Last Updated on November 26, 2025 by Bilal Hasdemir
At Liv Hospital, we know how tough it is to deal with brain tumor removal. Our team is full of experts ready to help. They use the latest and safest ways to remove tumors, like open craniotomy and radiosurgery.
We’re all about new ideas and caring for our patients. We help patients and their families find new ways to fight neurosurgery for brain tumors. Our top-notch care and trusted team make sure every patient gets the best treatment.
Key Takeaways
- Advanced surgical methods for brain tumor removal
- Minimally invasive techniques for reduced recovery time
- Radiosurgery as a precise treatment option
- Personalized care for each patient
- State-of-the-art protocols for optimal outcomes
Understanding Brain Tumors and Their Impact
It’s important to know about brain tumors for good treatment plans. These are abnormal growths in the brain, either benign or malignant. We’ll look at the different types and how they affect patients.
Types of Brain Tumors: Benign vs. Malignant
Brain tumors fall into two main types: benign and malignant. Benign brain tumors are not cancerous and don’t spread. But, they can cause problems because of their size and where they are. Malignant brain tumors, being cancerous, can spread and are more dangerous.
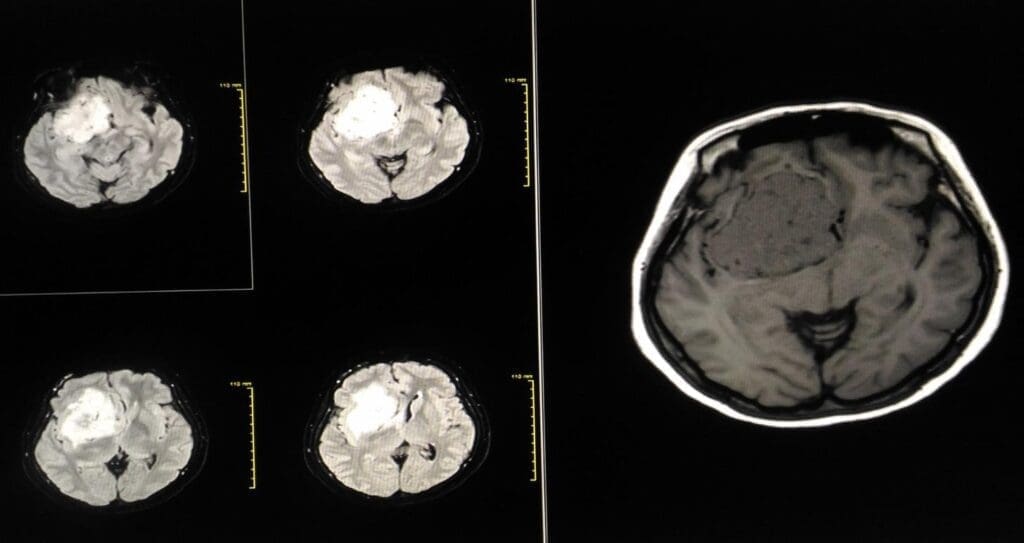
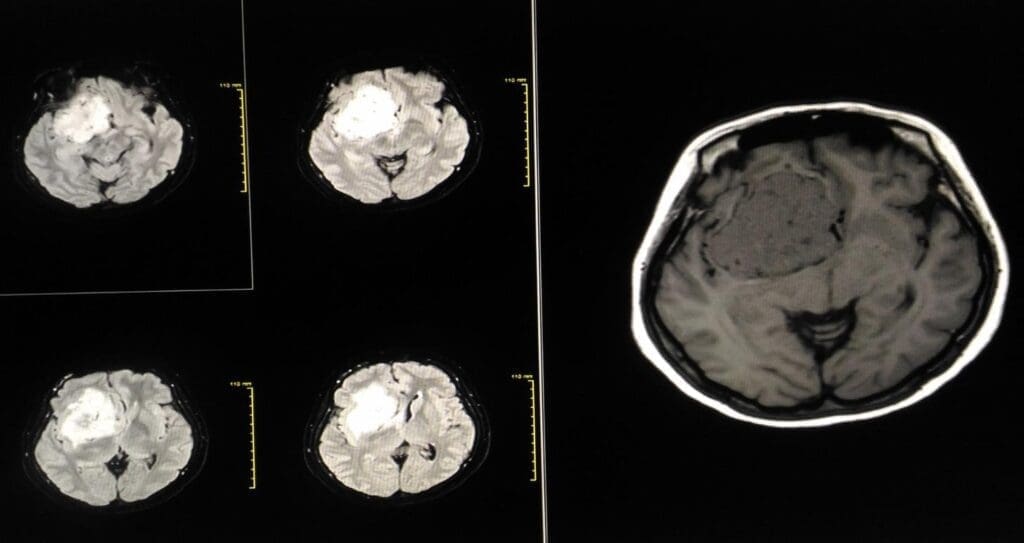
Symptoms of brain tumors depend on their location, size, and type. Common signs include headaches, seizures, nausea, and weakness or numbness in limbs. Doctors use MRI and CT scans, along with neurological exams, to diagnose.
A leading neurosurgeon said,
“Early diagnosis is critical in managing brain tumors effectively. Advanced imaging techniques have significantly improved our ability to detect and treat these tumors.”
| Symptom | Description | Possible Tumor Location |
| Headaches | Persistent and often severe | Various, depending on tumor size and location |
| Seizures | Can be focal or generalized | Often in areas controlling motor functions |
| Numbness or Weakness | Typically affects one side of the body | Motor cortex or nearby areas |
Knowing about brain tumors helps both patients and doctors make better treatment choices.
When Surgical Intervention Becomes Necessary
