Last Updated on October 31, 2025 by
Cervical cancer treatment has made big strides. It’s now a condition that can be managed well. Thanks to new therapies like surgery, chemotherapy, and radiation, more people are surviving.
At Liv Hospital, we give top-notch care for cervical cancer. We use the latest treatments and care for each patient like family. We choose treatments based on the cancer’s stage, the patient’s health, and what they prefer.
Effective treatment modalities are picked based on what each patient needs. Treatments might include surgery, radiation, chemotherapy, or a mix of these.
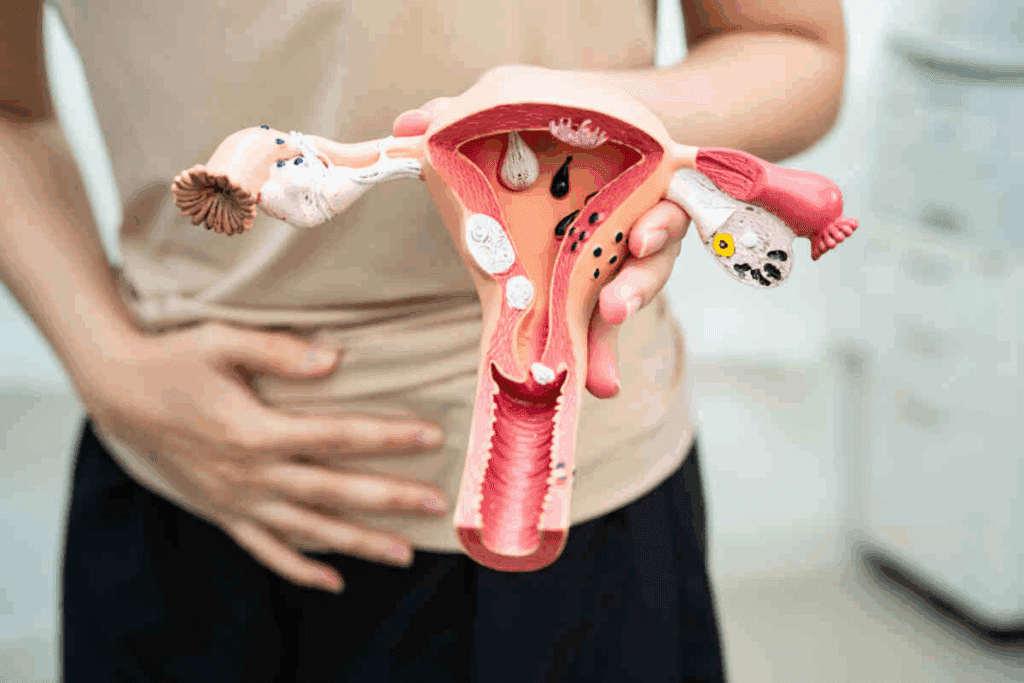
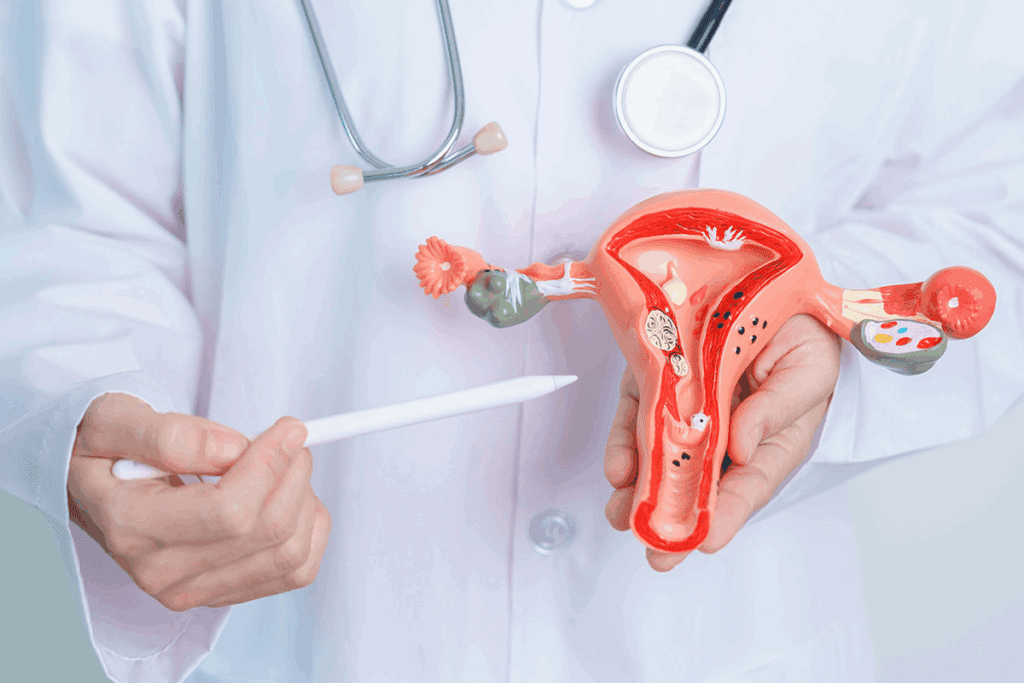
To treat cervical cancer well, we need to know a lot about it. This includes its causes, stages, and risk factors. Cervical cancer is a big health issue worldwide. It’s mainly caused by the human papillomavirus (HPV), which is a common sexually transmitted infection.
Cervical cancer often comes from a long-lasting HPV infection. Other things can raise your risk too. These include smoking, being immunosuppressed, and certain lifestyle choices.
Key Factors Contributing to Cervical Cancer:
The stage of cervical cancer depends on the tumor’s size and if it has spread. Knowing the stage helps pick the best treatment.
| Stage | Description |
| Stage I | Cancer is confined to the cervix |
| Stage II | Cancer has spread beyond the cervix but not onto the pelvic wall |
| Stage III | Cancer has extended to the pelvic wall and/or lower third of the vagina |
| Stage IV | Cancer has spread to distant organs or outside the pelvis |
There are many risk factors for cervical cancer. These include early sex, many partners, and smoking. But, we can lower the risk with HPV vaccines and Pap smears.
Prevention is key: Getting the HPV vaccine and getting regular Pap smears are important steps to prevent cervical cancer.
