Last Updated on October 20, 2025 by

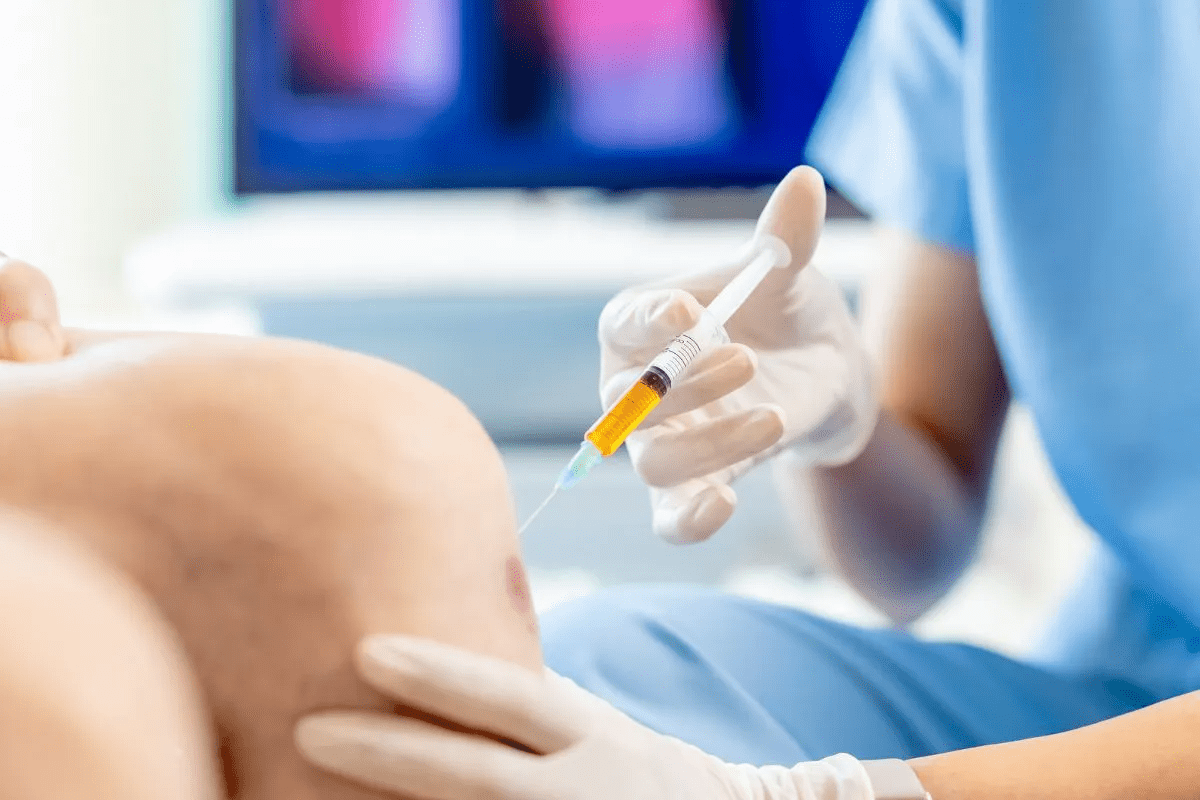
Administering platelets is a key medical action. It helps treat or prevent bleeding in patients with low platelet counts or dysfunctional platelets. At Liv Hospital, we focus on safe practices to ensure the best results for our patients. Platelet transfusion is a lifesaving method that stops or prevents bleeding in such cases.
We understand the vital role of platelets in stopping bleeding. Our guide helps healthcare professionals give safe and effective platelet transfusions.
Key Takeaways
- Understanding the importance of safe platelet administration practices.
- Recognizing the critical role of platelets in hemostasis.
- Identifying patients who require platelet transfusion.
- Outlining the key steps involved in administering platelets safely.
- Emphasizing the need for evidence-based platelet transfusions.
Understanding Platelets and Their Clinical Significance

Platelets are very important in medical settings. They help stop bleeding by forming clots. These small cells are found in the blood and play a key role in healing wounds.
What Are Platelets and Their Role in Hemostasis
Platelets are made in the bone marrow and live for about 8 to 12 days. They stick to injuries, gather with other platelets, and form a clot. This is vital for stopping blood loss.
Platelet activation is a complex process. It involves many biochemical signals that lead to their clumping. Knowing this helps us understand their role in health and disease.
Common Conditions Requiring Platelet Support
Many conditions need platelet transfusions. These include low platelet counts and platelet problems. Other reasons include major surgery, trauma, and some cancers.
- Thrombocytopenia due to bone marrow failure or chemotherapy
- Platelet dysfunction due to medications or underlying conditions
- Bleeding due to trauma or major surgery
Types of Platelet Products and Their Storage Requirements
There are different types of platelet products. These include random donor platelets and single donor platelets from apheresis. Platelets must be stored carefully to stay effective. They are kept at room temperature (20-24 °C) for up to 5 days.
