Last Updated on November 27, 2025 by Bilal Hasdemir

Radiation therapy is a common treatment for cancer. It uses high-energy radiation to damage cancer cells and stop them from growing. Many patients wonder, how soon after radiation can you have a CT scan, as timing can depend on the type and area of treatment.
After radiation therapy, patients need follow-up imaging. This helps check if the treatment worked well.
A CT scan is often used for this purpose. It’s usually safe to have a CT scan after radiation. But, when it’s needed, scans can happen right away.
Knowing when and how to have a CT scan after radiation is key. Liv Hospital uses the latest methods. They make sure radiotherapy is safe and effective for patients.
Key Takeaways
- CT scans after radiation therapy are generally safe when medically necessary.
- The timing of a CT scan depends on the clinical need and treatment plan.
- Liv Hospital prioritizes patient comfort and delivers world-class outcomes.
- Radiation therapy uses high-energy radiation to treat cancer.
- Follow-up imaging is key to see if treatment worked.
Understanding Radiation Therapy and Imaging

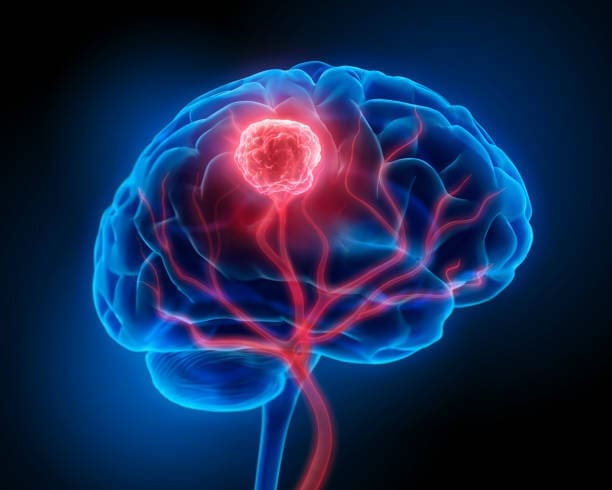
Radiation therapy is a key part of cancer treatment. It uses high-energy particles or waves to kill or harm cancer cells. This method is important in fighting cancer, aiming to destroy cancer cells while protecting healthy tissue.
The Role of Radiation in Cancer Treatment
Radiation therapy damages cancer cells’ DNA, stopping them from growing and multiplying. It uses ionizing radiation, which is focused on the tumor. The goal is to give enough radiation to kill the tumor without harming nearby healthy tissues.
Radiation therapy is proven to be effective in treating cancer. It can be used alone or with other treatments like surgery and chemotherapy. Imaging technologies are key in planning and delivering radiation therapy, making it precise and effective.
Types of Imaging Used in Conjunction with Radiation
Several imaging methods are used with radiation therapy to target tumors accurately. These include CT scans, MRI, and PET scans. Each type gives important information for planning radiation treatment. For example, CT scans are often used because they show the tumor’s size, shape, and location in detail.
Using these imaging methods with radiation therapy has greatly improved treatment results. They help make radiation delivery more precise. This means the tumor gets the right amount of radiation, while healthy tissue is protected.
How Soon After Radiation Can You Have a CT Scan?

Deciding when to have a CT scan after radiation therapy is important. It depends on the scan’s purpose and the patient’s treatment plan.
“The need for a CT scan after radiation therapy is determined on a case-by-case basis,” says a radiation oncologist. “It’s important to balance the need for timely imaging with the risks and benefits.”
Immediate Scans for Medical Necessity
In some cases, a CT scan is needed right after radiation therapy. This is true for treatments aimed at easing symptoms or pain. For example, if a patient has severe side effects, a CT scan can help doctors adjust the treatment.
Timing for Monitoring Treatment Response
For treatments aimed at curing cancer, CT scans are scheduled weeks after radiation therapy. This lets doctors see how well the treatment is working. The timing depends on the cancer type, treatment, and patient response.
As the American Cancer Society notes, “imaging tests like CT scans are used to check treatment success and look for cancer recurrence.”
Factors Affecting Scan Scheduling
Many things can affect when a CT scan is scheduled after radiation therapy. These include the patient’s health, cancer stage and type, and treatment goals. Doctors must consider these when deciding on the best time for a scan.
Understanding these factors can help patients prepare for their radiation and imaging tests. This knowledge can reduce anxiety and ensure timely care.
The Science Behind Radiation Therapy
It’s important to know how radiation therapy works in fighting cancer. This treatment uses high-energy particles or waves to kill cancer cells. It damages the DNA of these cells, stopping them from growing and multiplying.
How Radiation Damages Cancer Cell DNA
Radiation therapy harms the DNA of cancer cells, stopping them from dividing. This damage can cause the cell to die or stop growing. It’s key in controlling tumor growth.
There are two ways radiation damages DNA: direct and indirect. Direct damage happens when radiation hits DNA straight on. Indirect damage comes from radiation ionizing water molecules, which then damage DNA with free radicals.
