Last Updated on November 26, 2025 by Bilal Hasdemir

At Liv Hospital, we know how critical it is to treat basal cell carcinoma well. This is a common skin cancer. We often choose surgery to make sure it’s gone for good. We use the newest surgical methods, like Mohs surgery and traditional excision, to treat it.
There are many ways to remove basal cell carcinoma. The right treatment depends on the tumor’s size, depth, and where it is. Surgical excision and Mohs micrographic surgery work best. We’ll walk you through these options and help you find the best one for you.
Key Takeaways
- Effective treatment of basal cell carcinoma often involves surgical removal.
- Mohs surgery and traditional excision are common surgical techniques used.
- The choice of treatment depends on the size, depth, and location of the tumor.
- Surgical excision involves removing the cancerous lesion and a surrounding margin of healthy tissue.
- Mohs surgery allows for the removal of the cancer without removing too much healthy skin around it.
Understanding Basal Cell Carcinoma

It’s important to know about basal cell carcinoma to catch it early and treat it well. Basal cell carcinoma (BCC) is the most common skin cancer. It starts in the basal cell layer of the skin. If not treated, it can cause serious damage.
What Is Basal Cell Carcinoma?
Basal cell carcinoma starts in the basal cells of the skin’s outer layer. It grows slowly and rarely spreads. But, it can damage the skin if not treated quickly.
“Basal cell carcinoma is a highly treatable form of skin cancer when detected early,” says a leading dermatologist. “Awareness of its causes and symptoms is key to effective management.”
Common Causes and Risk Factors
The main cause of basal cell carcinoma is UV radiation from the sun or tanning beds. Other risk factors include:
- Fair skin that burns easily
- History of sunburns
- Increased age
- Male gender
- Family history of skin cancer
- Exposure to certain chemicals like arsenic
- Previous radiation therapy
Knowing these risk factors helps prevent and treat basal cell carcinoma.
Signs and Symptoms to Watch For
Basal cell carcinoma can show up in different ways, such as:
- A new growth or sore that doesn’t heal
- A shiny, pink, or red bump
- A pink or red patch with a raised border
- A scar-like area that is white, yellow, or waxy
Spotting it early is key to better treatment. Regular skin checks and knowing the signs can help catch it on time.
Diagnosing Basal Cell Skin Cancer

To find basal cell carcinoma, doctors use several ways. They look at the skin and use dermatoscopy. Finding it early is key to treat it well and avoid problems.
Visual Examination and Dermatoscopy
First, doctors look at the skin to find basal cell carcinoma. They check for signs like shiny bumps or flat, flesh-colored spots. Dermatoscopy uses a special microscope to see more. It shows details not seen by the eye.
Skin Biopsy Procedures
If a spot looks like basal cell carcinoma, a skin biopsy is done. There are different biopsies, like shave or punch biopsies. The choice depends on the spot’s size and where it is. A biopsy takes a piece of skin to check for cancer cells.
