Last Updated on November 26, 2025 by Bilal Hasdemir
how to know chemo is working
Knowing if chemotherapy works is key for cancer patients. A good response to chemotherapy can greatly improve treatment results and patient health.
There are many signs and tests to check if chemotherapy is working. We will look at the main indicators of a positive response. This will help clear up the complex part of cancer treatment.
Understanding how well chemotherapy works is very important. It helps both patients and doctors make better choices for care.
Key Takeaways
- A good response to chemotherapy is vital for improving cancer treatment outcomes.
- Various tests and signs help determine the effectiveness of chemotherapy.
- Understanding chemotherapy response is crucial for managing patient expectations.
- Factors influencing chemotherapy efficacy include the type of cancer and treatment regimen.
- Informed decision-making is key to optimizing cancer care.
Understanding Chemotherapy and Treatment Goals

Chemotherapy is a treatment that uses drugs to kill cancer cells. Its success depends on the cancer type and stage. Knowing how chemotherapy works is key for both patients and doctors.
How Chemotherapy Works
Chemotherapy targets fast-growing cells, like most cancer cells. It uses drugs that stop these cells from dividing. Chemotherapy can be given in different ways, like orally or through an IV. The method depends on the cancer type and the drugs used.
Chemotherapy also affects healthy cells that grow fast. This can cause side effects like hair loss, nausea, and tiredness.
Different Types of Chemotherapy Treatments
Chemotherapy treatments vary based on their purpose and the drugs used. Neoadjuvant chemotherapy is given before main treatments to shrink tumors. Adjuvant chemotherapy is after main treatments to kill any remaining cancer cells.
Other types include induction, consolidation, and palliative chemotherapy. Each has its own goal.
- Combination chemotherapy uses multiple drugs to attack cancer cells from different angles.
- Targeted therapy is used with chemotherapy to target specific cancer cell traits.
Setting Realistic Treatment Expectations
It’s important to have realistic expectations when undergoing chemotherapy. Knowing the treatment goals and possible side effects helps patients cope. Good communication between patients and doctors is key for managing expectations and making informed decisions.
We consider the cancer stage, patient health, and past treatments when setting expectations. This helps patients understand their treatment better.
Defining Treatment Response in Oncology
Understanding treatment response in oncology is key. It shows how well a patient’s cancer reacts to treatment, like chemotherapy. We divide treatment response into types based on how the cancer acts during and after treatment.
Complete Response vs. Partial Response
A complete response means all cancer is gone after treatment. It’s a big win, but it doesn’t always mean the cancer is fully cured. A partial response shows the cancer has shrunk a lot, but some is still there.
Both are good signs, showing the treatment is working. But, the exact meaning depends on the cancer type, its stage, and the patient’s health.
Stable Disease vs. Progressive Disease
Stable disease means the cancer isn’t getting bigger or smaller. It’s not the best outcome, but it’s okay if the cancer was expected to grow. On the other hand, progressive disease shows the cancer is getting worse, even with treatment.
Knowing these terms helps manage patient hopes and make better treatment choices.
The Importance of Individualized Response Criteria
While standard categories help, individualized response criteria are key for real assessment. The type of cancer, the patient’s health, and past treatments all matter. They help decide if treatment is working well.
We use many methods to check treatment success. These include doctor checks, scans, and lab tests. This detailed approach helps make treatment plans that fit each patient best, improving life quality and outcomes.
- Treatment response is categorized into complete response, partial response, stable disease, and progressive disease.
- Complete and partial responses are considered positive outcomes, indicating effective treatment.
- Stable disease can be a positive outcome if cancer progression is halted.
- Progressive disease indicates that treatment is not effective, and alternative strategies may be needed.
- Individualized response criteria are essential for personalized patient care.
How to Know Chemo is Working: Key Indicators
When patients get chemotherapy, there are key signs that show if it’s working. Knowing these signs helps manage hopes and understand how the treatment is going.
Clinical Symptoms Improvement
One main sign that chemo is effective is when symptoms get better. Symptoms like pain, tiredness, and hard breathing really affect a patient’s life. When chemo works, these symptoms lessen, making daily tasks easier.
For example, a lung cancer patient might breathe better or cough less as the tumor gets smaller. Breast cancer patients might feel less pain in their bones.
