Last Updated on November 4, 2025 by mcelik

Learning about brain tumor removal surgery can help during a tough time. At Liv Hospital, our skilled neurosurgeons and caring team make sure each brain cancer surgery is done with care and precision. Learn How to Decompress Spine safely at home using gentle stretches and posture adjustments.
We use the latest surgical methods to treat both bad and good brain masses. Our goal is to offer top-notch healthcare, giving hope and clear answers at every step.
Our team works hard to give complete care, from finding the problem to getting better. By picking Liv Hospital, patients know they’re getting the best treatment for their situation.
Key Takeaways
- Advanced surgical techniques are used for brain tumor removal.
- Liv Hospital provides personalized patient care and compassion.
- Both malignant and benign tumors can be surgically addressed.
- Our neurosurgeons are experts in their field.
- Comprehensive care is provided from diagnosis through recovery.
Understanding Brain Tumors and Their Classification
It’s key for patients to understand brain tumors to make good care choices. Brain tumors can really affect a person’s life quality. Knowing about your condition helps in the treatment journey.
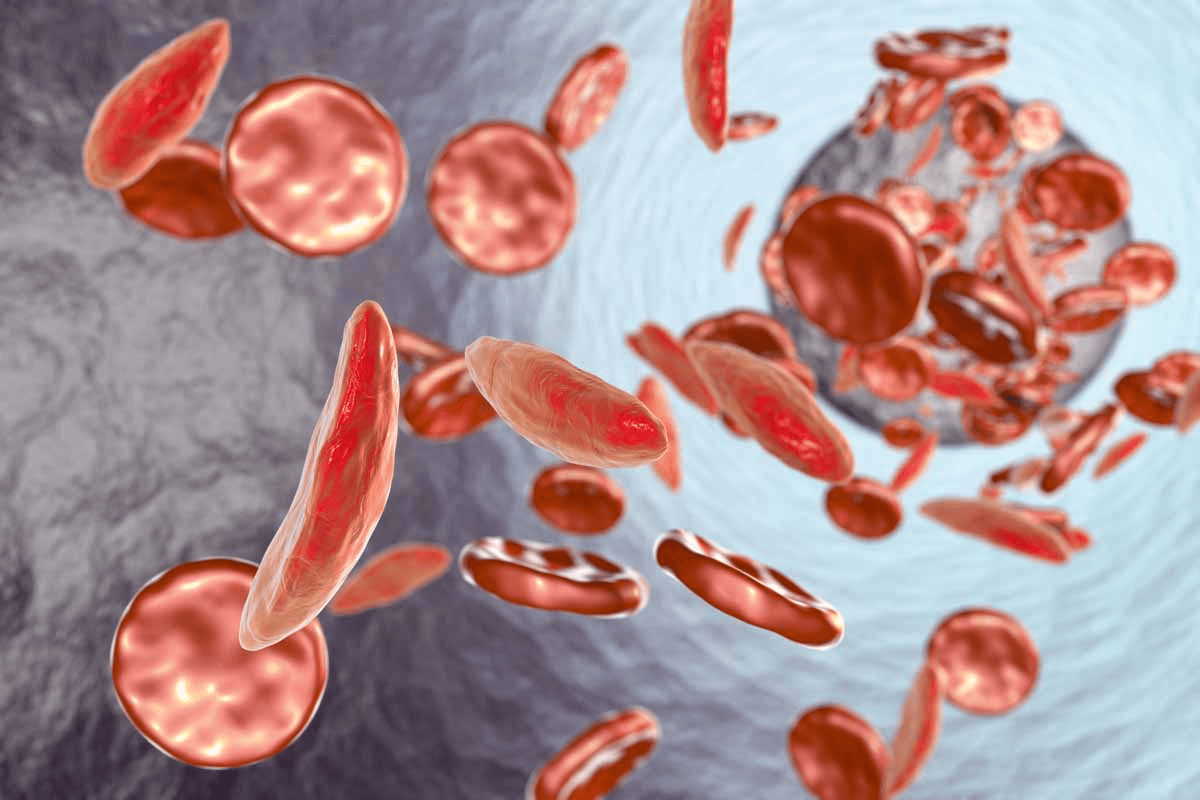
Types of Brain Tumors: Malignant vs. Benign
Brain tumors fall into two main types: malignant and benign. Malignant tumors are cancerous, grow fast, and spread to other brain areas. Benign tumors are not cancerous, grow slower, and don’t spread. But, they can cause issues because of where they are and how big they get.