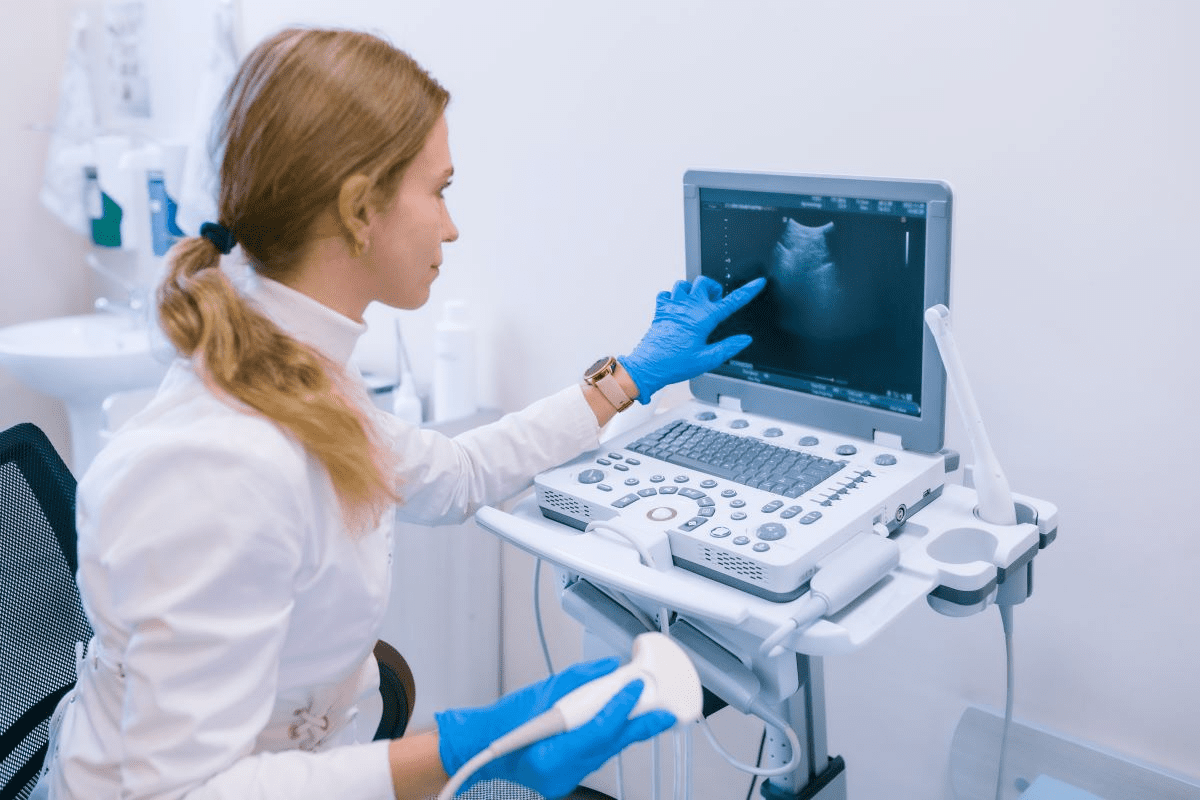
Imaging Tests for Advanced Cases
For advanced basal cell carcinoma, imaging tests are used. These include ultrasound, CT scans, or MRI scans. They show how far the cancer has spread. This helps doctors plan the best treatment.
Pre-Surgery Considerations
As you get ready for basal cell carcinoma surgery, your medical team will help you a lot. They will do a detailed check-up and plan your treatment. This makes sure you’re ready for the surgery and that it fits your needs perfectly.
Medical Evaluation and Testing
We do a full medical check-up before surgery. This might include blood tests to make sure you’re healthy enough. We’ll also look at your medical history, like past surgeries, allergies, and medicines you’re taking.
Medication Adjustments
Some medicines might need to be changed or stopped before surgery. We’ll check your medicines, like blood thinners, and tell you what to do. It’s very important to follow our advice to avoid any problems during and after the surgery.
Preparing for Your Procedure Day
On the day of your surgery, please arrive 15 minutes early. It’s a good idea to have someone with you, as you might not be able to drive right away. We’ll give you clear instructions on how to get ready, including any fasting or hygiene rules.
By following our pre-surgery advice, you can make your procedure go smoothly. If you have any questions or worries, please contact our team. We’re here to help you every step of the way.
Surgical Excision: The Standard Approach
Surgical excision is a key treatment for basal cell carcinoma. It removes the cancerous tissue and keeps the healthy skin around it safe.