When a brain tumor is diagnosed, deciding if surgery is needed is key. This choice depends on the tumor’s type, size, and where it is. It also looks at the patient’s health overall.
Indications for Brain Tumor Removal
Surgery is often suggested for brain tumors that cause big symptoms or might grow and harm more. Key signs for surgery include:
- Tumors that raise pressure inside the skull
- Lesions near important brain parts
- Tumors that cause brain function problems
- Suspected cancer that needs tissue check
These signs are checked to see if surgery is the best option.
Risk Assessment for Surgery
Before surgery, a detailed risk check is done. This looks at the patient’s health history, current health, and the tumor’s details. Risks of brain tumor surgery include:
- Infection
- Bleeding
- Damage to brain function
- Reaction to anesthesia
Our neurosurgery team talks with the patient about these risks. They work to lessen them.
Consultation with Neurosurgical Team
Talking with a neurosurgery team is a big step in deciding on surgery. Our experts do a full check, talk about surgery’s pros and cons, and answer questions. This is a chance for patients to:
- Get a clear view of their diagnosis and options
- Share their worries and hopes
- Learn about the surgery and recovery
By teaming up with our neurosurgery team, patients can make smart choices about their care.
The aim of surgery for brain tumors is to better the patient’s life and health. By carefully looking at the need for surgery and working with a skilled team, patients get top care for their condition.
Preoperative Planning and Patient Preparation
The journey to successful brain tumor surgery starts with detailed preoperative planning. This important step makes sure we, as a medical team, are ready to give our best care to patients.
Advanced Imaging for Surgical Mapping
Advanced imaging is key for surgical mapping. It lets us see the tumor and brain structures clearly. MRI and CT scans help us understand the tumor’s size and where it is in the brain.
A leading neurosurgeon says, “Advanced imaging is not just for diagnosis; it’s a guide for surgery.” This shows how vital accurate imaging is for planning the surgery.
“The use of advanced imaging techniques has changed neurosurgery, making surgeries more precise and safer.”