Physical Examination Findings
Physical checks are key to seeing if chemo is working. Doctors look for changes in tumors or swollen lymph nodes. Seeing tumors shrink or lymph nodes disappear means chemo is effective.
| Physical Examination Findings | Indication of Chemotherapy Effectiveness |
| Decrease in tumor size | Positive response to chemotherapy |
| Disappearance of palpable lymph nodes | Effective treatment |
| Improvement in overall physical condition | Chemotherapy is working as intended |
Patient-Reported Outcomes
Patient feedback is now seen as very important in showing if chemo is working. These include how well a patient feels, how bad symptoms are, and overall happiness. When patients say they feel better, it’s a good sign chemo is helping.
For instance, a patient might say they can walk again or spend time with loved ones. These changes show chemo is doing its job.
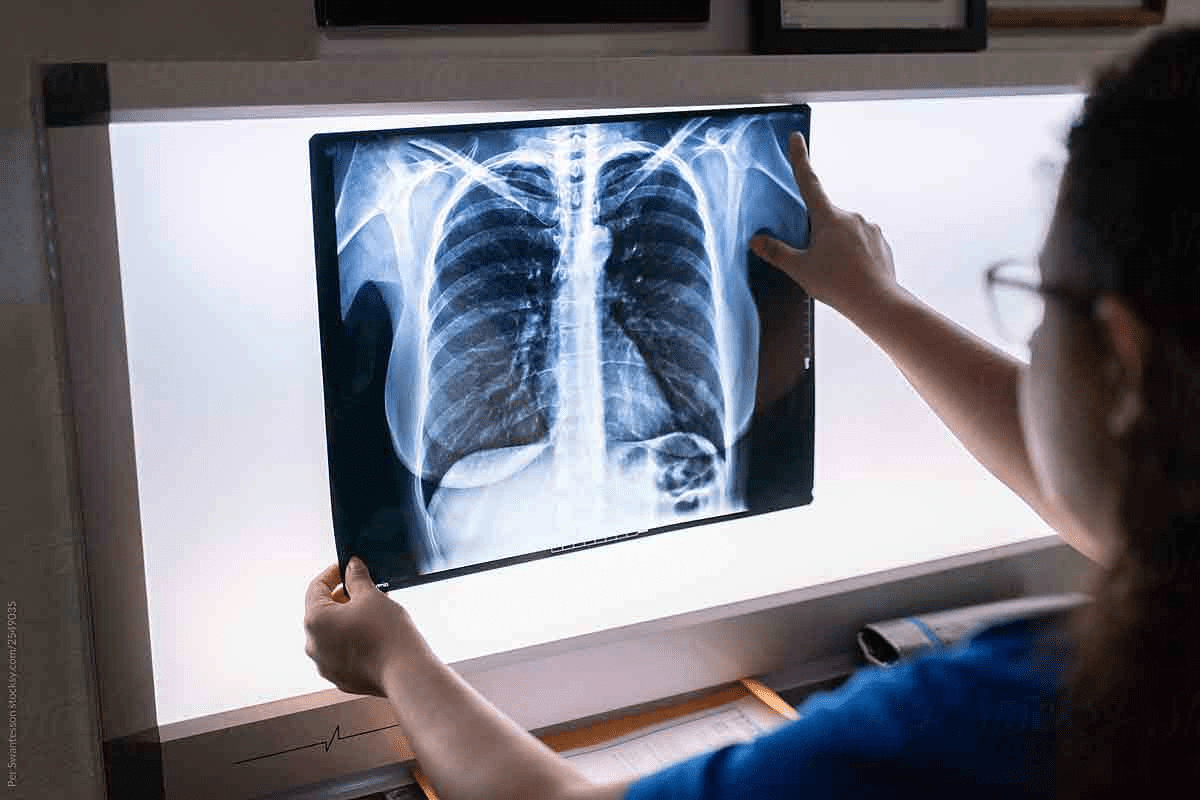
Medical Imaging: Visualizing Chemotherapy Response
Medical imaging is key in checking how well chemotherapy works. It uses different methods to see how tumors change. This helps doctors understand if treatment is working.
CT Scans and MRI Results Interpretation
Computed Tomography (CT) scans and Magnetic Resonance Imaging (MRI) are main tools for checking treatment results. CT scans show detailed body images, helping measure tumor size. MRI gives clear pictures of soft tissues, showing how tumors react to treatment.
Doctors look at CT and MRI results for size, density, and shape changes in tumors. If a tumor gets smaller or changes, it means chemotherapy is working.
PET Scans for Metabolic Response
Positron Emission Tomography (PET) scans show how active tumors are by looking at metabolism. They spot changes in glucose use in tumors, showing early signs of treatment success. A drop in metabolic activity often happens before size changes, making PET scans very useful.
