Last Updated on November 27, 2025 by Bilal Hasdemir

When the body’s immune system attacks its own tissues, it leads to autoimmune diseases. There are over 80 recognized conditions in this category. At Liv Hospital, we focus on providing effective care for these conditions.
Treating autoimmune disorders needs a detailed approach. This approach aims to control symptoms and fix the immune system’s wrong response. We use the latest treatments, including stem cell therapy, to help patients fight back and regain their health.
Key Takeaways
- Autoimmune diseases happen when the immune system attacks the body’s own tissues.
- There are over 80 recognized autoimmune diseases.
- Effective care involves controlling symptoms and correcting the immune system’s response.
- Liv Hospital offers the latest treatments, including stem cell therapy.
- A detailed approach is key for managing autoimmune disorders.
Understanding Autoimmune Disorders

Autoimmune disorders happen when the body’s immune system attacks its own cells, tissues, and organs. This is due to a mix of genetic and environmental factors. It leads to many diseases that affect different parts of the body.
What Happens When Your Body Attacks Itself
In autoimmune diseases, the immune system can’t tell the difference between self and non-self. This causes it to make autoantibodies that attack the body’s own tissues. The results can be very harmful, causing chronic inflammation, tissue damage, and various symptoms.
Common Types of Autoimmune Diseases
There are over 80 recognized autoimmune diseases. Some examples include:
- Rheumatoid Arthritis: A condition that causes inflammation in the joints.
- Lupus: A disease that can affect multiple organs, including the skin, joints, and kidneys.
- Type 1 Diabetes: A condition where the immune system attacks the insulin-producing beta cells in the pancreas.
- Multiple Sclerosis: A disease that affects the central nervous system, leading to issues with vision, muscle control, and other basic bodily functions.
- Hashimoto’s Thyroiditis: A condition that affects the thyroid gland, leading to hypothyroidism.
Risk Factors and Prevalence
Research suggests that 5–10% of the global population may have autoimmune diseases. Risk factors include genetic predisposition, environmental triggers, and hormonal influences. Knowing these factors helps in early diagnosis and effective management.
Recognizing the Signs and Symptoms

Spotting early signs of autoimmune disorders is key to better treatment. Autoimmune diseases happen when the body’s immune system attacks itself. Symptoms vary based on the disease and affected areas.
General Symptoms Across Autoimmune Conditions
Many autoimmune diseases share common symptoms. Fatigue, joint pain, and skin rashes are common. These symptoms can make it hard to diagnose early.
Other common symptoms include:
- Muscle pain and weakness
- Fever
- Swollen glands
- Sensitivity to sunlight
Disease-Specific Symptoms
Each autoimmune disease has its own set of symptoms. For example, rheumatoid arthritis mainly affects joints, causing pain and stiffness. Type 1 diabetes impacts the pancreas, leading to high blood sugar.
| Autoimmune Condition | Primary Symptoms |
|---|---|
| Rheumatoid Arthritis | Joint pain, swelling, stiffness |
| Type 1 Diabetes | High blood sugar, increased thirst and urination |
| Lupus | Butterfly-shaped rash on the face, joint pain, kidney issues |
When to Seek Medical Attention
If you have symptoms that could be autoimmune, see a doctor. Early treatment can greatly improve your life.
Red flags for immediate medical help include:
- Severe joint pain or swelling
- Unexplained fever or weight loss
- Skin rashes or lesions
- Neurological symptoms such as numbness or weakness
Knowing the signs of autoimmune diseases is the first step to managing them. Recognizing symptoms and knowing when to seek help can help you stay healthy.
Getting Diagnosed: The First Step to Treatment
Getting a correct diagnosis is key to treating autoimmune disorders. These diseases are hard to diagnose because their symptoms can look like other illnesses. But, with a detailed diagnostic process, doctors can pinpoint the exact condition.