Medical Optimization Before Surgery
Before surgery, we work to improve the patient’s health to lower risks. We manage chronic conditions like hypertension and diabetes. We also stop certain medications that could affect surgery or anesthesia.
| Medical Condition | Optimization Strategy |
| Hypertension | Medication adjustment, lifestyle changes |
| Diabetes | Blood glucose monitoring, medication adjustment |
Patient Education and Expectation Management
Telling patients about the surgery, risks, and what to expect is key. We explain the procedure in detail. This ensures patients have realistic hopes and are ready for recovery.
- Clear explanation of the surgical procedure
- Discussion of possible risks and complications
- Info on what to expect during recovery
By focusing on preoperative planning, we can greatly improve surgery results and patient happiness. Our thorough preparation shows our commitment to top-notch healthcare.
Modern Brain Tumor Surgery Approaches
Medical technology has changed brain tumor surgery a lot. Now, we have many ways to treat each patient differently. We’ve learned a lot about brain tumors and how to remove them safely.
“Choosing the right surgery is key for good results,” says a top neurosurgeon. “The right method helps us remove tumors well and protect the brain.”
Open Craniotomy Procedure
Open craniotomy is a main way to treat brain tumors. It means taking part of the skull off to get to the tumor. This method lets us see and work on the tumor directly, which is good for big or hard-to-reach tumors.
We use new imaging tools during this surgery to find the tumor right and avoid harming other brain parts. We also use monitoring during surgery to make it safer and more effective.
Minimally Invasive Techniques
There are also new, less invasive ways to treat brain tumors. These methods use smaller cuts and disturb the brain less. They can mean quicker recovery times and fewer complications.
We use different minimally invasive methods, like endoscopic and keyhole surgeries, for many brain tumors. These need special skills and tools but are great for the right patients.
Choosing the Right Surgical Approach
Choosing the best surgery for a brain tumor patient is complex. We look at the tumor’s size, where it is, and what it’s like. We also think about the patient’s health and what they want.
- Tumor-specific factors, such as its proximity to critical brain structures
- Patient factors, including age, overall health, and previous treatments
- Surgeon expertise and institutional capabilities
By looking at all these things, we pick the best surgery for each person. This helps them have the best chance of a good outcome.
Minimally Invasive Endoscopic Techniques
Minimally invasive endoscopic techniques have changed brain tumor surgery. They make treatments safer and more effective. These methods allow us to do complex surgeries with more precision. This reduces risks and helps patients recover faster.
Endoscopic Endonasal Approach
The endoscopic endonasal approach removes brain tumors through the nose. It avoids the need for big cuts on the outside. This cuts down on trauma and pain after surgery.
We use top-notch endoscopic tools and systems. They help us remove tumors accurately while keeping important areas safe.
Keyhole Craniotomy Methods
Keyhole craniotomy makes a small hole in the skull to reach the tumor. It causes less damage and helps the body heal faster. We use advanced imaging and tools to find the tumor and plan the best way to remove it.
Benefits and Limitations
These techniques have many benefits. They lead to quicker recovery, less pain, and better looks. But, they also need special training and tools. We choose the best method for each patient, considering the good and bad sides.
Using these techniques, we offer our patients the latest in care. As technology grows, we keep up to give our patients the best treatment.
Stereotactic Radiosurgery for Brain Tumors
Stereotactic radiosurgery is a key tool in fighting brain tumors. It uses precise radiation to target tumors. This method is non-invasive and treats tumors that are hard to reach with surgery.
This technique has many benefits. It causes little damage to healthy tissue and lowers the risk of complications. It’s a good choice for patients who can’t have open surgery.
Gamma Knife Technology
Gamma Knife radiosurgery is a form of stereotactic radiosurgery. It uses cobalt sources to focus radiation on tumors. It’s great for treating small to medium-sized tumors.