Ultrasound and X-ray Findings
CT and MRI give detailed body images, but ultrasound and X-ray add more info. Ultrasound is great for looking at surface tumors or guiding biopsies. X-rays, though not as detailed, help track size changes or spot problems like fractures.
Using all these imaging methods together, doctors get a full picture of how cancer responds to chemotherapy. This helps them make better treatment plans.
Laboratory Tests That Measure Chemotherapy Effectiveness
Chemotherapy’s success can be checked through various lab tests. These tests give important insights into how well the treatment is working.
Tumor Markers and Their Significance
Tumor markers are substances made by cancer cells or in response to cancer. Blood tests can measure these markers. A drop in a specific marker level means the treatment is likely working.
Some common tumor markers include:
- CA-125 for ovarian cancer
- PSA for prostate cancer
- CEA for colorectal cancer
Tracking these markers over time helps understand how well the treatment is doing.
Blood Count Improvements
Blood counts are key in checking if chemotherapy is effective. An increase in white blood cells shows the treatment is helping to make blood cells again.
| Blood Component | Normal Range | Significance in Chemotherapy |
| White Blood Cells (WBC) | 4,500 – 11,000 cells/μL | An increase can indicate recovery from chemotherapy-induced neutropenia. |
| Red Blood Cells (RBC) | 4.32 – 5.72 million cells/μL | Stable or improving counts suggest effective management of anemia. |
| Platelets | 150,000 – 450,000 cells/μL | Normalization after chemotherapy indicates recovery of bone marrow function. |
Biochemical Indicators of Response
Biochemical tests check blood substances to see how organs are working and if chemotherapy is causing side effects. For example, liver tests can spot liver damage from chemotherapy.
“Biochemical indicators provide a window into the body’s response to chemotherapy, helping clinicians adjust treatment plans as needed.” – An Oncologist
These tests include:
- Liver function tests (e.g., ALT, AST)
- Kidney function tests (e.g., creatinine, urea)
- Electrolyte levels (e.g., sodium, potassium)
RECIST Criteria: The Standard for Measuring Tumor Response
RECIST guidelines in the context of assessing the effectiveness of chemotherapy.
Checking how tumors react to treatment is key in cancer care. The Response Evaluation Criteria in Solid Tumors (RECIST) is a widely used standard. It helps doctors and researchers see how well treatments work.
Understanding Target Lesions
The RECIST criteria focus on target lesions. These are specific tumors or lymph nodes measured at treatment start. Choosing the right target lesions is important for judging treatment success.
Doctors pick lesions that show the disease’s overall size and can be seen on scans. This makes sure the response to treatment is measured correctly.
Calculating Response Percentages
After picking target lesions, the next step is to calculate the treatment response. This means measuring the lesions at the start and later. The size of all target lesions is added up to see the overall response.
A complete response means all lesions are gone. A partial response is when the size of lesions drops by at least 30%. On the other hand, progressive disease is when lesions grow by at least 20%, or 5 mm if small. Stable disease means the size of lesions doesn’t change much.
Limitations of RECIST in Clinical Practice
Even though RECIST is very helpful, it has some limitations. It mainly looks at tumor size, missing other important details like how active the tumor is or its genetic makeup.
Using RECIST can be tricky, especially with tumors that are hard to measure. This shows the need for skilled doctors and radiologists to use RECIST correctly.
In summary, RECIST is a key tool in cancer care for checking how tumors respond to treatment. By understanding target lesions, calculating response percentages, and knowing RECIST’s limits, doctors can better care for their patients.
Timeframes: When to Expect Signs of Effective Chemotherapy
Knowing when chemotherapy starts to work is key for patients. Chemotherapy affects people in different ways. The time it takes for a response can vary a lot.
Early Response Indicators
Some signs of improvement can show up early, in the first few cycles. These might include less pain, better appetite, or fewer symptoms related to the tumor. We watch these signs closely because they suggest the treatment is working.
- Reduced pain levels
- Improved appetite
- Decreased tumor-related symptoms
Mid-Treatment Evaluation Points
After 2-3 months of treatment, we do a mid-treatment check-up. We use imaging like CT scans or MRI, and lab tests to see how well the treatment is doing. This helps us know if we need to make any changes.
