Last Updated on November 27, 2025 by Bilal Hasdemir
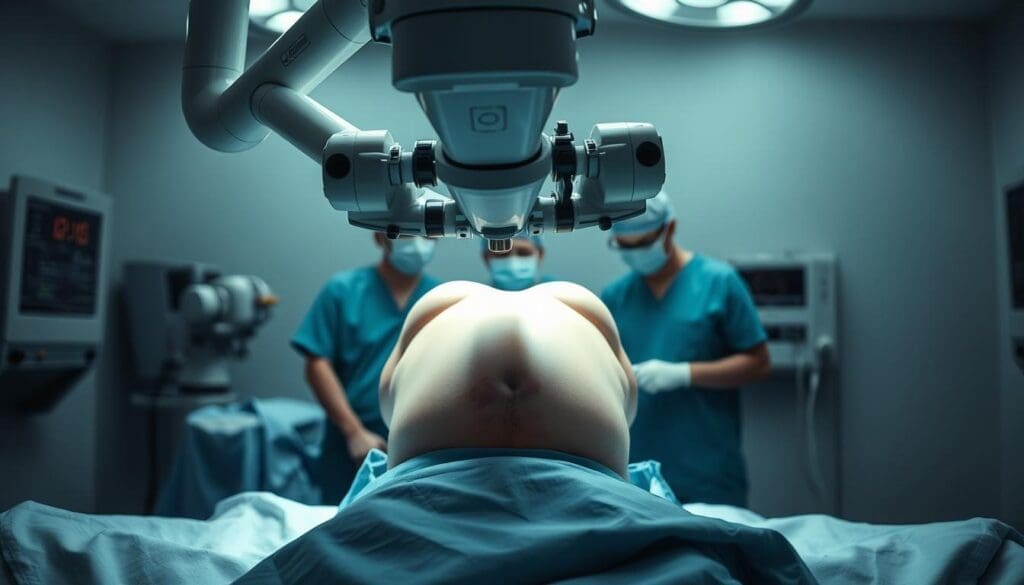
At Liv Hospital, we utilise cutting-edge robotic technology to deliver world-class minimally invasive hysterectomy care. In this guide, we walk you through how a robotic hysterectomy is performed—step by step—and what to expect during recovery.
We are dedicated to top-notch healthcare for international patients. A minimally invasive procedure like robotic hysterectomy is a big step forward in gynecology. It gives patients a quicker recovery and less pain.

Robotic hysterectomy uses laparoscopic surgery with a computer to control tools. This means the surgeon can work with great precision. It’s a way to offer expert care and focus on making sure patients recover well.
Robotic hysterectomy is a new way to remove the uterus using advanced technology. It’s a less invasive option compared to traditional surgery. This method has changed gynecological surgery for the better.
A robotic hysterectomy uses a robotic system for precise surgery. The surgeon sits at a console and controls the robotic arms. These arms do the actual surgery.
This surgery uses advanced tech to improve results. The robotic system gives a 3D view of the area. This helps the surgeon remove the uterus more accurately.
Robotic systems make surgery more precise in many ways. They allow for very small movements, which lowers the risk of mistakes. The 3D view helps surgeons see better and avoid damaging important areas.
Key features of robotic systems that enhance precision include:
| Feature | Benefit |
| 3D Visualization | Enhanced clarity and accuracy |
| Robotic Arms | Precise movements and reduced tremors |
| Ergonomic Design | Reduced surgeon fatigue and improved focus |
Minimally invasive gynecological surgery has come a long way. It started with traditional laparoscopic surgery and now includes robotic-assisted procedures. Robotic hysterectomy is the latest step, improving precision and recovery times.
As medical technology keeps improving, robotic hysterectomy will play a bigger role in gynecological surgery. It will offer safer and more effective treatments for patients.
It’s important for patients to know about the types of robotic hysterectomy procedures. These procedures have evolved to meet different patient needs. Each technique is designed for specific conditions.
Robotic Total Laparoscopic Hysterectomy is a minimally invasive surgery. The surgeon uses a robotic system to remove the uterus through small incisions. This method offers better precision and control, making it more detailed.
Robotic Assisted Total Laparoscopic Hysterectomy uses a robotic system to help the surgeon. The surgeon controls the robotic arms, combining robotic precision with their skill.
