal History of Adenomatous Polyps
Having had adenomatous polyps before raises your risk of colorectal cancer. The size, number, and type of polyps help decide how often you should get screened.
Inflammatory Bowel Disease (Crohn’s and Ulcerative Colitis)
People with inflammatory bowel disease (IBD) like Crohn’s or ulcerative colitis face a higher risk of colorectal cancer. How long and how widespread the disease is matters a lot.
Surveillance Strategy: Regular colonoscopies with many biopsies are advised for those with long-standing IBD.
Genetic Syndromes (Lynch Syndrome, FAP)
Genetic conditions like Lynch syndrome and Familial Adenomatous Polyposis (FAP) greatly increase your risk of colorectal cancer. These people need special screening plans.
| Genetic Syndrome | Screening Recommendations |
| Lynch Syndrome | Annual colonoscopy starting at age 20-25 |
| FAP | Annual sigmoidoscopy or colonoscopy starting at age 10-12 |
Knowing about these risk factors helps set the right screening schedule for high-risk people. This way, doctors can better prevent and catch colorectal cancer early.
Colonoscopy Frequency After Polyp Removal
After a colonoscopy, how often you need another one depends on what was found. This includes if polyps were found and removed. The type, number, and size of these polyps are key in setting the follow-up schedule.
Types of Polyps and Their Cancer Risk
Polyps are growths inside the colon or rectum. Most are not cancerous. But, some types, like adenomatous polyps, can turn cancerous over time. The risk of cancer depends on the polyp’s type, size, and if it has dysplasia.
Adenomatous polyps are common and can be precancerous. The bigger the polyp, the higher the risk of it turning into cancer.
Follow-up Schedules Based on Number and Size of Polyps
The number and size of polyps removed are important for setting the next screening’s timing. People with many or large polyps usually need more frequent checks.
| Number and Size of Polyps | Recommended Follow-Up |
| 1-2 small polyps ( | 5-10 years |
| 3-10 adenomatous polyps or 1 polyp >1 cm | 3 years |
| More than 10 polyps | Less than 3 years, consider 1 year |
The 3-5 Year Rule for Post-Polypectomy Surveillance
People with adenomatous polyps often need a follow-up colonoscopy in 3 to 5 years. This is based on the polyps’ risk assessment.
The exact timing within this range depends on the specifics of the polyps and the patient’s overall risk profile.
When to Return to Normal Screening Intervals
If follow-up colonoscopies show no new polyps or only small, benign ones, the screening interval can be extended to 10 years. This decision is made based on the patient’s history and risk factors.
Knowing what affects how often you need a colonoscopy after polyp removal is key to preventing colorectal cancer. By following the recommended schedule, you can greatly lower your risk of colorectal cancer.
Age-Specific Recommendations for Colonoscopy Screening
The age of 45 marks a key time for starting colorectal cancer screening. This advice comes from top medical groups. They stress the need for early detection to lower cancer risk.
First-Time Screening at Age 45: The New Standard
Most people should start screening for colorectal cancer right after turning 45. This change is based on studies showing early screening improves cancer prevention. The American Cancer Society and others say those at average risk should start screening at 45.
Screening Protocols for Ages 45-75
People aged 45 to 75 should get colonoscopies every 10 years if they’re at average risk. This helps catch and remove polyps before they turn cancerous. It greatly lowers the risk of colorectal cancer.
Screening frequency might change based on past colonoscopy results. For example, if polyps are found, a follow-up might be needed sooner than 10 years.
Special Considerations for Adults Over 75
For those over 75, screening decisions depend on health and past screenings. Health status, life expectancy, and past results are key in deciding if screening is beneficial.
Guidelines say stop screening if life expectancy is short or if past screenings have been negative.
When to Stop Colonoscopy Screening
Stopping colonoscopy screening is a personal choice. It’s usually advised to stop when the risks of the procedure are greater than the benefits. This often applies to older adults or those with serious health issues.
Doctors look at health status, screening history, and personal wishes when deciding to stop screening.