Knowing about cervical cancer’s causes, stages, and risk factors helps us fight it better. Regular screenings and HPV vaccines are key to stopping this disease.

Getting a correct diagnosis and staging is key to finding the best treatment for cervical cancer. This process is complex. It involves many tests and procedures to see how far the disease has spread.
Several tests are used to diagnose cervical cancer. These include Pap smears, HPV DNA tests, colposcopy, and biopsy. These tests look for abnormal cell changes in the cervix and confirm if cancer is present.
The International Federation of Gynecology and Obstetrics (FIGO) staging system is used to stage cervical cancer. This system helps determine the extent of the disease and guides treatment decisions.
The FIGO staging system categorizes cervical cancer into stages from I to IV, with subcategories within each stage. Knowing the stage of cervical cancer is critical for choosing the right treatment.
| FIGO Stage | Description | Typical Treatment Approach |
| Stage I | Cancer is confined to the cervix. | Surgery or radiation therapy. |
| Stage II | Cancer extends beyond the cervix but not to the pelvic wall. | Combination of radiation and chemotherapy. |
| Stage III | Cancer extends to the pelvic wall and/or causes hydronephrosis. | Radiation therapy with chemotherapy. |
| Stage IV | Cancer extends beyond the true pelvis or involves the mucosa of the bladder or rectum. | Palliative care or clinical trials. |
The stage of cervical cancer at diagnosis greatly affects the treatment plan. Early-stage disease may be treated with surgery or localized radiation. Advanced stages often require a combination of radiation therapy and chemotherapy.
Knowing the stage of cervical cancer helps us tailor the treatment to the individual’s needs. This improves outcomes and quality of life.