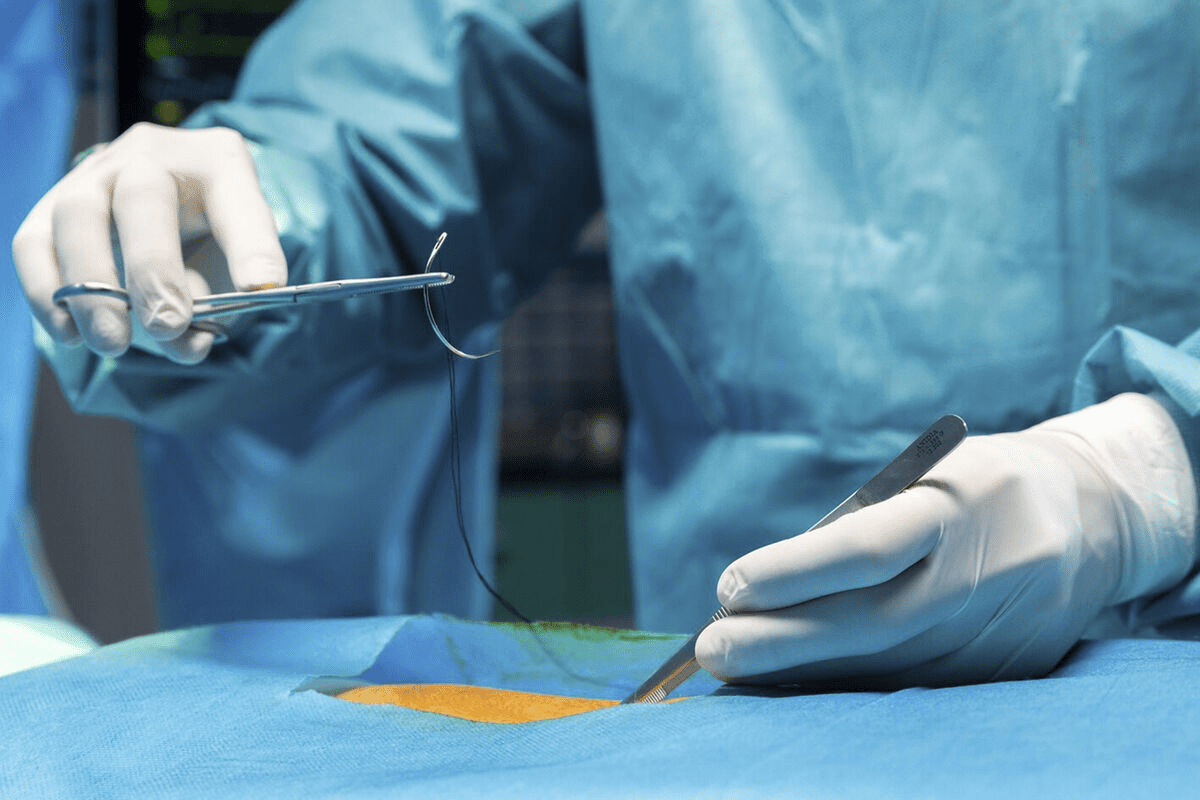
How Surgical Excision Works
Surgical excision removes the tumor and some healthy skin around it. This is important to make sure all cancer cells are gone. The procedure is done under local anesthesia, making it less painful and helping you recover faster.
The surgeon carefully takes out the tumor and some skin around it. Then, they check the removed tissue to make sure there are no cancer cells left.
Margin Requirements and Tissue Preservation
The size and location of the tumor affect how much skin needs to be removed. Usually, 2-5 mm of skin is enough for most basal cell carcinomas. But, for bigger or more aggressive tumors, more skin might be needed.
We try to keep as much healthy tissue as possible. This helps the skin look better after treatment and lowers the chance of problems.
When Surgical Excision Is Recommended
Surgical excision is often chosen for big, recurring, or sensitive tumors. It’s also best for tumors that grow fast. The choice to have surgery depends on many factors, like your health and the tumor’s details.
Knowing about surgical excision helps patients make better choices. We aim to give you the best care and support during your treatment.
Excision Depths for Different Skin Cancers
Removing skin cancers requires careful planning. The depth of excision is key. It aims to remove the cancer fully while keeping healthy tissue. This balance is important for treatment success and looks.
Typical Depths for Basal Cell Carcinoma
Basal cell carcinoma (BCC) is the most common skin cancer. It’s often treated with surgery. For BCC, a 3-5 mm margin is usually enough for small tumors. Studies show a 3 mm margin works for 85-90% of tumors under 1 cm. But, bigger or aggressive tumors might need deeper cuts.
“The margin of excision is critical in ensuring that all cancerous cells are removed,” says a renowned dermatological surgeon. “For BCC, we often aim for a balance between removing the tumor and preserving cosmetic appearance.”
How Deep Do They Cut for Squamous Cell Carcinoma?