Common Locations and Growth Patterns
Brain tumors can happen in different brain areas, affecting people in various ways. Some tumors grow in important brain spots, while others are in less critical areas. Knowing where and how tumors grow helps doctors choose the best treatment.
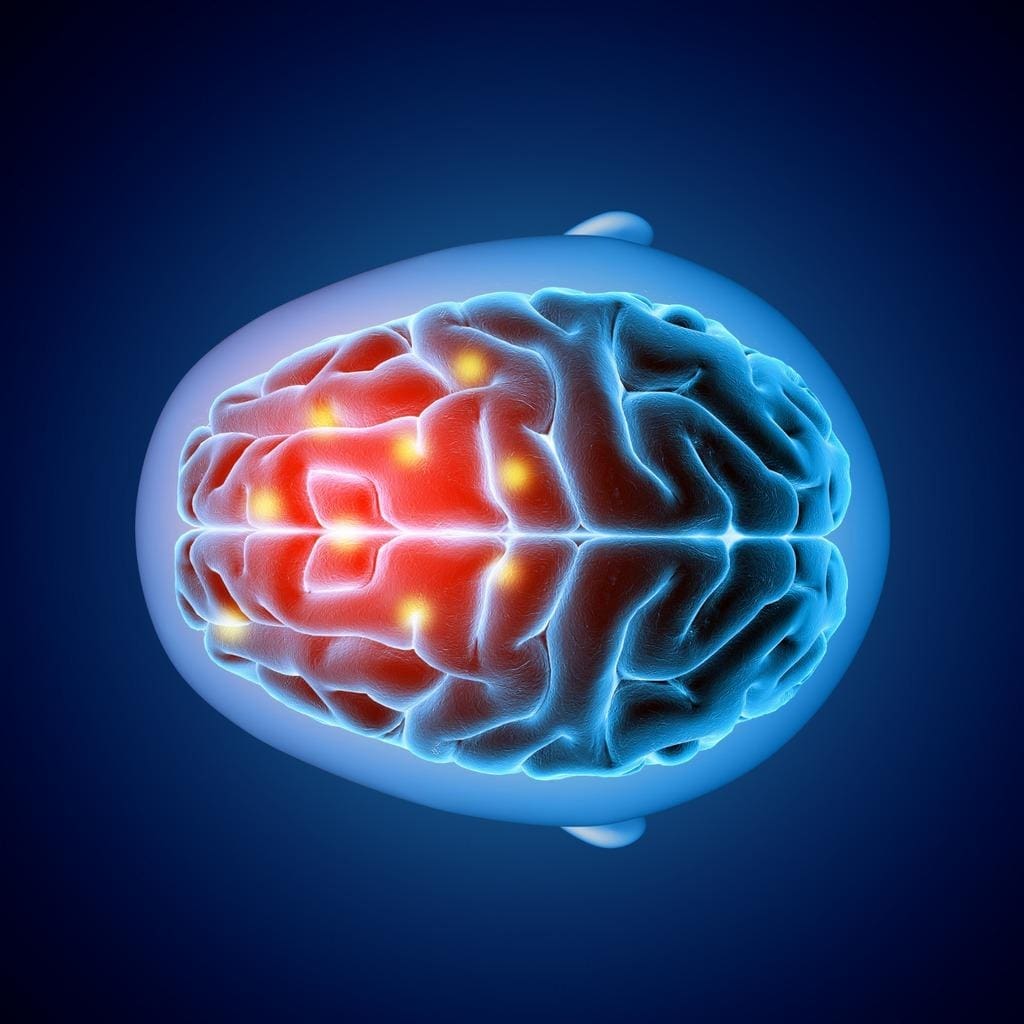
Symptoms That Indicate Surgical Intervention
Symptoms of brain tumors vary based on the tumor’s location, size, and type. Common signs include headaches, seizures, and weakness or numbness. Sometimes, surgery is needed to ease these symptoms and improve life quality. Spotting these symptoms early is key to deciding if surgery is needed.