Key evaluation methods include:
- Imaging studies (CT scans, MRI)
- Laboratory tests (tumor markers)
Long-Term Response Assessment
Looking at how well chemotherapy works over time is very important. We keep an eye on how the tumor responds, manage side effects, and adjust the treatment as needed. This ongoing assessment can last months to years, depending on the cancer and treatment goals.
By understanding these timeframes, patients can better plan their chemotherapy journey. They’ll know when to expect signs that the treatment is effective.
Cancer-Specific Response Patterns
Different cancers react differently to chemotherapy. This is because of their unique biology. Doctors need to understand these differences to choose the best treatments.
Solid Tumors vs. Hematological Malignancies
Solid tumors, like those in the breast, lung, and colon, need aggressive treatments. This is because of their size and location.
Hematological malignancies, like leukemia, respond better to chemotherapy. This is because they spread throughout the body, making systemic treatment more effective.
Breast Cancer Response Patterns
Breast cancer’s reaction to chemotherapy depends on its type and stage. For example, HER2-positive cancers often do well with targeted treatments and chemotherapy.
Lung Cancer Response Characteristics
Lung cancer, especially non-small cell lung cancer (NSCLC), shows varied responses to chemotherapy. Some patients see significant tumor shrinkage. Immunotherapy has also helped some patients.
Colorectal Cancer Response Indicators
Colorectal cancer’s response to chemotherapy is measured by tumor size and CEA levels. New chemotherapy combinations have improved survival rates in advanced cases.
| Cancer Type | Common Chemotherapy Response Patterns | Key Indicators of Response |
| Breast Cancer | Varies by subtype; HER2-positive responds well to targeted therapy | Tumor shrinkage, improvement in symptoms |
| Lung Cancer (NSCLC) | Variable response; improved with immunotherapy in some patients | Tumor size reduction, improved lung function |
| Colorectal Cancer | Response seen in tumor size and CEA levels | Decrease in CEA levels, tumor shrinkage |
| Hematological Malignancies | Generally responsive to chemotherapy | Normalization of blood counts, reduction in lymphadenopathy |
Positive Response to Chemotherapy: Physical and Symptomatic Changes
Chemotherapy can lead to many positive changes. These include better pain management, increased energy, improved appetite, and enhanced daily functioning. When it works well, it greatly improves a patient’s quality of life.
Pain Reduction and Management
Pain reduction is a key sign of chemotherapy success. As treatment progresses, patients often feel less pain. This makes it easier to manage their condition and do daily tasks.
Energy Level Improvements
Chemotherapy can also boost energy levels. Patients may start doing things they couldn’t before because of tiredness. This energy boost is vital for a better quality of life.
Appetite and Weight Stabilization
Another sign of success is stabilizing appetite and weight. Patients might eat more, helping them keep a healthy weight. This is important for staying strong and recovering from treatment.
Improved Functional Status
Effective chemotherapy leads to an improvement in functional status. Patients can do daily tasks more easily and independently. This shows the treatment is working well and improves their life quality.
These changes are important signs that chemotherapy is effective. By watching for these improvements, doctors can see how well the treatment is going. This helps them make the best decisions for ongoing care.
When Chemotherapy Isn’t Working: Recognizing Treatment Failure
When chemotherapy doesn’t work as expected, it’s key to know the signs of treatment failure. Chemotherapy is a main part of cancer treatment. But, its success depends on many things like the cancer type, disease stage, and patient characteristics. Spotting when chemotherapy isn’t working is vital for choosing other treatments and dealing with the emotional side of failure.
Signs of Disease Progression
Disease progression shows chemotherapy isn’t working. This can be seen as tumors growing, new tumors forming, or cancer spreading. Symptoms like pain, tiredness, and weight loss can get worse too. Tests like CT scans and MRIs, along with doctor checks, help spot these changes.
When to Consider Alternative Treatments
When disease progression is confirmed, doctors talk about other treatment options. These might include trying a different chemotherapy, adding targeted therapy or immunotherapy, or focusing on symptom relief. The right choice depends on the patient’s health, past treatments, and cancer details.
The Emotional Impact of Treatment Failure
Treatment failure can deeply affect patients and their families. They might feel disappointed, anxious, or scared. Healthcare providers should offer emotional support and counseling. Family, friends, and support groups are also important in getting through this tough time.
How Doctors Evaluate and Communicate Treatment Response
Doctors use a detailed method to check how well a patient is doing with chemotherapy. They look at many things and work with different teams to make sure they get it right.
The Multidisciplinary Tumor Board Approach
A team of doctors from different fields comes together to talk about patient cases. This team includes oncologists, radiologists, surgeons, and pathologists.