It’s important to handle and store platelets correctly. This ensures they work well and are safe to use. Checking for bacteria is also key, as platelets can grow bacteria at room temperature.
Indications for Platelet Transfusion

Deciding to give platelet transfusions depends on the patient’s health and platelet count. These transfusions are key for patients with low platelets or platelet problems. Knowing when to give them is important for good care.
Prophylactic Transfusion Thresholds
When the platelet count drops below 10×10^9/L, a prophylactic transfusion is advised. This is based on guidelines to stop bleeding in severe cases. Following this rule can greatly lower the chance of bleeding in high-risk patients.
As professional education resources note, “platelet transfusions are for patients bleeding or at risk due to low platelets or dysfunction.” This highlights the need for quick action.
Therapeutic Transfusion in Active Bleeding
For active bleeding, a therapeutic transfusion is needed to control the bleeding. The choice to transfuse depends on the bleeding’s severity, platelet count, and other factors. Therapeutic transfusion is vital for managing severe bleeding in patients with low platelets or dysfunction.
“Platelet transfusion should be considered in patients with significant thrombocytopenia or platelet dysfunction who are experiencing major bleeding.”
Pre-Procedural Platelet Requirements
Before some medical procedures, platelet transfusions may be needed to prevent bleeding. The required platelet count varies by procedure and patient condition. Thorough evaluation of the patient’s platelet count and health is key to decide on pre-procedure transfusions.
Understanding when to give platelet transfusions helps healthcare providers improve patient care and reduce bleeding risks.
Pre-Transfusion Assessment and Planning
The journey of platelet transfusion starts with a detailed pre-transfusion assessment. This step is vital to ensure the transfusion is safe and effective. We focus on careful planning and evaluation to reduce risks and improve patient results.
Patient Evaluation and Informed Consent
Assessing the patient is key in pre-transfusion steps. We review the patient’s medical history, current health, and past transfusions or reactions. Informed consent is essential for safety. Patients need to know the risks and benefits of platelet transfusion and other options.
We make sure patients understand the procedure, possible complications, and how to report any issues. This empowers them and helps in their care.
Required Laboratory Testing
Before a platelet transfusion, we do lab tests for compatibility and to check the patient’s platelet count. These tests include:
- Complete Blood Count (CBC) to check the platelet count.
- Blood typing to check ABO and Rh compatibility.
- Screening for antibodies against platelet antigens.
| Laboratory Test | Purpose |
|---|---|
| Complete Blood Count (CBC) | Check the current platelet count |
| Blood Typing | Check ABO and Rh compatibility |
| Antibody Screening | Find antibodies against platelet antigens |
ABO Compatibility and Selection Criteria
ABO compatibility is very important in platelet transfusions. Even though platelets don’t show ABO antigens as much as red blood cells, using compatible platelets can lower the risk of bad reactions. We look at ABO compatibility and other factors like the patient’s health and past transfusions when choosing platelet products.
Patient Education About the Procedure
Telling patients about the platelet transfusion is key in pre-transfusion planning. We give them clear, simple information about what to expect during and after the transfusion. This includes possible side effects and signs of bad reactions. By educating patients, we help them take part in their care and improve their results.
Equipment and Supplies for Blood and Platelet Transfusion
Having the right equipment and supplies is key for safe platelet transfusions. Administering platelets needs several important parts. These must be ready and kept in good shape to protect patients and make transfusions work well.
Platelet Transfusion Tubing Requirements
The tubing for platelet transfusions helps keep the process safe. Platelet transfusion tubing has a filter. This filter takes out clots or debris that might have formed during storage.
Filter Specifications (170“260 µm)
Filters in platelet transfusion tubing have a 170“260 µm pore size. This size is important. It lets platelets through but keeps out big clots and debris. Using a filter in this range helps lower the chance of bad reactions.
Intravenous Access Considerations
Getting the right intravenous access is key for platelet administration. The size and type of intravenous catheter depend on the patient’s veins and how long the transfusion will take. Smaller gauge catheters are good for slower transfusions. Larger gauge catheters are better for faster ones.
Monitoring Equipment Preparation
Monitoring equipment is vital for transfusion safety. It includes vital sign monitors and tools to check the patient’s condition during and after the transfusion. We must make sure all monitoring gear is working right before starting the transfusion.
Some important monitoring tools are:
- Pulse oximeters
- Blood pressure monitors
- Cardiac monitors
Step-by-Step Platelet Administration Protocol
Administering platelets is a detailed process to ensure safety and effectiveness. We will walk you through the key steps. This includes verifying patient and product details to completing the transfusion.