The Gamma Knife’s precision is unmatched. It delivers a high dose of radiation to the tumor while protecting nearby tissues. It’s often used for acoustic neuromas, meningiomas, and some metastatic brain tumors.
| Tumor Type | Treatment Success Rate | Common Side Effects |
| Acoustic Neuroma | 85-90% | Hearing loss, tinnitus |
| Meningioma | 80-85% | Headache, fatigue |
| Metastatic Brain Tumor | 70-80% | Nausea, neurological deficits |
CyberKnife and Other Radiosurgery Options
CyberKnife is another stereotactic radiosurgery method. It uses a linear accelerator for radiation. It’s flexible and treats tumors that move or have irregular shapes.
Novalis and TrueBeam are other options. They also deliver precise radiation. The choice depends on the tumor and the patient’s health.
“The advancements in stereotactic radiosurgery have significantly improved our ability to treat complex brain tumors, providing patients with more options and better outcomes.”
A Neurosurgeon
Ideal Candidates for Radiosurgery
Patients with small to medium-sized tumors are good candidates. Tumors in sensitive areas also benefit. We look at each case carefully to decide if radiosurgery is right.
We consider tumor size, location, and the patient’s health. This helps us choose the best treatment for each patient.
Laser Ablation and Thermal Therapies
Laser interstitial thermal therapy (LITT) is a big step forward in treating brain tumors. It offers a precise way to remove tumors. This method is great for those who can’t have open surgery or have tumors in hard-to-reach places.
Laser Interstitial Thermal Therapy (LITT)
LITT uses a laser probe to heat and kill tumor cells. It targets the tumor well, keeping the brain around it safe. The surgery is guided by MRI, so the team can watch the temperature and make sure the tumor is treated right.
Some key benefits of LITT are:
- Minimally invasive: It’s done through a small cut, cutting down on risks and helping you heal faster.
- Precision: MRI guidance lets the team aim exactly at the tumor.
- Reduced risk of neurological damage: It keeps more of the brain safe, helping you keep your functions.
Recovery and Effectiveness
Recovery from LITT is quicker than open surgery. Most people go home in a few days. Studies show LITT works well for brain tumors, helping control them and manage symptoms.
What makes LITT work depends on:
- Tumor type and location: It works best for certain tumors in certain spots.
- Patient selection: Choosing the right patients is key for success.
- Technical expertise: The skill of the neurosurgical team matters a lot.
Limitations and Considerations
LITT has its downsides. It needs special tools and experts, and it’s not for every case. Like any surgery, it comes with risks like infection and brain damage.
We look at each patient carefully to see if LITT is right for them. We consider the good and bad to give the best care for each person.
Embolization and Vascular Approaches
Embolization is a key step before surgery to make brain tumors easier to remove. It blocks the blood vessels that feed the tumor. This reduces its size and lowers the risk of bleeding during surgery.
Benefits of Pre-surgical Embolization
Pre-surgical embolization has many advantages. It cuts down on bleeding during surgery and makes tumors less vascular. It can even make tumors that were thought to be inoperable operable.
Patients who get embolization before surgery often have an easier time during surgery. The tumor becomes smaller and less vascular, making the surgery simpler.
| Benefits | Description |
| Reduced Intraoperative Bleeding | Minimizes blood loss during surgery, improving visibility and reducing complications. |
| Decreased Tumor Vascularity | Makes the tumor less vascular, facilitating a safer surgical removal. |
| Making Inoperable Tumors Operable | Can convert complex, inoperable tumors into operable ones by reducing their size and vascularity. |
Procedure and Recovery
The embolization process involves guiding a catheter to the tumor’s arteries. Then, materials are used to block these arteries. The whole thing is done under anesthesia or sedation to keep the patient comfortable.
Recovery from embolization can differ from person to person. Some might feel a headache or nausea, but these are usually treated with medication.
Combined Treatment Strategies
Embolization is often paired with other treatments like surgery, radiation, or chemotherapy. The choice of treatments depends on the tumor’s type, size, and location, and the patient’s health.