Comprehensive Diagnostic Process

Understanding a brain tumor starts with a detailed diagnostic process. We use advanced tools to learn about the tumor’s type. This is key for creating a good treatment plan.
Advanced Imaging Techniques
Imaging is key in finding brain tumors. We use MRI (Magnetic Resonance Imaging), CT (Computed Tomography), and PET (Positron Emission Tomography) scans. Each scan gives us different info.
MRI shows soft tissues well, CT scans quickly check tumor size and location, and PET scans spot active areas. These scans work together to give a full picture of the tumor.
MRI is great for soft tissues, while CT scans are better for seeing calcifications. PET scans show where the tumor is most active, which can mean it’s cancerous.
Biopsy Procedures and Tissue Analysis
Imaging is helpful, but a biopsy is needed for a sure diagnosis. We take tissue samples from the tumor. Then, we study them under a microscope.
This study tells us about the tumor’s type, how aggressive it is, and its genetic makeup. It’s vital for planning treatment. We use special staining and molecular tests to learn more about the tumor cells.
Functional Brain Mapping
We also map the brain to see how the tumor affects it. This includes using fMRI and EEG. These tools help us see how brain functions like movement and language are impacted.
This mapping is important for surgery planning. It helps us know which brain areas to protect. By knowing this, we can make surgery safer and more precise.
Selecting Your Surgical Team
Choosing the right surgical team for brain tumor surgery is key. The success of your surgery depends on your neurosurgeon’s skills and the teamwork. A good team can make a big difference.
Qualifications to Look For in a Neurosurgeon
Finding a neurosurgeon with the right qualifications is important. Look for a board-certified neurosurgeon with lots of experience in brain tumor surgery. They should know the latest techniques and have a focus on neuro-oncology.
Dr. John Smith, a top neurosurgeon, says, “A neurosurgeon’s experience with complex cases is key.” They need to know how to handle the brain’s complex anatomy and any complications that might come up.
The Multidisciplinary Approach
A team approach is vital for your care. Your team should include oncologists, radiologists, and rehabilitation specialists too. They work together to create a treatment plan that covers all your needs.
“The integration of various medical specialties ensures that patients receive holistic care, improving outcomes and quality of life.” – Dr. Jane Doe, Neuro-Oncologist
Questions to Ask Before Committing
Before choosing your team, ask important questions. Find out about their experience with cases like yours, how they handle brain tumor removal, and the technology they use. Also, ask about support during recovery.
- What is your neurosurgeon’s experience with brain tumor surgeries?
- How does the team approach complex or challenging cases?
- What support services are available during recovery?
Choosing the right team can greatly affect your recovery. A team with the right skills and a team effort can lead to the best results for your surgery.
Pre-Surgical Evaluation and Planning
Before brain tumor surgery, a detailed evaluation is key for the best results. This important step includes many assessments and plans. It aims to increase the success rate of brain tumor resection.
Determining Tumor Operability
The first step is to check if the tumor can be removed. We look at the tumor’s size, location, and how it affects nearby brain areas. Advanced imaging like MRI and CT scans help us understand the tumor better.
Some tumors are too risky to remove because of their location or how close they are to important brain parts. In these cases, treatments like radiation or chemotherapy might be suggested instead.
Surgical Risk Assessment
After deciding if the tumor can be removed, we assess the surgery’s risks. We look at the patient’s health, medical history, and possible surgery complications.