This team looks at images, lab results, and other info to see how well the treatment is working. Working together helps them consider all parts of a patient’s health.
| Specialty | Role in Treatment Response Evaluation |
| Oncologist | Assesses overall treatment response and adjusts chemotherapy plans |
| Radiologist | Interprets imaging studies to evaluate tumor response |
| Pathologist | Examines tissue samples to assess tumor characteristics and response |
Discussing Scan Results with Patients
Doctors try to explain scan results in a way that’s easy to understand. They talk about what the results mean for treatment and answer any questions.
Good communication helps patients understand their treatment progress.
Shared Decision-Making in Treatment Adjustments
Doctors and patients work together to decide on treatment changes. They talk about the good and bad of different options and what the patient wants.
This teamwork helps make sure treatment plans fit the patient’s needs. It’s all about making choices together.
- Patients are actively involved in decision-making processes
- Healthcare providers offer expert guidance and recommendations
- Treatment plans are adjusted based on ongoing evaluation and patient feedback
Beyond Tumor Shrinkage: Modern Concepts of Treatment Benefit
We now see that chemotherapy’s success goes beyond just shrinking tumors. It also boosts quality of life, extends survival, and improves how well patients can function. This new view of treatment benefits shows how complex cancer is and its big impact on patients.
Quality of Life Improvements
Improving a patient’s quality of life is a big win. Good chemotherapy can cut down on pain, nausea, and tiredness. This lets patients get back to their daily lives and feel better overall. Quality of life improvements are now key in judging how well cancer treatment works.
Progression-Free Survival
Progression-free survival (PFS) is another important measure. It’s the time a patient lives with the disease without it getting worse. PFS shows how well chemotherapy keeps the disease in check.
| Treatment Outcome | Description | Clinical Significance |
| Progression-Free Survival | Time during and after treatment that the disease does not worsen | Indicates control of the disease |
| Overall Survival | Length of time from diagnosis or treatment start that a patient is still alive | Reflects the ultimate goal of treatment: extending life |
| Quality of Life | Patient’s ability to maintain daily activities and well-being | Essential for patient-centered care |
Overall Survival Benefits
Overall survival (OS) is the most clear sign of treatment success. It’s how long a patient lives after being diagnosed or starting treatment. Better chemotherapy has helped many cancers last longer.
Functional Status and Independence Gains
Chemotherapy can also make patients more functional. This means they can keep doing their daily tasks and stay independent. This is very important for their mental and social health.
In summary, chemotherapy’s benefits are more than just shrinking tumors. They include better quality of life, longer survival, and more independence. These modern views of treatment benefit show how cancer care is getting more comprehensive.
Emerging Technologies in Chemotherapy Response Assessment
New technologies are changing how we check if chemotherapy is working. These changes are making treatment more precise and personal for patients.
Liquid Biopsies and Circulating Tumor DNA
Liquid biopsies are a big step forward in fighting cancer. They let doctors check for cancer mutations in blood. This is a safer way than old tissue biopsies.
“Liquid biopsies are revolutionizing the way we monitor cancer treatment, providing a window into the tumor’s genetic makeup without the need for invasive procedures.”
They’re great for patients with hard-to-reach tumors. Studies show they can predict how well treatment will work. This helps doctors adjust plans quickly.
Artificial Intelligence in Imaging Analysis
Artificial intelligence (AI) is making medical images better. AI looks at scans to spot changes in tumors that humans might miss.
AI helps doctors see how well treatment is working sooner. This means they can change plans faster, helping patients more.
- Enhanced accuracy in tumor measurement
- Faster analysis of imaging data
- Improved detection of subtle changes in tumor characteristics
Molecular and Genetic Response Markers
Discovering new markers is a big deal in fighting cancer. These markers tell doctors how a tumor might react to certain treatments.
For instance, some genetic changes show if a tumor will respond well to certain drugs. This lets doctors tailor treatments to fit each patient’s cancer better.
“The integration of molecular and genetic markers into treatment planning represents a crucial step towards personalized medicine in oncology.”
As we learn more about these markers, we can make treatments even more targeted. This means better chances of beating cancer.
Psychological Aspects of Treatment Response
It’s key to understand the emotional and psychological sides of treatment response. When patients get chemotherapy, how they feel mentally is very important. It affects their whole treatment journey.