Using embolization as part of a full treatment plan can lead to better results for patients with complex brain tumors. Combining embolization with other treatments can help manage tumors more effectively.
Innovative Solutions for Previously Inoperable Brain Masses
Brain surgery is changing fast, thanks to new technologies. These advancements are opening up new ways to treat brain tumors that were once thought impossible to operate on. We’re seeing big changes in how doctors tackle these complex cases.
BrainPath Technology
BrainPath technology is a big step forward in neurosurgery. It makes surgeries more precise and less invasive. This new method lets surgeons reach tumors through a smaller path, which can lead to less damage and quicker healing.
“BrainPath technology has changed how we treat brain tumors,” says a top neurosurgeon. “It’s a major breakthrough for patients with tumors that were once too risky to operate on.”
The BrainPath system uses a special way to move through the brain. It gently parts the brain tissue along natural paths. This approach is promising for tumors in hard-to-reach areas.
Robot-Assisted Brain Surgery
Robot-assisted brain surgery is another big leap forward. It lets neurosurgeons do complex surgeries with more precision and control. The robots help surgeons handle delicate instruments better, which can lead to better results for patients.
One key advantage of robot-assisted surgery is the high-definition, 3D view it offers. This clear view, combined with the robots’ precision, helps surgeons navigate the brain’s complex structures more confidently.
Awake Craniotomy for Functional Preservation
Awake craniotomy is a special surgery where patients stay awake during parts of the procedure. It’s very useful for tumors near important brain areas. These areas are key for things like language, movement, and thinking.
In an awake craniotomy, patients are first sedated, then woken up as the tumor is removed. They’re asked to do tasks to help the team check brain function. This way, surgeons can remove more of the tumor while keeping important brain functions intact.
“Awake craniotomy has been a game-changer for patients with tumors in sensitive brain areas,” says a neurosurgeon who specializes in this method. “It lets us remove more of the tumor while reducing the risk of brain damage.”
These new solutions are making it possible to treat brain masses that were once thought too risky. By using advanced technology and skilled surgeons, we’re improving treatment options and giving patients new hope.
Advanced Technologies Guiding Brain Tumor Surgery
Brain tumor surgery is getting better thanks to new technologies. These tools help surgeons be more precise, lower risks, and improve patient results.
Intraoperative Genetic Testing
Intraoperative genetic testing lets surgeons analyze tumors during surgery. This helps them decide how much of the tumor to remove. Rapid genetic analysis finds specific markers, guiding the surgery.
Functional MRI and Tractography
Functional MRI (fMRI) and tractography map brain functions and paths. They show where tumors are in relation to important brain parts. This helps in more precise surgical planning.
Neuronavigation Systems
Neuronavigation systems use imaging data to guide surgeons. They give real-time feedback on the surgeon’s position. Enhanced spatial awareness reduces damage to key brain areas.
A leading neurosurgeon says, “Advanced technologies have changed brain tumor surgery. We can now achieve outcomes we couldn’t before.”
“The future of brain tumor surgery lies in the continued development and integration of these advanced technologies.”
Recovery and Rehabilitation After Brain Tumor Removal
Recovery and rehabilitation are key after brain tumor surgery. They need a detailed and caring plan. The path to getting better includes many steps, from right after surgery to long-term care. Each step is important for the best results.
Immediate Post-Operative Care
Right after surgery, it’s vital to watch the patient closely. They often need to stay in an intensive care unit (ICU) to manage risks like swelling or infection.
- Monitoring of vital signs and neurological status
- Management of pain and discomfort
- Prevention and treatment of complications
A team of experts is needed to take care of the patient’s health fully.
Long-term Rehabilitation
Long-term care helps patients get back their strength, movement, and thinking skills. A special program might include physical, occupational, and speech therapy. It depends on what the patient needs.
- Physical therapy to improve mobility and strength
- Occupational therapy to enhance daily functioning
- Speech therapy to address communication challenges
Rehabilitation goals are personalized to help each patient live their best life.