The main difference between Robotic Total Laparoscopic Hysterectomy and Robotic Assisted Total Laparoscopic Hysterectomy is the level of robotic involvement. Both are minimally invasive and use robotic technology. But, the total laparoscopic approach uses more robotic tools.
The choice between Robotic Total Laparoscopic Hysterectomy and Robotic Assisted Total Laparoscopic Hysterectomy depends on several factors. These include the patient’s medical history and the complexity of the case. The surgeon’s judgment also plays a role. Robotic Total Laparoscopic Hysterectomy is often chosen for precise dissections. Robotic Assisted Total Laparoscopic Hysterectomy is preferred when both robotic precision and surgeon skill are needed.
It’s important to know the differences between robotic hysterectomy and other surgeries. There are many ways to do a hysterectomy, each with its own good and bad points.
Traditional open hysterectomy uses a big cut in the belly to get to the uterus. Robotic hysterectomy, on the other hand, uses small cuts and a robotic system for the surgery. The robotic method leads to less blood loss, lower infection risk, and faster healing than open surgery.
Laparoscopic hysterectomy uses a thin, lighted tube with a camera to do the surgery through small cuts. The robotic-assisted version adds a robotic system for better precision and flexibility. This robotic system makes it easier to do detailed work, which can lower the chance of problems.
Vaginal hysterectomy removes the uterus through the vagina, without any cuts outside. It’s less invasive but might not work for everyone, like those with big uteruses or certain health issues. Robotic hysterectomy is more flexible and offers a less invasive way with better views.
Choosing a surgery depends on many things, like the patient’s health, why they need the surgery, and the surgeon’s skill. Things like past surgeries or adhesions can also play a part. A doctor’s careful look at each patient is key to picking the best surgery.
| Surgical Approach | Incision Size | Recovery Time | Blood Loss |
| Robotic Hysterectomy | Several small incisions | Typically 1-2 weeks | Minimal |
| Traditional Open Hysterectomy | One large incision | 6-8 weeks | Significant |
| Laparoscopic Hysterectomy | Several small incisions | 2-4 weeks | Moderate |
| Vaginal Hysterectomy | No external incisions | 1-2 weeks | Minimal |
Choosing the right patients for robotic hysterectomy is key for a good outcome. We carefully check each patient to see if they’re a good fit for this advanced surgery.
Good candidates for robotic hysterectomy often have issues like uterine fibroids or endometriosis. Robotic surgery is great for those needing precise work and have complex anatomy.
Before robotic hysterectomy, patients get a lot of tests. This includes blood tests, ultrasound or MRI, and sometimes a biopsy. These tests help confirm the diagnosis and check how bad the condition is.
Some health issues can make a patient not eligible for robotic hysterectomy. These include severe heart or lung problems, or a lot of adhesions from past surgeries. We do a detailed medical check to spot any risks.
Talking openly with patients about what to expect from robotic hysterectomy is vital. We tell them about the benefits and risks. This way, they know what to expect during recovery and the surgery’s results.
Getting ready for robotic hysterectomy surgery is key for a smooth process. We know being prepared can make a big difference in your experience and recovery.
We’ll give you specific instructions before your surgery. You might need to arrive at the hospital early, wear loose clothes, and remove jewelry or contacts.
It’s very important to follow these steps to keep you safe and ensure the surgery goes well.
You’ll get advice on what to eat and what meds to skip before surgery. We want you to eat well to help your body heal faster. Some meds, like blood thinners, might need to be stopped a few days before.
| Medication | Action Required | Days Before Surgery |
| Blood Thinners | Discontinue | 5-7 days |
| Anti-inflammatory | Consult Doctor | 2-3 days |
| Antibiotics | Follow Doctor’s Instructions | As directed |
On surgery day, bring your insurance cards, ID, and a list of your meds and medical history. Also, bring comfy clothes and things like your phone charger and a book to make your stay better.
Mental prep is as important as physical prep. Try relaxation methods like deep breathing or meditation to calm your nerves before surgery. Having a loved one with you can also offer emotional support.
Robotic-assisted hysterectomy is a detailed process. It involves several steps to ensure success. We will walk you through the main stages of this advanced surgery.
The first step is to position the patient. They are placed in a lithotomy position for better access to the pelvic area. This position helps keep the patient stable during surgery.