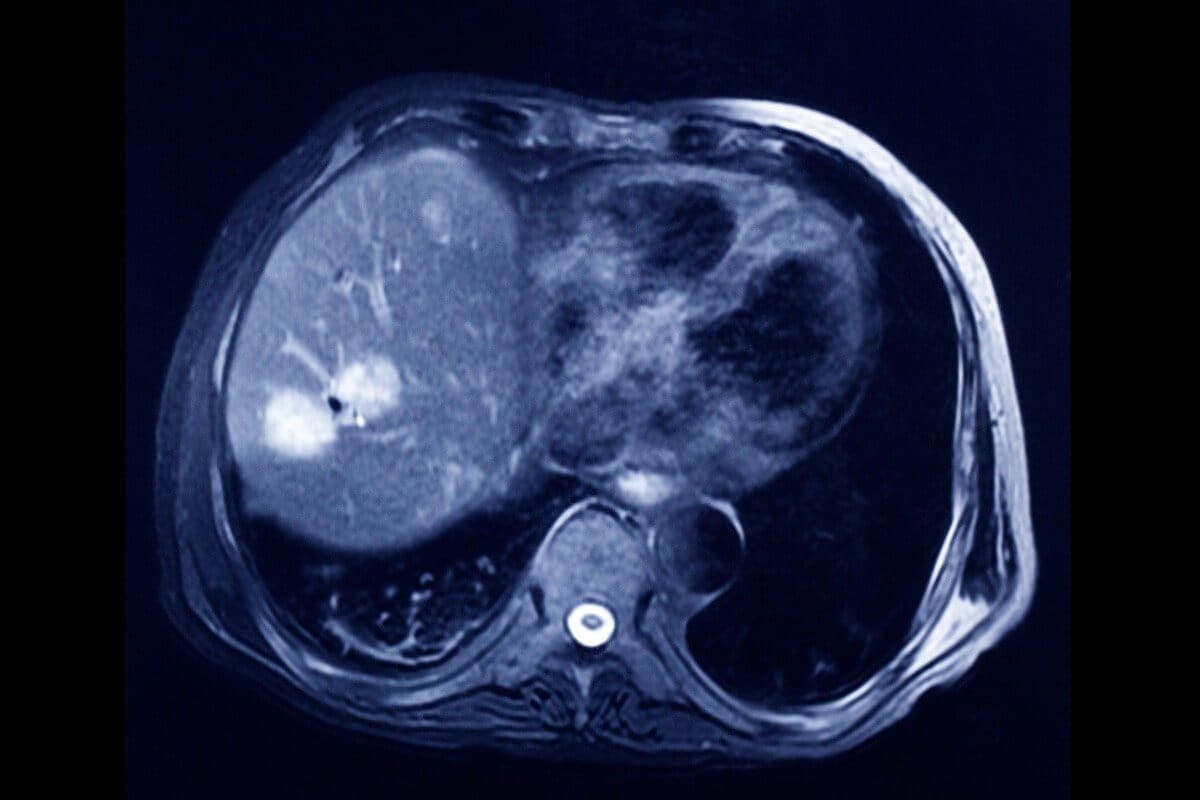
Common Diagnostic Tests
Doctors use a mix of medical history, physical exams, and lab tests to diagnose autoimmune diseases. Blood tests help find specific antibodies linked to certain conditions. For example, antinuclear antibodies (ANA) often point to lupus or rheumatoid arthritis.
Other tools like imaging studies are used to see tissue damage or inflammation. This includes X-rays, ultrasound, or MRI scans.
Working with Specialists
Autoimmune diseases are complex, so specialists are often needed. Rheumatologists usually handle conditions like rheumatoid arthritis and lupus. Other specialists, like endocrinologists for thyroid diseases or gastroenterologists for liver diseases, may also be involved.
Working together, healthcare teams provide a thorough evaluation and accurate diagnosis. A case study shows how a team saved a music conductor’s life, highlighting the value of teamwork in complex cases. You can read more about it here.
Understanding Your Test Results
After tests, it’s important to understand the results. Doctors will explain the findings and what they mean for your condition. Patients should ask questions to fully grasp their diagnosis and treatment plan.
While many autoimmune diseases are chronic, there are treatments to manage symptoms and slow disease progress. Knowing that these diseases are not curable but can be managed helps patients cope better.
Creating a Treatment Plan with Your Healthcare Team
To manage autoimmune conditions well, making a personalized treatment plan is key. This plan should fit your specific condition, health, and lifestyle. Working with your healthcare providers is essential for a tailored approach.
Building Your Medical Support Network
A strong medical support network is vital for managing autoimmune diseases. This network should include primary care doctors, specialists like rheumatologists, and other experts like physical therapists or dietitians. Effective communication among team members is key to coordinate your care.
When building your network, think about each member’s expertise and how they can help. For example, a specialist can offer the latest treatments for your condition. A dietitian can help with an anti-inflammatory diet plan.