Managing Side Effects
Handling side effects is a big part of getting better. Side effects can be tiredness, changes in thinking, or mood swings. Good management uses medicine, lifestyle changes, and support.
- Medications to manage symptoms
- Lifestyle changes, such as diet and exercise
- Supportive therapies, including counseling and support groups
We help patients make a plan to deal with side effects. This way, they get the help they need to recover.
Conclusion
Removing brain tumors safely is a complex task. It needs careful planning, advanced tech, and skilled neurosurgeons. Different surgical methods, like minimally invasive and stereotactic radiosurgery, help treat brain tumors effectively.
Advanced tech, like genetic testing and neuronavigation systems, makes surgery safer and more precise. Knowing about the different brain tumors and when surgery is needed helps patients make better choices.
The main aim of brain tumor surgery is to remove the tumor safely and keep brain function intact. Thanks to new neurosurgical methods and tech, we can now offer better results for patients. This is a big step forward in treating brain tumors.
FAQ
What are the different types of brain tumor removal surgeries?
We use several advanced methods. These include open craniotomy, minimally invasive techniques, and radiosurgery. They help us safely remove brain tumors.
How do you determine if a brain tumor is benign or malignant?
We use advanced imaging and tests to find out the tumor type. This is key for planning the best treatment.
What are the indications for surgical removal of a brain tumor?
Surgery is often needed for tumors causing big symptoms. It’s also needed if the tumor grows or affects important brain areas.
How is the risk assessment for brain tumor surgery performed?
Our team looks at the risks and benefits. We consider the tumor’s location, size, and the patient’s health.
What is the role of advanced imaging in brain tumor surgery?
Advanced imaging, like functional MRI, helps us map the brain. This planning ensures the safest surgery approach.
What are the benefits of minimally invasive brain tumor surgery?
Minimally invasive methods, like keyhole craniotomy, cause less damage. They also reduce scarring and recovery time, making them a good choice for many.
Can radiosurgery be used to treat brain tumors?
Yes, radiosurgery, including Gamma Knife and CyberKnife, is very effective. It offers precise and non-invasive tumor removal for certain tumors.
What is laser interstitial thermal therapy (LITT), and how is it used?
LITT uses laser heat to destroy tumor tissue. It’s a promising treatment for specific brain tumors, being minimally invasive.
How does embolization help in brain tumor treatment?
Embolization reduces blood flow to the tumor before surgery. This makes it easier to remove and lowers the risk of complications.
What is BrainPath technology, and how does it improve brain tumor surgery?
BrainPath technology offers precise and minimally invasive access to tumors. It reduces tissue damage and improves surgery outcomes.
What is the role of intraoperative genetic testing in brain tumor surgery?
Intraoperative genetic testing identifies the tumor’s genetic characteristics during surgery. This helps in making better decisions and can improve outcomes.
How is neuronavigation used in brain tumor surgery?
Neuronavigation systems guide us during surgery. They help us accurately locate and remove the tumor while protecting surrounding brain tissue.
What can I expect during recovery from brain tumor removal surgery?
Our team provides care right after surgery. We also offer long-term rehabilitation to manage side effects and support recovery.
How do you manage side effects after brain tumor removal surgery?
We create personalized rehabilitation plans to address side effects. We provide ongoing support to ensure the best outcome.
References:
• National Cancer Institute. (2025). Rapid genetic test could help guide brain cancer surgery. https://www.cancer.gov/news-events/cancer-currents-blog/2025/brain-cancer-surgery-rapid-test-mutations-tumor-cells
• The Brain Tumour Charity. (n.d.). BrainPath – Surgical brain tumour removal technique. https://www.thebraintumourcharity.org/brain-tumour-diagnosis-treatment/treating-brain-tumours/emerging-treatments/brainpath/
• Frontiers in Oncology. (2024). [XML] https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1481430/xml