Then, a small incision is made in the umbilical region. This incision is where the laparoscope goes. It gives us a clear view of the internal organs.

After initial access, we place trocars. These are special ports for the robotic instruments. The right placement of trocars is key for the surgery’s success.
We use landmarks and imaging to place the trocars accurately.
Next, we dock the robotic system. We align the robotic arms with the trocars. This prepares the instruments for the surgery.
The robotic system offers better dexterity and precision. It helps with detailed dissection and tissue manipulation.
The surgical dissection is a vital part of the procedure. We use robotic instruments to carefully separate the uterus from surrounding tissues.
This step needs precision. The robotic system’s high-definition view and design help a lot.
We will explore how long a robotic hysterectomy typically takes and what influences this duration. The length of time required for this surgical procedure is a common concern among patients.
The average duration of a robotic hysterectomy is between 1 to 3 hours. This timeframe can vary based on the complexity of the case and the surgeon’s experience. Generally, robotic hysterectomy procedures are known for their efficiency compared to traditional open hysterectomies.
Several factors can influence the duration of a robotic hysterectomy. These include:
Understanding these factors can help manage patient expectations and improve the overall surgical experience.
Robotic hysterectomy typically offers a shorter recovery time compared to traditional open hysterectomy. While the surgical time may be comparable or slightly longer, the overall benefits of a robotic approach often outweigh the slightly extended surgical duration. The reduced blood loss, less post-operative pain, and quicker return to normal activities make robotic hysterectomy an attractive option for many patients.
In conclusion, while the duration of a robotic hysterectomy can vary, understanding the factors that influence surgical time can help patients prepare for their procedure. By choosing an experienced surgeon and being aware of the possible complexities, patients can optimize their surgical experience.
Robotic hysterectomy has changed gynecological surgery a lot. It brings many benefits to patients. The way this surgery is done has improved a lot, making it better for women.
One big plus of robotic hysterectomy is less blood loss. The robotic system’s precision and clear view help avoid damage to tissues. This makes the surgery safer.
People who have robotic hysterectomy usually stay in the hospital less. This is because the surgery is less invasive. It causes less damage and trauma.
The robotic system makes surgery more precise. It’s great for tricky cases where careful work is needed. This reduces the chance of problems.
Robotic hysterectomy helps patients recover faster. They can get back to their daily life sooner. This is a big plus for those who need to get back to their routine.
| Benefits | Robotic Hysterectomy | Traditional Open Hysterectomy |
| Blood Loss | Reduced | Significant |
| Hospital Stay | Shorter (1-2 days) | Longer (3-5 days) |
| Surgical Precision | Enhanced | Limited |
| Recovery Time | Faster (2-4 weeks) | Slower (6-8 weeks) |
In summary, robotic hysterectomy is a good choice for many women. It leads to less blood loss, shorter hospital stays, better surgery, and quicker recovery. These benefits make the experience much better for patients.
It’s important for patients to know about the side effects of robotic hysterectomy. This surgery is less invasive but can have risks and complications.
Patients may face several symptoms after robotic hysterectomy. These include:
These symptoms are usually short-term and can be managed with proper care. Effective pain management is key, and our team will help you manage these symptoms.
Though rare, serious complications can occur. These include:
It’s vital for patients to know about these risks. They should promptly report any concerning symptoms to their healthcare provider.
Seek immediate medical help if you experience:
Knowing about these side effects and complications helps patients prepare. Our medical team is dedicated to providing the best care and support during recovery.
Recovering from a robotic hysterectomy is a journey with many steps. We help our patients understand each step. This way, they know what to expect and how to recover well.
Right after surgery, patients start their recovery in the hospital. Typically, hospital stays range from 1 to 2 days. Our team manages pain and watches for complications. They also give initial care instructions.
The first week is key for a smooth recovery. Patients should rest, avoid heavy lifting, and eat well. Gentle walking is also recommended to prevent blood clots. Pain is managed with medication.
In weeks 2-6, patients can start doing more. Light exercise and stretching are okay, but no heavy lifting. Regular check-ups with our team are important to track healing.