Targeting Mechanisms and Precision
Advanced imaging and planning are key to precise radiation therapy. 3D conformal radiation therapy, Intensity-Modulated Radiation Therapy (IMRT), and Stereotactic Body Radiation Therapy (SBRT) help target tumors accurately. This reduces harm to healthy tissues.
Radiation’s Effect on Healthy Tissue
Radiation therapy aims at cancer cells but can also hit healthy tissues. The impact varies based on several factors. Treatment plans are designed to protect healthy areas.
Side effects like fatigue and skin changes are common but usually temporary. Understanding radiation therapy helps patients through their treatment. New technologies make it safer and more effective against cancer.
The Radiation Treatment Planning Process
Radiation treatment planning is a detailed process. It makes sure cancer treatment is precise and effective. This is key to getting the most from radiation therapy while protecting healthy tissues.
Initial Consultation and Assessment
The first step is an initial consultation with the patient and the radiation oncologist. They talk about the patient’s health, medical history, and what the therapy aims to achieve. This meeting is important for understanding the patient’s needs and finding the best treatment.
The next step is a thorough check of the patient’s condition. This includes the type and stage of cancer. It helps decide if radiation therapy is right and how it should be given.
CT Simulation and Mapping
CT simulation is a key part of planning. The patient has a CT scan in the treatment position. This creates a detailed map of the tumor and the area around it.
The CT simulation makes sure the patient is in the right position for treatment. Markers or tattoos might be used to guide the radiation beams.
Treatment Plan Development
After the CT simulation, a team works together to create the treatment plan. This plan includes the total radiation dose, how many sessions, and the treatment technique.
| Component | Description | Importance |
| Initial Consultation | Assessment of patient’s health and medical history | Determines suitability for radiation therapy |
| CT Simulation | Detailed imaging of tumor and surrounding anatomy | Essential for precise treatment planning |
| Treatment Plan Development | Collaboration to outline radiation dose and delivery technique | Ensures effective and safe treatment |
The treatment plan is made just for the patient. It considers the cancer type and stage, the patient’s health, and any past treatments. The goal is to target the tumor closely while protecting healthy areas.
Integration of Diagnostic Scans in Treatment Planning
Diagnostic scans are key in radiotherapy treatment planning. They help make treatment plans more precise. CT scans, in particular, give detailed images that are vital for planning.
When planning treatment, a big question is whether to use old CT scans or get new ones. Using existing CT scans is good when they are recent and relevant to the treatment area.
Using Existing CT Scans vs. New Simulations
Old CT scans are useful if they are of high quality and show the patient’s current anatomy well. This is very helpful in palliative care, where quick treatment is important.
But, new simulations are needed if the old scans are outdated, low quality, or don’t match the treatment area. The choice depends on the patient’s health and the treatment plan’s needs.
Time-Saving Benefits in Treatment Preparation
Using old diagnostic scans saves a lot of time in treatment preparation. Studies show that using prior scans can cut preparation time for palliative treatments from hours to under 30 minutes.
| Aspect | Using Existing CT Scans | Conducting New Simulations |
| Time Required | Under 30 minutes | Several hours |
| Quality of Scan | Dependent on existing scan quality | High-quality, up-to-date scans |
| Applicability | Palliative care, stable conditions | Complex cases, curative treatments |
In conclusion, using diagnostic scans in treatment planning is complex. It’s about finding the right balance between accurate imaging and quick treatment start. By using old CT scans when it makes sense, doctors can make treatment planning faster. This improves patient care.
What to Expect During Radiation Mapping and Treatment
Learning about radiation mapping and treatment can ease worries and get patients ready. Radiation therapy is a detailed process with steps like mapping, planning, and treatment delivery.
The Mapping Appointment Experience
The mapping appointment, or simulation, is key in radiation therapy. Here, patients get a CT scan to pinpoint the tumor and plan treatment. This usually takes 45 minutes to an hour.
The CT scan makes a detailed map of the area to be treated. Patients might need to stay very quiet during the scan. Sometimes, they use a special device to keep them steady for accuracy.
Duration of Radiation Planning Sessions
How long planning sessions last depends on the treatment’s complexity. They can range from 30 minutes to several hours. The team works together to create a plan tailored to the patient’s needs.
- The radiation oncologist defines the treatment target and the areas around it.
- The medical physicist figures out the best radiation dose and how to arrange the beams.
- The radiation therapist operates the machine to give the treatment.
The Actual Treatment Experience
The actual treatment is painless and quick, lasting just a few minutes. Patients lie on a table, and the therapist delivers the radiation as planned. Though painless, patients might feel tired or have skin issues, depending on the area and dose.
Knowing what to expect during radiation mapping and treatment helps patients feel more prepared and confident in their care team.
Differences Between Palliative and Curative Radiation Approaches
It’s important to know the difference between palliative and curative radiation. Radiation therapy is a key part of cancer treatment. It has different goals based on the patient’s condition and the cancer type.