Setting Treatment Goals
Setting clear, achievable treatment goals is critical for managing autoimmune disorders. These goals should be specific, measurable, and align with your health objectives. For instance, a goal might be to reduce flare-ups or improve your daily activities.
Work closely with your healthcare team to set these goals. It’s also important to regularly review and adjust them as your condition changes or new treatments emerge. Recent advancements, like Novartis’s iptacopan for IgA nephropathy, show the importance of staying updated on treatments.
Tracking Your Progress
Tracking your progress is essential to see if your treatment plan is working. This means monitoring your symptoms, health metrics, and any medication side effects. Keeping a health journal can help track your condition and find patterns or triggers.
Your healthcare team will also use tests and assessments to check your condition. By combining your observations with medical data, you and your team can make informed decisions about your treatment plan.
Conventional Medical Approaches to How to Treat Autoimmune Disorders
Conventional medicine is key in managing autoimmune disorders. It aims to control symptoms, reduce inflammation, and fix the immune system’s wrong response. Patients can work with their doctors to find the best treatment plan.
Anti-inflammatory Medications
Anti-inflammatory drugs are often the first choice for treating autoimmune disorders. These drugs, like NSAIDs, cut down inflammation and ease symptoms like pain and swelling. Managing inflammation well is key to avoiding long-term damage to the body’s tissues.
Immunosuppressant Therapies
Immunosuppressant therapies calm down the immune system’s wrong response in autoimmune diseases. These medicines are vital for conditions where the immune system attacks healthy tissues. They help reduce the immune system’s activity, preventing more damage and helping healing.
Corticosteroids and Their Role
Corticosteroids are strong anti-inflammatory drugs used for many autoimmune conditions. They quickly reduce inflammation and slow down the immune system’s response. Corticosteroids can be taken by mouth or injected, based on the inflammation’s severity and location.
Biologics and Targeted Treatments
Biologics and targeted treatments are newer therapies that target specific immune system parts in autoimmune diseases. These treatments can be very effective for those who don’t respond to traditional therapies. Biologics block specific proteins or cells that cause inflammation and tissue damage.
Advanced Treatment Options
Advanced treatments offer new hope for managing autoimmune diseases. When conventional treatments fail, these innovative approaches can bring significant relief. They improve the quality of life for patients.
Plasma Exchange Therapy
Plasma exchange therapy, also known as plasmapheresis, removes plasma from the blood. This removes harmful antibodies. It’s useful for severe autoimmune conditions where antibodies attack the body’s own tissues.
Benefits of Plasma Exchange Therapy:
- Reduces the level of harmful antibodies in the blood
- Can provide rapid relief from severe symptoms
- May be used in conjunction with other treatments for enhanced effectiveness
Intravenous Immunoglobulin (IVIG)
IVIG involves infusing high doses of antibodies into the patient’s bloodstream. These antibodies help modulate the immune system and reduce inflammation.
“IVIG has been a game-changer for many patients with autoimmune disorders, providing a new treatment option when others fail.”
Key aspects of IVIG treatment:
| Treatment Aspect | Description |
|---|---|
| Mechanism | Modulates the immune system by introducing external antibodies |
| Benefits | Reduces inflammation and immune system dysregulation |
| Administration | Given intravenously, typically in a clinical setting |
Stem Cell Transplantation
Stem cell transplantation is a more aggressive treatment. It resets the immune system. This is done by destroying existing immune cells and then regenerating them from the patient’s own stem cells.
Emerging Immunotherapies
Emerging immunotherapies are a promising area in treating autoimmune diseases. They include targeted therapies that address the immune system’s dysregulation without broadly suppressing it.
Examples of Emerging Immunotherapies:
- Biologic agents that target specific components of the immune response
- Gene therapies aimed at correcting the underlying genetic causes of autoimmunity
- Cell-based therapies that modulate the immune system
As research advances, these emerging therapies could revolutionize treating autoimmune disorders. They offer more personalized and effective care.
Nutrition Strategies for Managing Autoimmune Conditions
Nutrition is key in managing autoimmune conditions. It helps reduce symptoms and improves life quality. By choosing the right foods, people can control their condition better and feel better overall.
Anti-inflammatory Diet Approaches
An anti-inflammatory diet is essential for managing autoimmune diseases. It focuses on eating foods that lower inflammation and avoiding those that increase it. Foods like fruits, vegetables, whole grains, and healthy fats are important.