Managing Expectations During Treatment
It’s vital to manage what patients expect during chemotherapy. They should know what to expect at each step, like side effects and how well they might respond. Clear communication from healthcare providers helps set realistic hopes. This lowers anxiety and uncertainty.
Here are some key aspects to consider when managing expectations:
- Understanding the treatment plan and its goals
- Being aware of potential side effects and how to manage them
- Knowing the criteria for assessing treatment response
- Having a support system in place for emotional support
Coping with Scan Anxiety
Scan anxiety is common in cancer patients getting chemotherapy. Waiting for scan results can be very stressful. Techniques such as mindfulness, meditation, and cognitive-behavioral therapy can help manage this anxiety.
Some strategies for coping with scan anxiety include:
- Preparing oneself for the possibility of different outcomes
- Engaging in relaxation techniques before and after scans
- Seeking support from family, friends, or support groups
The Impact of Response on Mental Health
The way chemotherapy works can deeply affect a patient’s mental health. A good response can lift spirits and lower anxiety. But a bad response can make patients feel down and hopeless. Monitoring mental health and offering the right support is very important during this time.
Family Support During Response Assessment
Family support is crucial for patients dealing with the mental side of treatment response. Emotional support from family members helps patients face the challenges of chemotherapy and its results.
Some ways family members can support include:
- Being present during doctor’s appointments
- Helping with daily tasks and responsibilities
- Encouraging patients to share their feelings and worries
Conclusion: Navigating the Chemotherapy Response Journey
Understanding how well chemotherapy works is complex. We’ve looked at many factors, like how symptoms change and what tests show. We’ve also talked about how patients feel and what they say about their treatment.
Different cancers react in unique ways to chemotherapy. New technologies help us see how well treatments are working. The mind also plays a big part, as dealing with anxiety and hopes can affect a patient’s mental state.
Knowing all these things helps doctors and patients make better choices. As we keep improving in cancer care, staying up-to-date is key. This way, we can help patients live better and longer lives.
FAQ
What is considered a good response to chemotherapy?
A good response to chemotherapy means a big drop in tumor size or the tumor disappearing. It also means feeling better and enjoying life more.
How do doctors measure the effectiveness of chemotherapy?
Doctors check how well chemotherapy works in many ways. They use CT scans, MRI, and PET scans. They also look at blood tests and tumor markers.
What are the different categories of treatment response?
Treatment response is divided into a few main categories. These are complete response, partial response, stable disease, and progressive disease. Each shows how well the treatment is working.
How long does it take to see the effects of chemotherapy?
The time it takes to see chemotherapy’s effects varies. It depends on the cancer type, treatment, and the patient. But, you might start seeing changes in a few weeks to months.
What are the signs that chemotherapy is working?
Signs that chemotherapy is working include feeling better. This means less pain, more energy, better appetite, and being able to do more. You might also see the tumor getting smaller or disappearing on scans.
How do different types of cancer respond to chemotherapy?
Each type of cancer reacts differently to chemotherapy. Some cancers, like blood cancers, respond quickly. Others, like solid tumors, might take longer.
What is the role of medical imaging in evaluating chemotherapy response?
Medical imaging is key in checking how well chemotherapy is working. It shows if the tumor is getting smaller or growing. This helps doctors make the right treatment changes.
How do laboratory tests contribute to understanding treatment response?
Laboratory tests give important clues about how well treatment is working. They check for changes in tumor activity and overall health.
What are the RECIST criteria, and how are they used?
The RECIST criteria are a set of rules for measuring how well a tumor responds to treatment. They help doctors see if the treatment is working by looking at changes in tumor size.
How do doctors communicate treatment response to patients?
Doctors talk about treatment response in a team effort. They discuss scan results, treatment options, and make changes as needed. They also listen to patient concerns and preferences.
What are the emerging technologies in chemotherapy response assessment?
New technologies like liquid biopsies, AI in imaging, and genetic markers are changing how we check chemotherapy response. They help make treatment more precise and personal.
How can patients cope with scan anxiety and manage expectations during treatment?
Patients can deal with scan anxiety and manage expectations by staying informed. They should talk openly with their healthcare team. Getting support from family and mental health professionals also helps.
References
- American Cancer Society. (2025). How Chemotherapy Drugs Work. https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/chemotherapy/how-chemotherapy-drugs-work.html
- Coyne, E. (2019). Current evidence of education and safety requirements for nursing administration of chemotherapy: An integrative review. European Journal of Oncology Nursing, 43, 101680. https://pubmed.ncbi.nlm.nih.gov/31358254/