Squamous cell carcinoma (SCC) is another common skin cancer. It often needs deeper cuts because it can grow faster. A 4-6 mm margin is usually recommended for SCC, but high-risk tumors might need wider cuts.
The depth of excision for SCC also depends on the tumor’s thickness. For tumors under 2 mm, a deeper cut might not be needed. But, thicker tumors need more extensive cuts to remove all cancerous tissue.
Factors That Determine Excision Depth
Several factors affect the depth of excision in skin cancer surgery. These include the tumor’s type, size, location, and the patient’s health. The tumor’s aggressiveness, based on its subtype and grade, is also important. For example, high-risk or recurrent tumors might need deeper cuts.
- Tumor type and size
- Location of the tumor
- Patient’s overall health
- Histological subtype and grade of the tumor
By considering these factors, surgeons can find the best excision depth for each patient. This ensures the best treatment outcome.
Mohs Micrographic Surgery Explained
Mohs micrographic surgery is known for its skill in removing skin cancer with little harm to nearby tissue. It has changed how we treat skin cancers, like basal cell carcinoma and squamous cell carcinoma.
The Step-by-Step Mohs Procedure
The Mohs procedure has several key steps. First, we take out the visible tumor and a thin layer of tissue around it. This tissue is then cut into slides and checked under a microscope.
If cancer cells are seen, we take out another layer of tissue. This is checked again under the microscope. We keep doing this until no cancer cells are found. This way, we remove all tumor tissue while keeping as much healthy tissue as we can.
During the procedure, patients are usually awake and can relax. It’s done in an outpatient setting, and the time needed varies based on the case’s complexity.
Benefits of Microscopic Examination
The microscopic check during Mohs surgery is a big plus. It lets us know right away if all cancer cells are gone. This quick feedback helps us remove the tumor precisely, cutting down on recurrence risk and healthy tissue loss.
Immediate examination also means the whole procedure can be done in one visit. This is different from other methods that might need more visits.
Ideal Candidates for Mohs Surgery
Mohs micrographic surgery is great for tumors in sensitive or important areas, like the face, ears, or hands. It’s also good for big, recurring, or fast-growing tumors.
We suggest Mohs surgery for those who want to keep as much healthy tissue as possible. It’s a top choice for skin cancers at high risk of coming back or with unclear borders.
Curettage and Electrodessication for Smaller Tumors
Curettage and electrodessication is a method used for small basal cell skin cancers. It involves two steps. First, a doctor scrapes out the tumor with a curette. Then, they apply an electric current to kill any leftover cancer cells.
The Scrape and Burn Technique
This procedure is called the “scrape and burn” technique. It starts with scraping the tumor away with a curette. This is key to removing most of the cancer cells.
Next, an electric current is used to kill any remaining cancer cells and stop bleeding. This technique is simple and works well for small tumors. It’s quick and can be done in a doctor’s office, making it easy for patients.
Limitations of This Approach
While curettage and electrodessication works for small basal cell carcinomas, it has its limits. It’s not good for big or aggressive tumors because it might not remove all cancer. It’s also not the best for tumors in areas that are important for looks or have specific features.
- Not ideal for large or aggressive tumors
- May not be suitable for cosmetically sensitive areas
- Risk of recurrence if not performed correctly
Recovery Expectations
Recovery from this treatment is usually easy. Patients might feel some pain, redness, and swelling where the treatment was done. These symptoms are short-lived and can be managed with pain meds and good wound care.
It’s important for patients to follow their doctor’s instructions well to heal right and avoid problems. Seeing the doctor regularly after treatment is also key. This helps make sure everything is healing well and catches any signs of cancer coming back.
Skin Cancer Basal Cell Removal: Comparing Procedures
We will look at the different ways to remove basal cell carcinoma. We’ll check how well they work, how they look, and their costs. This will help us compare them all.
Effectiveness Rates of Different Techniques
The success of basal cell carcinoma removal methods varies. Surgical excision is often used and works well, with cure rates over 90%. Mohs micrographic surgery is great for tricky cases, with cure rates up to 99% in some studies.