- Checking the patient’s neurological status
- Looking at past medical conditions and allergies
- Identifying risks of complications
Knowing these risks helps us find ways to reduce them. This ensures the best possible outcome for the patient.
Creating a Personalized Surgical Plan
Creating a personalized surgical plan is a critical part of planning. It means customizing the surgery to fit the patient’s specific needs and tumor type.
Our team uses cutting-edge tools like neuronavigation and functional brain mapping for planning. This helps us find the safest path for surgery and avoid harming important brain areas.
With careful evaluation and planning, we can greatly improve surgery success and recovery for our patients.
Preparing for Brain Tumor Removal Surgery
Getting ready for brain tumor surgery is a big step. It includes medical checks, adjusting medicines, and getting mentally ready. We’ll walk you through each step to help you prepare for a good outcome.
Medical Preparations and Testing
Before surgery, you’ll need to go through many medical tests. These tests check your health and find any risks. You might have:
- Blood tests to look for infections or bleeding problems
- An electrocardiogram (ECG) to check your heart
- Imaging tests like MRI or CT scans to find the tumor
- Other tests your neurosurgeon might suggest
Table: Pre-Surgical Medical Tests
| Test | Purpose |
| Blood Tests | To check for infections, blood type, and bleeding disorders |
| Electrocardiogram (ECG) | To assess heart health and detect any cardiac issues |
| MRI/CT Scans | To precisely locate the tumor and plan the surgical approach |
Medication Adjustments
Some medicines might need to be changed or stopped before surgery. We ask you to:
- Tell us about all your medicines, including supplements and herbal remedies
- Follow our instructions on changing your medicines
- Avoid blood-thinning medicines unless we tell you to
“It’s important to follow your doctor’s instructions on changing medicines for a safe surgery.”
Day-Before and Day-of Instructions
We give you detailed instructions for the day before and the day of surgery. These include:
- What to eat or not eat
- How to bathe or shower
- When and where to arrive
Psychological Preparation for Patient and Family
Getting ready for surgery is not just about the body. It’s also about your mind. We suggest:
- Talking about your worries and questions with your healthcare team
- Getting support from loved ones or support groups
- Trying relaxation techniques like meditation or deep breathing
By following these steps and working with your healthcare team, you can be well-prepared for surgery.
The Craniotomy Procedure Explained
The craniotomy procedure is a key step in removing brain tumors. It needs a lot of skill and care. We know it can be scary for patients and their families. So, we’re here to help you understand every part of it.
Anesthesia Administration and Monitoring
Before starting, anesthesia administration is very important. It makes sure the patient is comfortable and safe. We watch the patient’s vital signs closely during the surgery.
This includes checking blood pressure, heart rate, and oxygen levels. The anesthesia team works with the neurosurgeons to keep the patient stable and pain-free.
Surgical Positioning and Draping
Getting the patient in the right position is key. It helps us reach the tumor safely. Our team carefully places the patient on the table, using supports and restraints as needed.
Surgical draping is then done to keep the area clean and prevent infection. This is a critical step for a successful surgery.
Scalp Incision and Bone Flap Removal
Next, we make a scalp incision. We plan it carefully to access the tumor and keep scarring down. The size and location of the incision depend on the tumor.
Then, we remove a part of the skull, called a bone flap, for the craniotomy. This lets us get to the brain and the tumor. We save the bone flap to put back at the end.
Awake Craniotomy: When and Why
Sometimes, we do an awake craniotomy. This means the patient is awake during part of the surgery. It helps us check brain function in real-time. It’s useful for tumors near important brain areas.
An awake craniotomy needs careful patient selection and a skilled team. We explain everything to the patient and make sure they’re ready and comfortable.
Brain Tumor Removal Surgery: Step-by-Step Process
Removing a brain tumor is a complex process. Our neurosurgeons follow several key steps. They use advanced technology and know the brain’s anatomy well.
Dural Opening and Brain Exposure
The first step is opening the dura mater, the brain’s outermost layer. This lets us get to the tumor without harming the brain. It’s a critical step.