Surgery is a key part of treating cervical cancer. It offers different options based on the patient’s needs. The choice of surgery depends on the cancer’s stage, the patient’s health, and if they want to keep their fertility.
For early cervical cancer, less invasive methods like conization and Loop Electrosurgical Excision Procedure (LEEP) are often used. Conization removes a cone-shaped tissue sample from the cervix, helping diagnose and treat. LEEP uses a heated wire loop to remove affected tissue. Both are good for treating pre-cancerous lesions and early cervical cancer.
A hysterectomy, or the removal of the uterus, is a more serious surgery for cervical cancer. There are various types, like total hysterectomy and radical hysterectomy. The choice depends on the cancer’s extent and the patient’s situation.
For women wanting to keep their fertility, radical trachelectomy is an option. It removes the cervix, upper vagina, and surrounding tissues but keeps the uterus. This is for women with early-stage cancer who want to have children.
For advanced or recurring cervical cancer, pelvic exenteration might be needed. It removes reproductive organs, part of the rectum, and other tissues. It’s a major surgery but can save lives for some patients.
For many patients with cervical cancer, radiation therapy is a key part of their treatment. It helps target and destroy cancer cells. This helps control the disease and ease symptoms.
External beam radiation therapy (EBRT) is a common treatment for cervical cancer. It uses high-energy beams from outside the body to hit the tumor. EBRT can be adjusted to fit each patient’s needs, aiming for the cancer while protecting healthy tissues.
Benefits of EBRT include:
Brachytherapy places a small amount of radioactive material inside or near the tumor. This method delivers high doses of radiation right to the cancer cells. It helps protect healthy tissues nearby.
Advantages of brachytherapy include:
Radiation therapy is effective against cervical cancer but can cause side effects. Common issues include fatigue, skin reactions, and stomach problems. It’s important to manage these side effects to keep the patient’s quality of life good during treatment.
| Side Effect | Management Strategy |
| Fatigue | Rest, exercise, and nutrition counseling |
| Skin Reactions | Topical creams, gentle skin care |
| Gastrointestinal Issues | Dietary adjustments, medication |
Understanding radiation therapy options and their side effects helps patients make informed choices. Our team is dedicated to giving full care and support during treatment.
Chemotherapy is a key treatment for cervical cancer. It targets cancer cells that have spread or are at high risk. It’s often used with surgery or radiation therapy.
Cisplatin is a common chemotherapy drug for cervical cancer. It damages cancer cells’ DNA, stopping them from growing. Cisplatin-based treatments are very effective, often used with radiation therapy.
A typical regimen involves cisplatin once a week during radiation. This approach has improved survival rates for patients with advanced cervical cancer.
Chemotherapy can be given at different times. Neoadjuvant chemotherapy is before the main treatment, like surgery. It makes tumors smaller. Adjuvant chemotherapy is after the main treatment to kill any remaining cancer cells.
In cervical cancer, both types of chemotherapy are important. Neoadjuvant chemotherapy can make surgery easier and better. Adjuvant chemotherapy lowers the chance of cancer coming back.
| Chemotherapy Type | Purpose | Timing |
| Neoadjuvant Chemotherapy | Shrink tumors before main treatment | Before surgery or radiation |
| Adjuvant Chemotherapy | Eliminate remaining cancer cells | After surgery or radiation |
Chemotherapy is effective but can cause side effects. These include nausea, fatigue, hair loss, and low blood cell counts. It’s important to manage these side effects to keep patients’ quality of life good.
We use many ways to reduce side effects. Anti-nausea drugs help with nausea and vomiting. Growth factors boost blood cell counts. Patients are also advised on nutrition to stay strong during treatment.
By managing side effects and tailoring treatments, we can make chemotherapy more effective. This helps patients live better lives during treatment.
Immunotherapy, using immune checkpoint inhibitors, is changing how we treat cervical cancer. It has shown great promise in helping patients with advanced or recurrent disease live longer.