Curettage and electrodessication are less invasive but cure rates are lower. They range from 70% to 90%, depending on the tumor and the doctor’s skill.
Cosmetic Outcomes Comparison
Cosmetic results are key, mainly for tumors on the face. Mohs micrographic surgery is known for its ability to keep tissue intact and reduce scarring.
Surgical excision can also lead to good looks, with the help of reconstructive surgery. Curettage and electrodessication might leave more noticeable scars. But, this depends on the doctor’s skill and the tumor’s size.
Cost and Insurance Considerations
The cost of removing basal cell carcinoma varies a lot. Insurance coverage is key in figuring out what patients will pay out of pocket.
Mohs micrographic surgery is pricier because it’s complex and requires special training. Surgical excision can also be expensive, adding up if reconstructive surgery is needed. Curettage and electrodessication are cheaper but might need more sessions, which can raise costs.
Facial Basal Cell Carcinoma: Special Considerations
Facial basal cell carcinoma needs a special approach because of its effect on looks and function. When treating this type of cancer on the face, preserving the patient’s appearance and maintaining functional integrity are key. It’s a delicate balance between removing the cancer and keeping the patient’s quality of life high.
Preserving Appearance and Function
Treating facial basal cell carcinoma is more than just removing the tumor. It’s about making the patient’s skin look as natural as possible. We look at many factors, like the tumor’s size and location, to choose the best treatment. Advanced surgical techniques help us keep important facial structures intact and get the best cosmetic results.
Reconstructive Options After Removal
After removing the basal cell carcinoma, reconstructive surgery may be needed to fix the facial area’s look and function. We have different reconstructive options, like skin grafts and local flaps, to fit each patient’s needs. Our goal is to make the patient look natural and keep their self-esteem up.
Managing Expectations for Facial Procedures
It’s important to manage patient expectations for facial basal cell carcinoma treatment. We spend time talking about what the treatment can do, its risks, and benefits. By knowing what the patient wants and expects, we can give them care that meets their needs and improves their experience.
Advanced and High-Risk Basal Cell Carcinomas
Managing advanced and high-risk basal cell carcinomas is complex. These types of carcinomas grow fast, come back often, and can spread. They need special care.
Identifying High-Risk Features
High-risk basal cell carcinomas are spotted by their size, where they are, and how they look under a microscope. Tumors over 2 cm, in the face, ears, or genital area, are at high risk. This is because they’re close to important parts and could cause disfigurement.
Key Features of High-Risk Basal Cell Carcinomas:
- Large size (>2 cm)
- Location in high-risk areas (central face, ears, genitalia)
- Aggressive histological subtypes (micronodular, infiltrative, morpheaform)
- Depth of invasion beyond the dermis
- Recurrent tumors
- Immunosuppressed patients
Specialized Treatment Approaches
Dealing with high-risk basal cell carcinomas needs a team effort. Dermatologists, surgeons, and radiation oncologists work together. The right treatment depends on the tumor, the patient’s wishes, and their health.
| Treatment Modality | Description | Indications |
|---|---|---|
| Mohs Micrographic Surgery | Microscopically controlled surgery that removes tumor tissue layer by layer | High-risk tumors, recurrent tumors, tumors in cosmetically sensitive areas |
| Radiation Therapy | High-energy radiation to kill cancer cells | Patients who are not surgical candidates, tumors in areas difficult to reconstruct |
| Targeted Therapy | Drugs that target specific molecular pathways involved in cancer growth | Advanced or metastatic basal cell carcinoma, patients with genetic syndromes (e.g., Gorlin syndrome) |
Multidisciplinary Care for Complex Cases
For complex basal cell carcinoma cases, a team approach is best. This team includes dermatologists, surgeons, and more. They ensure all aspects of the disease are covered.
Multidisciplinary care is key for advanced or high-risk basal cell carcinomas. It helps create a treatment plan that fits the patient’s health, tumor details, and wishes.
By working together, we can better treat these cancers. This approach improves outcomes, lowers recurrence risk, and boosts patient quality of life.
Non-Surgical Treatment Alternatives
Non-surgical treatments are great for managing basal cell carcinoma in some cases. They are perfect for those who can’t have surgery or prefer less invasive methods.