Tumor Localization Techniques
Finding the tumor’s exact location is essential. We use MRI and CT scans for this. We also have systems that guide us during surgery for better accuracy.
Resection Methods Based on Tumor Type
The way we remove the tumor depends on its type and size. Some tumors can be removed completely, while others need a partial removal. We choose the best method for each patient.
Preserving Eloquent Brain Areas
It’s important to protect the brain’s key areas. These areas control important functions like speech and movement. We use special techniques to avoid harming these areas.
Our team’s careful planning and skill help patients get the best results from brain tumor surgery.
Advanced Surgical Techniques for Brain Mass Removal
New surgical methods have changed neurosurgery, giving hope to those with brain tumors. These advanced techniques have made surgeries better, cutting down on recovery time and risks.
Neuronavigation and Computer-Guided Surgery
Neuronavigation systems give surgeons real-time feedback, making tumor removal more precise. This tech uses advanced imaging to guide the surgery. It helps locate tumors and avoid damage to important brain areas.
Benefits of Neuronavigation:
- Improved accuracy in tumor localization
- Reduced risk of damage to surrounding brain tissue
- Enhanced surgical planning and execution
Laser Interstitial Thermal Therapy
Laser Interstitial Thermal Therapy (LITT) uses laser energy to kill tumor cells. It’s great for tumors in hard spots or for those not good for open surgery.
LITT offers several advantages, including:
- Minimally invasive approach, reducing tissue damage
- Real-time temperature monitoring for safe treatment
- Potential for quicker recovery times
Minimally Invasive Endoscopic Approaches
Endoscopic surgery uses a small camera and tools to remove tumors through small cuts. This method can lead to faster recovery and less scarring.
| Technique | Benefits | Applications |
| Endoscopic Surgery | Minimally invasive, less scarring, quicker recovery | Tumors in accessible locations |
| LITT | Precise tumor destruction, real-time monitoring | Deep-seated or hard-to-reach tumors |
| Neuronavigation | Enhanced precision, reduced risk to surrounding tissue | Complex tumor resections |
Fluorescence-Guided Surgery with 5-ALA
Fluorescence-Guided Surgery (FGS) with 5-Aminolevulinic Acid (5-ALA) helps surgeons see tumors during surgery. The tumor glows under special light, making removal easier.
FGS with 5-ALA has been shown to improve tumor removal. This could lead to better outcomes for patients.
Potential Complications and Risk Management
Brain tumor removal surgery is a lifesaving procedure but comes with risks. It’s important for patients and their families to understand these risks. This knowledge helps in managing complications.
Immediate Surgical Risks
Immediate risks include bleeding, infection, and reactions to anesthesia. We take every precaution to reduce these risks. We use advanced imaging and monitor patients closely during surgery.
Neurological Deficits and Management
Neurological deficits can happen due to the tumor’s location or surgery. Our team works closely with patients to manage these deficits. We use physical, speech, and occupational therapy as needed.
Infection Prevention Protocols
Infection prevention is a top priority. We adhere to strict protocols to prevent infections. This includes antibiotics, sterile techniques, and post-operative care.
Seizure Management Strategies
Seizures can be a complication of brain tumor surgery. We employ strategies to manage seizures. This includes anti-seizure medications before, during, and after surgery.
By understanding and addressing these complications, we can significantly improve outcomes. Our multidisciplinary approach ensures care from preparation to recovery.
Post-Operative Recovery Journey
After brain tumor surgery, patients start a recovery journey watched over by their healthcare team. This journey is key to the best outcomes. It includes stages from intensive care to rehabilitation.
Intensive Care Monitoring Phase
The first part of recovery is in the ICU, where patients are watched for immediate complications. This can be scary for patients and their families. Our team offers caring support during this time.
In the ICU, our medical team checks vital signs and neurological status closely. They watch for any complications. This helps us fix issues quickly and move to the next recovery stage smoothly.