How Long Is a Colonoscopy “Good For”? Understanding Protection Periods
Knowing how long a colonoscopy protects you is key to preventing colorectal cancer. For most, it’s up to 10 years. But, if you’re at higher risk, you might need to go back sooner.
The Science Behind the 10-Year Protection Period
Science backs the 10-year protection period after a colonoscopy. Studies show it works for people at average risk. This time frame is based on how colorectal cancer grows over years.
Key factors supporting the 10-year interval include:
- The slow growth rate of most colorectal polyps
- The high sensitivity of modern colonoscopy in detecting and removing precancerous lesions
- Epidemiological data showing a significant reduction in colorectal cancer incidence following colonoscopy
Factors That May Shorten Your Screening Interval
While the usual time between screenings is 10 years, some factors might make you need to go more often. These include:
- A family history of colorectal cancer or polyps
- A personal history of adenomatous polyps, if they were large or numerous
- Presence of inflammatory bowel disease (Crohn’s disease or ulcerative colitis)
- Known genetic syndromes such as Lynch syndrome or Familial Adenomatous Polyposis (FAP)
Warning Signs That Warrant Earlier Screening
Even with a normal colonoscopy, some symptoms might mean you need to screen sooner. Look out for:
- Rectal bleeding or blood in the stool
- Changes in bowel habits
- Unexplained abdominal pain
- Iron deficiency anemia
Balancing Cancer Prevention with Procedure Risks
Colonoscopy is great for preventing cancer, but it’s not risk-free. It can cause bleeding, perforation, and reactions to sedation. So, the choice of when to screen depends on weighing these risks against the benefits.
| Risk Category | Recommended Screening Interval | Rationale |
| Average Risk | 10 years | Standard interval based on natural history of colorectal cancer |
| High Risk (Family History, Genetic Syndromes) | Shorter interval (3-5 years) | Increased risk necessitates more frequent surveillance |
| Post-Polypectomy | 3-5 years (depending on polyp characteristics) | Risk of recurrence or missed lesions |
By understanding these factors and balancing the benefits and risks, healthcare providers can tailor colonoscopy screening intervals to individual patient needs. This maximizes the effectiveness of colorectal cancer prevention strategies.
Alternative Colorectal Cancer Screening Methods and Their Frequencies
Colonoscopy is a top choice for screening, but other options exist. These alternatives vary in convenience, accuracy, and how invasive they are. They cater to different needs and preferences.
Stool-Based Tests
Stool tests like FIT, gFOBT, and FIT-DNA are non-invasive. FIT looks for hemoglobin in stool and is done yearly. gFOBT finds blood in stool but needs more samples and diet changes. FIT-DNA tests, like Cologuard, find genetic changes in stool cells every three years.
Flexible Sigmoidoscopy
Flexible sigmoidoscopy uses a camera tube in the rectum to see the lower colon. It’s suggested every 5-10 years, often with FIT. It’s quicker and needs less prep than colonoscopy.
CT Colonography
CT colonography, or virtual colonoscopy, uses CT scans to see the colon. It’s advised every 5 years for those at average risk. It doesn’t remove polyps but technology has made it more accurate.
Comparing Effectiveness, Intervals, and Limitations
Each method has its own benefits and drawbacks. Colonoscopy is the best because it can find and remove polyps at once. Stool tests are easy but might need more tests and colonoscopies if they show something. Flexible sigmoidoscopy looks at the lower colon, and CT colonography uses radiation.
| Screening Method | Recommended Interval | Key Features |
| FIT | Annually | Non-invasive, detects hemoglobin |
| Flexible Sigmoidoscopy | Every 5-10 years | Examines lower colon, quicker than colonoscopy |
| CT Colonography | Every 5 years | Detailed images, no polyp removal |
Knowing about these screening options helps people make better choices. It’s key to talk to a doctor about your risk, preferences, and any worries. This way, you can pick the best screening plan for you.
Creating Your Personalized Colonoscopy Schedule
Creating a personalized colonoscopy schedule is key for your health. It takes into account your risk factors, screening history, and health status.