Topical Medications and Their Efficacy
Topical medications are creams or gels applied to the skin. They treat superficial basal cell carcinomas.
Imiquimod cream boosts the body’s immune system to fight cancer cells. 5-fluorouracil cream stops abnormal cells from growing.
The success of these treatments depends on the tumor’s size, depth, and location. It also depends on the patient’s health.
Radiation Therapy Options
Radiation therapy uses high-energy rays to kill cancer cells. It’s good for tumors in sensitive areas or hard to reach surgically.
External beam radiation therapy (EBRT) sends radiation from outside the body. Brachytherapy places a radioactive source near the tumor.
Emerging Treatments and Clinical Trials
New treatments for basal cell carcinoma are being researched. Targeted therapy and immunotherapy are among them.
Targeted therapy uses drugs that target cancer cells, sparing normal cells. Immunotherapy boosts the body’s immune response against cancer.
| Treatment | Description | Efficacy |
|---|---|---|
| Topical Medications | Creams or gels applied directly to the skin | Effective for superficial basal cell carcinomas |
| Radiation Therapy | Uses high-energy rays to kill cancer cells | Recommended for tumors in sensitive areas or difficult to treat surgically |
| Emerging Treatments | Targeted therapy and immunotherapy | Shows promise in clinical trials |
The Patient Experience: What to Expect
We’re here to help you understand what to expect during and after basal cell carcinoma removal. Knowing what to expect can help reduce anxiety and make your recovery smoother.
During the Procedure: Sensations and Timeline
During the procedure, you might feel some sensations. These can depend on the treatment type. For surgical excision, local anesthesia numbs the area, so you won’t feel pain during it. Some might feel a pinch when the anesthesia is given, but this is usually the most uncomfortable part.
The procedure’s length can vary, but most surgical excisions last about 30 minutes to an hour. Mohs surgery, which checks the tissue during the procedure, can take longer.
| Procedure Type | Typical Duration | Sensations During Procedure |
|---|---|---|
| Surgical Excision | 30 minutes – 1 hour | Pinch from anesthesia, pressure during excision |
| Mohs Surgery | Several hours | Variable, depending on the number of stages |
Immediate Post-Procedure Effects
Right after the procedure, you might see redness, swelling, and discomfort at the removal site. These effects are usually short-lived and can be managed with over-the-counter pain meds and cold compresses.
Following your doctor’s post-procedure care instructions is key to avoiding complications and aiding healing. This might include keeping the wound clean, using topical ointments, and avoiding heavy activities.
Patient Stories and Perspectives
Listening to others who’ve gone through similar experiences can be very reassuring. Many patients feel relieved after the procedure, knowing the cancer is gone. Some worry about scarring, but most are surprised by how little it affects their appearance.
“I was nervous about the procedure, but the team was so supportive and explained everything clearly. The recovery was easier than I expected.” –
These stories show how important personalized care and support are during treatment.
Recovery After Basal Cell Carcinoma Removal
Recovering well after basal cell carcinoma removal is key. The time after surgery is important for healing and avoiding problems.
Immediate Post-Operative Care
Right after surgery, taking good care is essential. Keep the wound dry and covered with a bandage for at least 24 hours. Always follow your doctor’s specific advice, as they may have special instructions for you.
Key aspects of immediate post-operative care include:
- Watching for signs of infection, like redness, swelling, or more pain
- Using the pain medicine your doctor prescribed
- Staying away from activities that might hurt the wound
Wound Healing Timeline
The healing of a wound usually follows a set timeline. The first healing steps happen in a few weeks. But, it can take months to fully recover.
The healing stages are:
- Inflammation (0-4 days)
- Proliferation (4-21 days)
- Remodeling (21 days to 2 years)
Managing Complications and When to Call Your Doctor
Complications are rare, but knowing the signs is important. If you see more redness, swelling, or pain, or notice infection signs, call your doctor.
It’s always better to err on the side of caution when it comes to your health. If you’re unsure about your recovery, always ask your healthcare provider for advice.
Preventing Future Skin Cancers
Preventing skin cancer is as important as treating it. We’re here to help you with effective ways to prevent it. This includes sun protection, regular skin checks, and making lifestyle changes.