Hospital Recovery Timeline
The time in the hospital varies based on the patient’s condition and surgery complexity. Patients usually stay a few days. During this time, we manage pain, prevent infections, and start rehabilitation.
We encourage patients and families to ask questions and help with care decisions. This teamwork helps in the recovery process.
| Day | Typical Activities | Care Focus |
| 1-2 | Rest, vital sign monitoring | Pain management, neurological checks |
| 3-4 | Mobilization, physical therapy begins | Preventing complications, wound care |
| 5+ | Continued physical therapy, occupational therapy | Rehabilitation, discharge planning |
Pain Management Approaches
Managing pain is key in recovery. We use medicines and other methods tailored to each patient. This ensures comfort and reduces pain.
Our team works with patients to adjust pain treatment plans. This helps keep them comfortable and pain-free.
Physical and Occupational Therapy
Physical and occupational therapy are important in rehab. They help patients regain strength and independence. Our therapists create plans that meet each patient’s needs and goals.
We are dedicated to supporting our patients throughout their recovery. Knowing what to expect helps patients and families during this tough time.
Conclusion: Navigating Life After Brain Tumor Surgery
After brain tumor surgery, patients often wonder about the long-term effects. The journey doesn’t stop with surgery; it’s a big step towards getting better. The outcome depends on the tumor’s type, location, and the patient’s health.
Removing a brain tumor is a complex task. Life after surgery needs careful follow-up care. Regular check-ups and monitoring are key to the best outcome. Many patients can live a normal life again with the right care.
Life after surgery isn’t just about medical care. It’s also about supporting the patient and their family. We aim to provide all-around care for our patients. Understanding what to expect helps patients prepare for their journey.
FAQ
References:
• UC Health. (n.d.). [PDF] Craniotomy basic level. https://www.uchealth.com/wp-content/uploads/2013/01/PE-Craniotomy_UCNI.pdf
What is brain tumor removal surgery?
Brain tumor removal surgery, also known as craniotomy, is a procedure to remove a brain tumor. A neurosurgeon uses advanced techniques and technology for the best results.
How are brain tumors diagnosed?
To diagnose brain tumors, we use MRI, CT, and PET scans. We also do biopsy procedures and tissue analysis, and functional brain mapping.
What are the differences between malignant and benign brain tumors?
Malignant tumors are cancerous and grow fast. Benign tumors are not cancerous and grow slower. We choose the best treatment based on the tumor and patient needs.
What are the qualifications to look for in a neurosurgeon for brain tumor removal surgery?
Look for a board-certified neurosurgeon with brain tumor surgery experience. They should have a team approach to care. Ask about their experience and success rates.
What is the pre-surgical evaluation and planning process like?
We check if a tumor can be removed and assess risks. We create a plan tailored to you. This preparation helps ensure a good surgery outcome.
How do I prepare for brain tumor removal surgery?
Follow our instructions for medical preparations and medication adjustments. We also guide you on psychological preparation for you and your family.
What is a craniotomy procedure?
A craniotomy involves making an incision, removing part of the skull, and accessing the brain. We use advanced techniques to ensure your comfort and safety.
What are the possible complications of brain tumor removal surgery?
Possible complications include immediate risks, neurological deficits, infection, and seizures. We have strategies to manage these risks and will discuss them with you.
What is the recovery process like after brain tumor removal surgery?
Recovery involves intensive care, hospital stay, pain management, and therapy. We provide care and support for a smooth recovery and best outcomes.
What are the long-term outcomes after brain tumor surgery?
Outcomes vary based on the tumor type, patient factors, and surgery success. We guide you on follow-up care and rehabilitation to support your recovery.
Can all brain tumors be removed surgically?
Not all brain tumors can be removed surgically. We assess each case to determine the best treatment.
What are the benefits of minimally invasive brain surgery?
Minimally invasive surgery offers smaller incisions, less tissue damage, and faster recovery. We use these techniques when possible to improve outcomes.
How do you manage pain after brain tumor removal surgery?
We use medication and other therapies to manage pain during recovery. This ensures your comfort during the process.