Benefits of an Anti-inflammatory Diet:
- Reduces inflammation and oxidative stress
- Supports the immune system’s natural balance
- Promotes overall health and wellbeing
Foods to Embrace and Avoid
Knowing which foods to eat and avoid is important. Embracing nutrient-rich foods like leafy greens, berries, and omega-3 rich fish helps manage symptoms. Avoid processed foods, sugars, and saturated fats that can cause inflammation.
| Foods to Embrace | Foods to Avoid |
|---|---|
| Leafy greens (spinach, kale) | Processed meats (sausages, bacon) |
| Berries (blueberries, strawberries) | Sugary drinks and snacks |
| Fatty fish (salmon, sardines) | Refined grains (white bread, pasta) |
Supplements That May Help
While diet is essential, some supplements can offer extra support. Omega-3 fatty acids, vitamin D, and probiotics may help reduce inflammation and support the immune system. Always talk to a healthcare provider before starting any supplements.
Meal Planning and Preparation Tips
Good meal planning is vital for sticking to an anti-inflammatory diet. Try preparing meals ahead of time, use seasonal produce, and try new recipes with anti-inflammatory ingredients.
Practical Tips:
- Plan your meals around seasonal fruits and vegetables
- Cook in bulk to save time during the week
- Experiment with new recipes that feature anti-inflammatory foods
Physical Activity and Exercise Guidelines
Moving your body every day can really help with autoimmune diseases. It boosts your health and can make symptoms less severe.
Benefits of Regular Movement
Being active regularly is great for those with autoimmune disorders. It cuts down on inflammation, improves heart health, and boosts mood. Exercise also helps lower anxiety and depression, common in autoimmune patients.
- Improves cardiovascular health
- Enhances mental wellbeing
- Reduces inflammation
- Increases flexibility and strength
Low-Impact Exercise Options
Low-impact exercises are best for those with autoimmune diseases. They’re easy on the joints and don’t usually cause flares. Good choices include:
- Yoga: Enhances flexibility and reduces stress
- Swimming: Provides a full-body workout without high-impact stress
- Cycling: Improves cardiovascular health and strengthens legs
- Walking: A simple and accessible form of exercise
Adapting Workouts During Flares
It’s important to listen to your body and adjust your workout plan when you’re having a flare. Lowering the intensity or taking a break can stop symptoms from getting worse. Here are some tips for adjusting workouts during flares:
- Reduce the intensity of your workout
- Opt for low-impact activities
- Consider alternative therapies like physical therapy or massage
Building a Sustainable Routine
Creating a lasting exercise plan is key for managing autoimmune disorders. Set achievable goals, track your progress, and adjust as needed. A well-thought-out plan helps keep you consistent and motivated.
| Exercise Component | Tips for Sustainability |
|---|---|
| Frequency | Aim for at least 3 times a week, with gradual increase |
| Intensity | Start low and gradually increase based on tolerance |
| Type | Mix low-impact exercises like yoga, swimming, and cycling |
Stress Management and Emotional Wellbeing
Stress has a big impact on autoimmune conditions. Learning to manage stress can improve wellbeing. Stress can make symptoms worse, making daily life hard for those with autoimmune disorders. So, it’s important to use effective stress management techniques.
The Connection Between Stress and Autoimmunity
Stress affects the immune system in complex ways. When we’re stressed, our body’s “fight or flight” response kicks in. This releases hormones like cortisol. While cortisol helps us respond to threats, too much can upset the immune system’s balance, making autoimmune conditions worse.
Mindfulness and Meditation Practices
Mindfulness and meditation are good for managing stress and emotional wellbeing. These practices help us stay in the present moment. They reduce worries about the past or future. Regular practice can lower stress, improve mood, and help us deal with autoimmune disease challenges.
To start, try short sessions (5-10 minutes) and increase time as you get more comfortable. Use guided meditation apps or join local mindfulness classes to help you.
Sleep Optimization Strategies
Good sleep is key for health, even more so for those with autoimmune disorders. Bad sleep can make symptoms worse, while good sleep helps manage stress and supports the immune system. To improve sleep, keep a regular sleep schedule, have a relaxing bedtime routine, and make your sleep environment comfortable.
Coping with the Emotional Impact of Chronic Illness
Living with an autoimmune disorder can be emotionally tough. It involves dealing with chronic pain, fatigue, and the uncertainty of flare-ups. It’s important to face these emotional challenges and seek help when needed. Joining support groups online or in-person can help you feel connected. Professional counseling or therapy can also provide tools for managing emotional aspects of chronic illness.