Patient and Product Identification Verification
Before starting the transfusion, it’s vital to check the patient’s identity and the platelet product details. This step is key to avoid any transfusion mistakes. We suggest using at least two patient identifiers, like name and date of birth, and matching them with the product label.
As clinical guidelines stress, “accurate patient and product identification is critical for safe transfusions.”
Accurate identification is key to safe transfusion practices.
Setting Up the Transfusion Equipment
After verifying the patient and product, we set up the transfusion equipment. This includes the right tubing and filters (170“260 µm). We must ensure all equipment is correctly connected and ready to avoid delays or issues.
Initiating the Transfusion
With everything ready, we start the transfusion. It’s important to begin slowly and watch the patient closely for any adverse reactions. The transfusion should take 30-60 minutes, as guidelines suggest.
| Transfusion Parameter | Recommended Value |
|---|---|
| Transfusion Duration | 30-60 minutes |
| Filter Size | 170“260 µm |
| Monitoring Frequency | At least every 15 minutes |
Completing the 30-60 Minute Transfusion Process
During the transfusion, we keep an eye on the patient’s vital signs and watch for any adverse reactions. After finishing, we document the outcome, including any complications.
By following this protocol, healthcare professionals can ensure platelet transfusions are safe and effective. This helps provide the best care for patients.
Patient Monitoring During Platelet Administration
It’s vital to watch patients closely when giving platelet transfusions. This helps spot and handle any bad reactions quickly. Good monitoring means checking the patient before, during, and after the transfusion. It also includes keeping an eye on vital signs and looking for signs of trouble.
Pre-Transfusion Baseline Assessment
We do a detailed check on the patient before starting the transfusion. We look at their current health, medical history, and vital signs. Clinical guidelines say this is key to knowing what’s normal for the patient.
Vital Sign Monitoring Schedule
Keeping an eye on vital signs is a big part of caring for patients during transfusions. We check temperature, blood pressure, heart rate, and breathing rate often. The timing of these checks depends on the patient’s health and the transfusion plan.
| Monitoring Time | Vital Signs to Check |
|---|---|
| Before Transfusion | Temperature, Blood Pressure, Heart Rate, Respiratory Rate |
| During Transfusion (15-30 minutes) | Temperature, Blood Pressure, Heart Rate |
| After Transfusion | Temperature, Blood Pressure, Heart Rate, Respiratory Rate |
Signs and Symptoms of Adverse Reactions
Patients getting platelet transfusions need to be watched for bad reaction signs. These include fever, chills, low blood pressure, and allergic reactions. Canadian Blood Services says it’s important to watch for these closely.
“Patients should be closely monitored during transfusion for signs of adverse reactions, such as fever, chills, and hypotension.” – Canadian Blood Services
Documentation Requirements Throughout Transfusion
Keeping accurate records is key during platelet transfusions. We write down vital signs, any bad reaction signs, and transfusion details. Good records help care for the patient and talk to other doctors.
Managing Transfusion Reactions and Complications
Handling transfusion reactions needs a full plan, from spotting them to stopping them. These reactions can be mild or very serious. So, it’s key for doctors to stay alert and ready.
Identifying Common Adverse Reactions
Platelet transfusions can cause several issues. Febrile non-hemolytic transfusion reactions (FNHTR) make you feel feverish or get chills. Allergic reactions might show up as hives or, worse, anaphylaxis.
- Febrile non-hemolytic transfusion reactions (FNHTR)
- Allergic reactions
- Transfusion-associated circulatory overload (TACO)
Immediate Interventions for Reactions
If a reaction is thought to be happening, stop the transfusion right away. Check the patient’s vital signs quickly. Quick action is key to stop mild issues from getting worse. The team should be ready to give medicines like antihistamines or steroids.
- Stop the transfusion
- Assess the patient’s vital signs
- Administer appropriate medications
Transfusion-Associated Circulatory Overload (TACO) Prevention
TACO is a big problem that can be avoided with smart fluid management. Watching the patient’s fluid levels and adjusting the transfusion rate helps. Also, checking the heart before transfusion can spot risks.
Reporting and Documentation Procedures
It’s vital to report and document transfusion reactions well. Every reaction should be written down in the patient’s file, including what happened, what was done, and how the patient did. This info also goes to the blood bank or transfusion service.
By sticking to these steps, doctors can manage transfusion issues well. This ensures platelet transfusions are given safely.
Post-Transfusion Care and Evaluation
Checking how well a platelet transfusion worked involves looking at both how the patient feels and lab tests. This step is key to making sure the transfusion did what it was meant to do. It also helps spot any problems early.
Assessing Transfusion Effectiveness
To see if a platelet transfusion worked, we look at both how the patient feels and lab results. We check if the bleeding has stopped or decreased. Lab tests check the patient’s platelet count before and after to see if it went up right.