Immune checkpoint inhibitors help the immune system fight cancer better. Pembrolizumab, an anti-PD-1 therapy, has been very effective in treating cervical cancer.
This treatment is a big step forward for cervical cancer patients. It offers hope to those with few treatment options.
The KEYNOTE-A18 trial showed pembrolizumab’s benefits in cervical cancer treatment. It found that adding pembrolizumab to standard treatment improved survival rates in patients with locally advanced cervical cancer.
| Trial | Treatment | Outcome |
| KEYNOTE-A18 | Pembrolizumab + Chemoradiation | Improved Survival Outcomes |
| Standard Treatment | Chemoradiation Alone | Baseline Survival Outcomes |
Targeted therapies are also being explored for cervical cancer treatment. These therapies aim to target specific molecular mechanisms that drive cancer growth and progression.
Some emerging targeted therapies target the PI3K/AKT/mTOR pathway and inhibit angiogenesis. While these therapies are in the early stages, they show promise for better treatment outcomes.
Not all cervical cancer patients will benefit from immunotherapy. It’s important to choose the right patients for this treatment. Biomarkers like PD-L1 expression help predict who will respond best to immune checkpoint inhibitors.
We are working to better understand how to select patients for immunotherapy. This ensures that those most likely to benefit from these treatments receive them.
Using different treatments together is key in fighting cervical cancer. This method helps doctors create a plan that fits each patient’s needs. It might lead to better results.
Chemoradiation therapy mixes chemotherapy and radiation. It’s a main treatment for many cervical cancer patients. This method has been proven to boost survival chances by tackling both local and widespread disease. It works best for those with advanced cervical cancer.
Chemotherapy and radiation work together well. Chemotherapy makes cancer cells more vulnerable to radiation. This makes the radiation therapy more effective at killing cancer cells.
The INTERLACE trial showed the benefits of sequential therapy in cervical cancer treatment. This study looked at starting with chemotherapy and then chemoradiation. It found better survival rates than just chemoradiation alone.
Sequential therapy helps tailor the treatment order. It might lead to better results by shrinking tumors before the main treatment.
Immunotherapy is being tested with chemoradiation for cervical cancer. Adding immunotherapy could boost the body’s fight against cancer. This might result in better treatment outcomes.
Studies are underway to check if combining immunotherapy with chemoradiation is safe and effective.
Maintenance therapy is part of the combined treatment for cervical cancer. This involves extra treatments after the first round to keep the disease under control. It aims to improve long-term results.
Maintenance therapy might include ongoing chemotherapy, targeted therapy, or other treatments. It depends on how well the patient responds to the first treatment and their overall health.
Knowing the stage of cervical cancer is key to a good treatment plan. We tailor our approach to each patient’s needs. This is because treatment plans change with the cancer’s stage.
Early-stage cervical cancer (Stages I-IIA) often gets less invasive treatments. Surgery is usually the first choice for early-stage cancer. It aims to cure the cancer with little impact on daily life.
We look at the patient’s health, fertility wishes, and tumor details to pick the best surgery. Sometimes, a conization or LEEP procedure can remove the cancer while keeping fertility. But for more serious cases, a hysterectomy might be needed. We talk about the pros and cons with our patients to help them decide.
For locally advanced cervical cancer (Stages IIB-IVA), treatment gets more intense. Chemoradiation therapy is often used. This combo has been shown to improve survival rates over radiation alone.
We help our patients manage chemoradiation side effects and provide the care they need. The INTERLACE trial shows that starting with chemotherapy followed by radiation can boost survival for locally advanced disease. We keep up with new research to offer the best treatments.
Metastatic cervical cancer (Stage IVB) focuses on improving quality of life. Chemotherapy and targeted therapies aim to slow cancer growth and ease symptoms. We create a care plan that meets our patients’ physical, emotional, and social needs.
Dealing with recurrent cervical cancer is tough. Treatment depends on where and how far the cancer has spread. Surgery, radiation, or chemotherapy might be used alone or together. We carefully choose the best treatment for each case, considering past treatments and health.