Recovery from a robotic hysterectomy takes time. Most women can get back to normal in 4 to 6 weeks. But, complete healing of internal tissues may take longer. We offer personalized support to help with the recovery.
| Recovery Stage | Timeline | Key Activities |
| Immediate Post-Operative | 1-2 days | Rest, pain management |
| First Week | 1 week | Gentle walking, balanced diet |
| Weeks 2-6 | 2-6 weeks | Light exercise, stretching |
| Long-Term | 4-6 weeks+ | Return to normal activities, full healing |
The recovery after a robotic hysterectomy is key. Knowing what to expect can make it easier. We’ll cover the physical, emotional, and practical sides of your recovery.
Patients may feel mild discomfort, bloating, and fatigue after a robotic hysterectomy. Resting well and following our instructions can help manage these feelings.
Common physical changes include:
Emotional and hormonal changes after a hysterectomy are big. Hormone level changes can affect mood. Our support team is here to help you through this.
Some people may feel:
Talking to your healthcare provider about these changes is important.
Following activity restrictions is key for a smooth recovery. These rules help avoid complications and aid in healing.
| Activity | Recommended Restriction Period |
| Heavy lifting | 4-6 weeks |
| Bending or straining | 4-6 weeks |
| Driving | 1-2 weeks |
| Returning to work | 2-4 weeks |
When you can go back to work depends on your job and how you’re feeling. Usually, it’s best to take 2-4 weeks off to rest and recover.
Listen to your body and don’t rush back to work too soon. Your health is our main concern.
Knowing what to expect after a robotic hysterectomy helps you navigate your recovery. If you have questions or concerns, reach out to your healthcare provider.
We’ve looked into robotic hysterectomy, a new surgery method. It brings many benefits to those needing a hysterectomy. Surgeons use advanced robots for better precision, less blood loss, and shorter stays in the hospital.
This surgery has many perks. Patients recover faster, feel less pain, and have less scarring. We talked about the different types of robotic hysterectomies, who can get them, and how the surgery is done.
Knowing how to recover from robotic hysterectomy is key. We covered the usual recovery time, possible side effects, and care tips. This helps patients prepare and get the best results.
In summary, robotic hysterectomy is a great choice for many. It’s a less invasive way to get the surgery done. Choosing a good surgeon and hospital can make the recovery smoother and more comfortable.
A robotic hysterectomy is a surgery to remove the uterus. It uses a robotic system for more precision and flexibility.
A robotic hysterectomy usually takes one to three hours. The time can vary based on the case’s complexity and the patient’s health.
Robotic hysterectomy has many benefits. It reduces blood loss, shortens hospital stays, and allows for quicker recovery. It also offers better surgical precision.
Side effects include pain, vaginal bleeding, and mild discomfort. Serious but rare complications can happen. Seek medical help for severe symptoms.
To prepare, follow dietary and medication guidelines. Bring necessary items to the hospital. Mental preparation is also key for a smooth surgery.
Expect a hospital stay followed by recovery at home. The process involves physical, emotional, and practical adjustments. Follow activity restrictions and return-to-work guidelines.
Robotic hysterectomy is less invasive than traditional open hysterectomy. It offers less blood loss and faster recovery. The choice depends on the patient’s condition and the surgeon’s judgment.
Both are robotic hysterectomy types. The difference is in robotic assistance levels. Robotic total laparoscopic is fully robotic, while robotic assisted combines robotic and laparoscopic techniques.
Robotic hysterectomy is recommended for certain gynecological conditions. The decision is based on the patient’s health, medical history, and the surgeon’s judgment.
“Robotic Hysterectomy for Benign Indications” — https://pmc.ncbi.nlm.nih.gov/articles/PMC8035818/ PMC
“Current Role of Robotic Hysterectomy” — https://pmc.ncbi.nlm.nih.gov/articles/PMC3827863/ PMC
“Robot-Assisted Surgery for Noncancerous Gynecologic Conditions” — https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2020/09/robot-assisted-surgery-for-noncancerous-gynecologic-conditions ACOG
“The Benefits and Challenges of Robotic-Assisted Hysterectomy” — https://journals.lww.com/co-obgyn/FullText/2014/08000/The_benefits_and_challenges_of_robotic_assisted.11.aspx Lippincott Journals
“Approaches for Hysterectomy and Implementation of Robot-Assisted Hysterectomy” — https://www.sciencedirect.com/science/article/abs/pii/S0301211524004159 ScienceDirect
“Da Vinci Surgical System” (overview of robotic surgery system) — https://en.wikipedia.org/wiki/Da_Vinci_Surgical_System Wikipedia
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!