By focusing on stress management and emotional wellbeing, people with autoimmune disorders can better handle their conditions. This can improve their quality of life.
Complementary and Alternative Approaches
Exploring the world of autoimmune disease management shows us the value of complementary and alternative therapies. Many people with autoimmune disorders look for holistic treatments to go along with their usual care.
Acupuncture and Traditional Chinese Medicine
Acupuncture, a part of Traditional Chinese Medicine (TCM), has been treating health issues for centuries. It helps regulate the immune system and lower inflammation by stimulating certain body points.
Benefits of Acupuncture for Autoimmune Diseases:
- Reduced inflammation
- Improved immune function
- Enhanced overall wellbeing
Massage and Physical Therapies
Massage therapy and other physical therapies can ease symptoms like pain and stiffness from autoimmune disorders. They also help reduce stress, which can make autoimmune conditions worse.
Types of Massage Therapy:
- Swedish massage
- Deep tissue massage
- Myofascial release
Mind-Body Practices
Mind-body practices, like meditation and yoga, help manage stress and promote relaxation. They can improve immune function and overall health.
Evaluating Alternative Treatments Safely
When looking into complementary and alternative therapies, it’s key to do so safely. Here are some guidelines:
| Therapy | Potential Benefits | Precautions |
|---|---|---|
| Acupuncture | Reduces inflammation, improves immune function | Ensure practitioner is licensed and uses sterile needles |
| Massage Therapy | Relieves pain and stiffness, reduces stress | Inform therapist about your condition and any sensitivities |
| Mind-Body Practices | Reduces stress, promotes relaxation | Start slowly and listen to your body |
Adding these complementary and alternative approaches to your treatment plan can improve your overall wellbeing. It can also help manage your autoimmune condition better.
Managing Flare-Ups and Daily Life
Autoimmune disorders can be unpredictable. It’s important to find ways to manage flare-ups and keep up with daily life. Flare-ups can make it hard to do everyday things and affect your health.
Identifying Trigger Factors
Knowing what causes flare-ups is key. Common triggers include:
- Stress: Both physical and emotional stress can trigger or make flare-ups worse.
- Diet: Some foods can cause inflammation and worsen symptoms.
- Environmental Factors: Exposure to certain chemicals or changes in weather can also trigger flare-ups.
By knowing your personal triggers, you can take steps to avoid them. This can help reduce how often and how bad flare-ups are.
Creating an Emergency Action Plan
Having a plan for severe flare-ups is essential. This plan should include:
- Medication List: A list of your current medications and how much to take.
- Emergency Contacts: The contact info for your healthcare providers and emergency services.
- Symptom Management: Steps to take when symptoms get worse, including when to get medical help.
A good emergency plan ensures you get the right care when you need it most.
Workplace Accommodations and Disability Benefits
Managing autoimmune disorders at work can be tough. Workplace accommodations can help a lot. These might include flexible hours, ergonomic changes, or working from home.
Building a Support System
Having a support system is vital. This can include:
- Family and Friends: Teaching them about your condition helps them support you better.
- Support Groups: Connecting with others who understand can offer emotional support and advice.
- Healthcare Professionals: Regular check-ins with your healthcare team can help manage your condition.
A strong support system can greatly improve your life with an autoimmune disorder.
Conclusion: Living Well with Autoimmune Disorders
Managing autoimmune disorders well needs a full approach. This includes medical care, lifestyle changes, and ongoing support. Working with their healthcare team, people can make a plan that fits their needs and helps them feel better.
Dealing with autoimmune disease is tough, but it’s possible to manage it. Eating right, staying active, and managing stress are key. Taking charge of their health helps people live fully despite their condition.
It’s a long journey to manage autoimmune disorders. It takes patience, persistence, and the right support. We urge people to learn more, find resources, and connect with others who get it. Together, we can make a difference for those with autoimmune conditions.
FAQ
What is an autoimmune disorder?
An autoimmune disorder happens when the immune system attacks the body’s own tissues. It thinks these tissues are foreign invaders.
What are the common symptoms of autoimmune disorders?
Symptoms include fatigue, joint pain, skin rashes, and fever. But, symptoms can vary a lot depending on the condition.
How are autoimmune disorders diagnosed?
Doctors use a medical history, physical exam, and tests like blood work and imaging studies to diagnose.
What are the conventional medical approaches to treating autoimmune disorders?
Doctors often use anti-inflammatory meds, immunosuppressants, and corticosteroids. These help manage symptoms and reduce immune activity.