Sun Protection Strategies
Keeping your skin safe from the sun is key to preventing skin cancer. Use a broad-spectrum sunscreen with an SPF of 30 or higher every day, even on cloudy days. Reapply every two hours or right after swimming or sweating.
Wearing the right clothes can also help a lot. Wear long-sleeved shirts, pants, and a wide-brimmed hat when you’re outside, mainly during the hottest part of the day (10 am to 4 pm).
| Sun Protection Measure | Description | Benefits |
|---|---|---|
| Sunscreen | Apply SPF 30 or higher daily | Protects against UVB rays |
| Protective Clothing | Wear long-sleeved shirts and pants | Covers skin from direct sun exposure |
| Shade | Stay in the shade, mainly during peak hours | Reduces direct sun exposure |
Regular Skin Examinations
Regular skin checks are essential for catching problems early. Do self-exams every month to spot any new or changing moles. Also, get annual skin checks from a dermatologist.
Lifestyle Modifications for Reduced Risk
Changing your lifestyle can also lower your risk of skin cancer. Avoid tanning beds because they give off UV radiation that can cause skin cancer. Eating a healthy diet full of fruits, veggies, and omega-3s is also good for your skin.
By using sun protection, doing regular skin checks, and living a healthy lifestyle, you can greatly lower your risk of getting skin cancer in the future.
Conclusion
We’ve looked at how to treat basal cell carcinoma, including surgery and non-surgical methods. It’s key to know the different ways to remove skin cancer for the best results.
Dealing with basal cell carcinoma needs a full plan, from removal to aftercare. Choosing the right treatment helps patients get better and lowers the chance of it coming back.
Preventing basal cell carcinoma is also important. Protecting yourself from the sun, getting skin checks, and changing your lifestyle can help a lot.
In conclusion, the best treatment for basal cell carcinoma is one that fits the patient’s needs. Always get medical help for the right diagnosis and treatment.
FAQ
What is basal cell carcinoma and how is it typically treated?
Basal cell carcinoma is a common skin cancer. It’s usually treated by removing it surgically. The type of surgery depends on the tumor’s size, location, and depth.
How deep do they cut for squamous cell carcinoma?
The depth of removal for squamous cell carcinoma varies. It depends on the tumor’s thickness and where it is. Generally, it’s deeper than for basal cell carcinoma to remove all cancer cells.
What are the different procedures for removing basal cell carcinoma?
There are several ways to remove basal cell carcinoma. These include surgical excision, Mohs micrographic surgery, and curettage and electrodessication. Non-surgical treatments like topical medications and radiation therapy are also options.
How is Mohs micrographic surgery different from standard surgical excision?
Mohs surgery checks the tumor’s margins under a microscope during the procedure. This allows for precise removal of cancerous tissue while sparing healthy tissue.
What is curettage and electrodessication, and when is it used?
Curettage and electrodessication involves scraping away the tumor and then applying an electric current. It’s often used for smaller, superficial basal cell carcinomas.
How can I prepare for basal cell carcinoma removal surgery?
To prepare, you’ll need a medical evaluation and may need to adjust your medications. Follow your healthcare provider’s instructions carefully to ensure a smooth procedure and recovery.
What are the cosmetic outcomes of different basal cell carcinoma removal procedures?
Cosmetic outcomes vary by procedure. Mohs surgery often provides excellent results due to its tissue-sparing nature. Other methods may have different outcomes based on the tumor’s size and location.
How can I prevent future skin cancers?
To prevent skin cancers, protect your skin from the sun. Use sunscreen and wear protective clothing. Also, have regular skin examinations and avoid excessive sun exposure.
What are the signs and symptoms of basal cell carcinoma that I should watch for?
Look out for new or changing growths on your skin. This includes bumps, lesions, or sores that don’t heal. If you notice anything unusual, consult a healthcare professional.
Are there non-surgical treatment options for basal cell carcinoma?
Yes, there are non-surgical options. These include topical medications, radiation therapy, and emerging treatments. These may be considered based on the tumor’s characteristics and your overall health.