In some cases, immunotherapy or targeted therapies might be suggested for clinical trials or compassionate use. We keep our patients updated on new treatments and discuss their benefits and risks.
A team of doctors from different specialties is key for treating cervical cancer. They work together to create a treatment plan that fits each patient’s needs.
Gynecologic oncologists are experts in treating gynecologic cancers, including cervical cancer. They are skilled surgeons who perform surgeries like hysterectomies. They also lead the team in planning the treatment.
Radiation oncologists are vital for treating cervical cancer with radiation. They help decide the best radiation plan. This could be external beam radiation or brachytherapy, to control the tumor and reduce side effects.
Medical oncologists are important for patients with advanced cervical cancer. They give chemotherapy and manage side effects. They work with the team to ensure a complete treatment plan.
Supportive care specialists help with the physical and emotional symptoms of cervical cancer. They support patients and their families, improving their quality of life during treatment.
| Team Member | Role in Cervical Cancer Treatment |
| Gynecologic Oncologists | Surgical management and leading the treatment team. |
| Radiation Oncologists | Providing radiation therapy expertise. |
| Medical Oncologists | Administering chemotherapy and managing systemic treatments. |
| Supportive Care Specialists | Managing symptoms and providing patient support. |
Recent breakthroughs in cervical cancer treatment have given patients and their families new hope. We’ve seen big steps forward in surgery, radiation, chemotherapy, and immunotherapy. These advancements offer better treatment choices and results.
Now, treatments like chemoradiation therapy and immunotherapy combined with chemoradiation are available. Ongoing research and clinical trials, like the KEYNOTE-A18 trial, keep bringing hope for better lives and outcomes.
Is there a cure for cervical cancer? While it depends on the stage and situation, we’re seeing better survival rates and treatment options. The most effective treatment often involves a team of specialists in gynecologic oncology, radiation oncology, and medical oncology.
As we keep moving forward in cervical cancer treatment, we’re committed to top-notch healthcare for international patients. These advances in treatment bring hope for better lives and outcomes. We’re here to help patients understand their treatment options.
We have many ways to treat cervical cancer. These include surgery, radiation, chemotherapy, and immunotherapy. We often use them together for the best results.
We use the FIGO staging system for cervical cancer. It’s key because it helps us decide on treatment. It also helps predict how well a patient will do.
We have several surgeries for cervical cancer. These include conization, LEEP, hysterectomy, and radical trachelectomy. The choice depends on the disease’s stage and the patient’s wishes.
Radiation therapy targets and kills cancer cells. We use external beam radiation and brachytherapy. It can be used alone or with other treatments.
Chemotherapy is used to treat cervical cancer. We often use cisplatin-based regimens. It can be used before or after surgery, or with radiation therapy.
Immunotherapy uses the body’s immune system to fight cancer. We use it for advanced or recurrent cervical cancer. Treatments like pembrolizumab are examples.
We look at several things to choose the best treatment. These include the disease’s stage, the patient’s health, and their preferences.
Our team includes gynecologic oncologists, radiation oncologists, and more. We work together for the best care and outcomes for our patients.
Many patients with cervical cancer can be cured today. Early diagnosis is key. Treatment outcomes depend on the disease’s stage.
Maintenance therapy, like immunotherapy, helps keep treatment working. It can prevent cancer from coming back.
Yes, we’re part of clinical trials like the KEYNOTE-A18 trial. They help us find new treatments for cervical cancer.
We have many options for metastatic or recurrent cervical cancer. These include chemotherapy, immunotherapy, and palliative care. They help manage symptoms and improve life quality.
HPV vaccination is key in preventing cervical cancer. It protects against the virus that causes most cases of the disease.
Regular Pap smears can find abnormal cell changes early. This can lead to early treatment and may prevent cervical cancer.
For early-stage cervical cancer, we might suggest surgery. This could be conization or hysterectomy. The choice depends on the patient’s needs.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!