Post-Transfusion Laboratory Testing
Lab tests after a transfusion are vital to see if it worked and to catch any bad reactions. Canadian Blood Services says these tests show if the transfusion was a success. Tests like a complete blood count (CBC) check the platelet count and more to see how the patient is doing overall.
Monitoring for Delayed Reactions
While we know about quick reactions to platelet transfusions, delayed ones can happen too. These might include reactions that happen later or rare cases of graft-versus-host disease. Watching the patient closely and checking lab results over time is key to catching these.
Documentation of Transfusion Outcomes
Keeping accurate records of how a transfusion goes is very important. It helps us see if the transfusion worked, keeps track of how the patient reacted, and helps plan for future transfusions. Records should include what happened during the transfusion, how the patient did, any bad reactions, and lab test results.
Conclusion: Ensuring Safe and Effective Platelet Transfusion
Administering platelets safely and effectively is key for the best patient care. We’ve covered the main steps, from learning about platelets to caring for patients after transfusion.
It’s vital to follow platelet transfusion guidelines to ensure safety. This means doing a thorough check before transfusion, preparing the right equipment, and watching the patient closely during transfusion.
Good platelet transfusion needs a full plan. This includes knowing when to transfuse, handling any problems that might come up, and checking how well the transfusion worked. By sticking to these steps, doctors can reduce risks and improve patient outcomes.
In the end, safe and effective platelet transfusion is a big part of top-notch patient care. We stress the need for healthcare teams to keep learning about the latest in platelet transfusion.
FAQ
What is the role of platelets in hemostasis?
Platelets are key in stopping bleeding by forming clots. They gather at injuries, creating a plug to control blood loss.
What are the common conditions that require platelet support?
Conditions needing platelet support include low platelet counts and bleeding disorders. They also help patients with leukemia and those undergoing chemotherapy or bone marrow transplants.
What is the standard transfusion threshold for platelets?
The usual transfusion threshold for platelets is 10×10^9/L. But, this can change based on the patient’s health and other factors.
How do you administer platelets?
Platelets are given through a sterile IV line. Use a transfusion set with a 170-260 µm filter. Start slowly and watch for any bad reactions.
What equipment is required for platelet transfusion?
You’ll need platelet tubing, a 170-260 µm filter, and vital sign monitors. Also, make sure you have the right IV access.
How do you monitor patients during platelet administration?
Keep an eye on patients with regular vital sign checks. Watch for signs of bad reactions and document the transfusion process.
What are the signs and symptoms of adverse reactions to platelet transfusion?
Look out for fever, chills, rash, and breathing problems. Severe reactions include anaphylaxis and TRALI.
How do you manage transfusion reactions and complications?
Identify the reaction, stop the transfusion, and act quickly if needed. Follow reporting and documentation steps.
What is the importance of post-transfusion care and evaluation?
Post-transfusion care is vital. It checks if the transfusion worked, looks for delayed reactions, and documents the outcome.
Do platelets need a filter during transfusion?
Yes, platelets need a 170-260 µm filter to remove aggregates or debris formed during storage.
How fast should platelets be transfused?
Transfusion speed varies, but aim for 30-60 minutes. Start slow and adjust based on the patient’s comfort.
References
- Agarwal, A., Khan, A. I., & Anwer, F. (2024, June 6). Platelet transfusion. In StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560632/ NCBI
- Kaufman, R. M., Djulbegovic, B., Gernsheimer, T., Kleinman, S., Tinmouth, A. T., Capocelli, K. E., Cipolle, M. D., Cohn, C. S., Fung, M. K., Grossman, B. J., Mintz, P. D., O’Malley, B. A., Sesok-Pizzini, D. A., Shander, A., Stack, G. E., Webert, K. E., Weinstein, R., Welch, B. G., Whitman, G. J., Wong, E. C., & Tobian, A. A. R. (2015). Platelet transfusion: A clinical practice guideline from the AABB. Annals of Internal Medicine, 162(3), 205–213. https://doi.org/10.7326/M14-1589 American College of Physicians Journals+2PubMed+2
- Transfusion Ontario. (2023, July). Transfusionists Talk: PLTS website [PDF]. Retrieved from https://transfusionontario.org/wp-content/uploads/2023/07/Transfusionists-Talk-2023-June_PLTS_website.pdf
- Lifeblood. (n.d.). Transfusion process: Platelet administration. Retrieved from https://www.lifeblood.com.au/health-professionals/clinical-practice/transfusion-process/administration
- Yataco, A. C. (2025). Transfusion of fresh frozen plasma and platelets in … PMC. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12489387/ PMC
- “The clinical use of platelet transfusions: A systematic …” (2025). Transfusion. doi:10.1111/trf.18277 Wiley Online Library