Palliative Treatment Goals and Timelines
Palliative radiation helps patients with advanced cancer feel better. It aims to ease pain and other symptoms. “Palliative care is about giving patients a better life, not necessarily a longer life,” say doctors.
The treatment is shorter. It’s designed to be quick to help patients feel relief.
Curative Treatment Protocols
Curative radiation tries to get rid of the cancer or extend life. It involves longer treatment and might include other treatments like chemo or surgery. The plan is made just for the patient, based on the cancer’s type, stage, and location.
“Curative radiation is a testament to the advancements in oncology, giving hope to patients,” says a leading oncologist.
How Imaging Needs Differ Between Approaches
Imaging needs change between palliative and curative radiation. For palliative, quick CT scans are used to start treatment fast. For curative, detailed scans like CT, PET, and MRI are needed. These scans help make a detailed treatment plan.
In summary, understanding the difference between palliative and curative radiation is key. Palliative focuses on symptom relief, while curative aims to cure the cancer. Each has its own timeline and imaging needs.
Preparing for CT Scans and Radiation Treatment
Being ready for CT scans and radiation treatment is key to a good outcome. It’s important to know what steps to take before these procedures.
Physical Preparation Guidelines
Getting ready physically is essential. You might need to fast or avoid certain foods and drinks. Your doctor will tell you what to do.
Wear comfy clothes and no jewelry or metal. This helps the scan or treatment go smoothly.
Follow any medicine and drink advice. Your team will guide you to keep you safe and the treatment effective.
Key Physical Preparation Steps:
- Follow dietary restrictions as advised
- Wear comfortable, loose clothing
- Avoid jewelry or metal objects
- Follow medication and hydration instructions
Mental and Emotional Preparation
Getting ready mentally and emotionally is just as important. Knowing what to expect can reduce anxiety. Your healthcare team can help a lot.
“The more you know about your treatment, the less intimidating it becomes.” –
A cancer patient
Try relaxation techniques like deep breathing or meditation. They can help with stress and anxiety.
Questions to Ask Your Healthcare Team
Make a list of questions for your healthcare team. Ask about the treatment, side effects, and recovery.
| Category | Sample Questions |
| Treatment Process | What does the treatment involve? How long will it take? |
| Potential Side Effects | What are the common side effects? How can they be managed? |
| Recovery | What is the recovery process like? Are there any specific post-treatment care instructions? |
Being physically, mentally, and emotionally ready helps you face CT scans and radiation treatment with confidence and less worry.
Conclusion: Navigating Your Radiation and Imaging Journey
It’s important for patients to understand radiation therapy and imaging. These are key parts of cancer treatment. They help in diagnosing, treating, and following up on cancer.
Knowing about radiation therapy helps patients prepare better. They learn about imaging in treatment planning and the types of treatments. This knowledge lets them ask better questions and manage their expectations.
When starting the imaging journey, knowing what to expect helps. This includes CT scans, radiation mapping, and treatment. Being informed and prepared helps patients focus on recovery and navigate their journey with confidence.
FAQ
How soon after radiation therapy can I have a CT scan?
The timing for a CT scan after radiation therapy varies. It depends on if you need it and how your treatment is going. Your healthcare team will decide when it’s best for you.
What is radiation therapy and how does it work?
Radiation therapy kills cancer cells by damaging their DNA. It uses beams of radiation to target cancer cells. This way, it harms the cancer more than healthy cells.
How long does radiation treatment planning take?
Planning your radiation treatment takes a few days to weeks. It includes steps like your first visit, a CT scan, and making your treatment plan.
Can I use an existing CT scan for radiation treatment planning?
Sometimes, an old CT scan can be used for planning. But, if it’s not good enough, you might need a new one.
What should I expect during radiation mapping and treatment?
During radiation mapping, you’ll have a CT scan to make your plan. For treatment, you’ll lie on a table while beams of radiation target the cancer.
How does radiation therapy differ between palliative and curative approaches?
Palliative therapy aims to ease symptoms and improve life quality. Curative therapy tries to get rid of cancer. Their goals and imaging needs are different.
How can I prepare for CT scans and radiation treatment?
To get ready, follow diet and hydration advice. Also, preparing mentally and emotionally can help you through the treatment.
How long does a radiation treatment session take?
Treatment sessions are short, lasting just a few minutes. The exact time depends on the type of therapy and where you’re being treated.
What are the possible side effects of radiation therapy?
Side effects can include tiredness, skin issues, and damage to healthy tissue. Your team will talk to you about these risks and benefits.
How often will I need to have CT scans during radiation treatment?
How often you’ll need CT scans depends on your treatment goals and needs. Your healthcare team will decide the best schedule for you.
Reference
- Sun, A., Bae, K., Gore, E. M., Movsas, B., Bradley, J. D., & Werner-Wasik, M. (2011). Phase III trial of prophylactic cranial irradiation compared with observation in patients with locally advanced non–small-cell lung cancer: Neurocognitive and quality-of-life analysis. Journal of Clinical Oncology, 29(3), 279–286. https://pubmed.ncbi.nlm.nih.gov/21135270/