Essential Questions to Discuss with Your Doctor
Talking to your doctor is vital for a good colonoscopy schedule. You should ask:
- What are my risk factors for colorectal cancer?
- How does my family history impact my screening schedule?
- What is the recommended screening interval based on my health profile?
- Are there any alternative screening methods that might be more suitable for me?
Tracking Your Screening History
Keeping a record of your screenings is important. It helps your doctor decide when you need another colonoscopy. Tracking this info ensures your screenings are on schedule.
| Date of Colonoscopy | Findings | Polyps Removed | Next Screening Due |
| 2022-01-01 | No polyps | None | 2032-01-01 |
| 2032-01-01 | Hyperplastic polyps | 2 | 2037-01-01 |
Insurance Coverage and Accessibility Considerations
Knowing your insurance is important for planning your colonoscopy. Insurance can affect how often you get screened. Also, think about where you can get screened and who can help you.
Preparing for Your Next Colonoscopy
Getting ready for your colonoscopy is important. You’ll need to change your diet, prepare your bowels, and have someone with you. Your doctor will give you specific instructions.
By thinking about these things and talking to your doctor, you can make a personalized colonoscopy schedule. This schedule will help keep your colorectal health in top shape.
Conclusion: Prioritizing Prevention Through Appropriate Screening Intervals
It’s vital to focus on prevention by choosing the right screening times. Regular colonoscopies can spot cancers and polyps early. This helps lower the risk of colorectal cancer.
Knowing when to have a colonoscopy is key. People with average risk should get screened every 10 years. Those at higher risk might need to go more often. Starting at 45, following screening guidelines is important.
By following medical advice, you can make a colonoscopy plan that fits you. This proactive step can greatly reduce your risk of colorectal cancer.
FAQ
How often should I get a colonoscopy if I’m at average risk for colorectal cancer?
If you’re at average risk, you should get a colonoscopy every 10 years. This starts when you turn 45.
What factors classify someone as high-risk for colorectal cancer, requiring more frequent colonoscopy screenings?
Being at high risk means having a family history of colorectal cancer or polyps. It also includes a personal history of certain polyps, inflammatory bowel disease, and genetic syndromes like Lynch Syndrome and FAP.
How does the type, number, and size of polyps removed during a colonoscopy affect the frequency of subsequent screenings?
The type, number, and size of polyps removed affect how often you’ll need another colonoscopy. For example, if you have high-risk polyps, you might need a follow-up in just 3 years.
At what age should I start getting colonoscopies, and when can I stop?
You should start getting colonoscopies at 45. For those between 45 and 75, screenings are recommended every 10 years. Over 75, the decision to keep screening depends on your health.
Are there alternative colorectal cancer screening methods beside colonoscopy, and how often should they be done?
Yes, there are alternatives like stool tests, flexible sigmoidoscopy, and CT colonography. The time between these tests varies, like annually for stool tests or every 5 years for sigmoidoscopy.
How can I create a personalized colonoscopy schedule?
To make a schedule that’s right for you, talk to your doctor about your risk factors and health. Keep track of your screenings and understand your insurance.
What are the warning signs that warrant earlier colonoscopy screening?
Signs that might mean you need an earlier screening include rectal bleeding, changes in bowel habits, or a family history of colorectal cancer.
How long is a colonoscopy considered “good for” in terms of protection against colorectal cancer?
For those at average risk, a colonoscopy protects you for 10 years. But, this can change based on your health and any high-risk polyps found.
How often can I get a colonoscopy?
How often you get a colonoscopy depends on your risk and past results. While most people can wait 10 years, those at higher risk might need more frequent tests.
What are the current medical guidelines for colonoscopy screening?
Groups like the American Cancer Society and the U.S. Preventive Services Task Force set guidelines. They suggest starting screenings at 45 for those at average risk.
References
Huttinger, R. (2023). Spigelian hernia. In StatPearls. National Library of Medicine. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK538290/