Are there any advanced treatment options available for autoimmune disorders?
Yes, advanced treatments include plasma exchange, IVIG, and stem cell transplantation. They can be effective for some conditions.
How can nutrition strategies help manage autoimmune conditions?
Eating an anti-inflammatory diet and avoiding trigger foods can help. Adding beneficial supplements also improves health.
What role does physical activity play in managing autoimmune disorders?
Low-impact exercise can reduce symptoms and improve function. It’s important to adjust workouts during flares.
How can stress management techniques help with autoimmune disorders?
Stress management like mindfulness, meditation, and good sleep can lessen stress’s impact on autoimmune conditions.
Can complementary and alternative approaches be used to treat autoimmune disorders?
Yes, methods like acupuncture, massage, and mind-body practices can help manage symptoms. They can be used with conventional treatments.
How can I manage flare-ups and daily life with an autoimmune disorder?
Identify triggers, create an emergency plan, and seek workplace help or disability benefits. These steps help manage daily life.
Are autoimmune disorders curable?
Some autoimmune disorders can be managed well, but a “cure” is not always possible. Yet, with the right treatment and lifestyle, many people live active, fulfilling lives.
How do I build a support system for living with an autoimmune disorder?
Work with healthcare providers, connect with others with similar conditions, and find resources and support groups.
What is the importance of working with specialists in treating autoimmune disorders?
Specialists offer targeted care, manage complex cases, and provide expertise in specific treatments and therapies.
How can I track my progress in managing an autoimmune disorder?
Regular check-ins with healthcare providers, monitoring symptoms, and adjusting treatment plans are key to tracking progress.
What is an autoimmune disorder?
An autoimmune disorder happens when the immune system attacks the body’s own tissues. It thinks these tissues are foreign invaders.
What are the common symptoms of autoimmune disorders?
Symptoms include fatigue, joint pain, skin rashes, and fever. But, symptoms can vary a lot depending on the condition.
How are autoimmune disorders diagnosed?
Doctors use a medical history, physical exam, and tests like blood work and imaging studies to diagnose.
What are the conventional medical approaches to treating autoimmune disorders?
Doctors often use anti-inflammatory meds, immunosuppressants, and corticosteroids. These help manage symptoms and reduce immune activity.
Are there any advanced treatment options available for autoimmune disorders?
Yes, advanced treatments include plasma exchange, IVIG, and stem cell transplantation. They can be effective for some conditions.
How can nutrition strategies help manage autoimmune conditions?
Eating an anti-inflammatory diet and avoiding trigger foods can help. Adding beneficial supplements also improves health.
What role does physical activity play in managing autoimmune disorders?
Low-impact exercise can reduce symptoms and improve function. It’s important to adjust workouts during flares.
How can stress management techniques help with autoimmune disorders?
Stress management like mindfulness, meditation, and good sleep can lessen stress’s impact on autoimmune conditions.
Can complementary and alternative approaches be used to treat autoimmune disorders?
Yes, methods like acupuncture, massage, and mind-body practices can help manage symptoms. They can be used with conventional treatments.
How can I manage flare-ups and daily life with an autoimmune disorder?
Identify triggers, create an emergency plan, and seek workplace help or disability benefits. These steps help manage daily life.
Are autoimmune disorders curable?
Some autoimmune disorders can be managed well, but a “cure” is not always possible. Yet, with the right treatment and lifestyle, many people live active, fulfilling lives.
How do I build a support system for living with an autoimmune disorder?
Work with healthcare providers, connect with others with similar conditions, and find resources and support groups.
What is the importance of working with specialists in treating autoimmune disorders?
Specialists offer targeted care, manage complex cases, and provide expertise in specific treatments and therapies.
How can I track my progress in managing an autoimmune disorder?
Regular check-ins with healthcare providers, monitoring symptoms, and adjusting treatment plans are key to tracking progress.
What is an autoimmune disorder?
An autoimmune disorder happens when the immune system attacks the body’s own tissues. It thinks these tissues are foreign invaders.
What are the common symptoms of autoimmune disorders?
Symptoms include fatigue, joint pain, skin rashes, and fever. But, symptoms can vary a lot depending on the condition.
How are autoimmune disorders diagnosed?
Doctors use a medical history, physical exam, and tests like blood work and imaging studies to diagnose.
What are the conventional medical approaches to treating autoimmune disorders?
Doctors often use anti-inflammatory meds, immunosuppressants, and corticosteroids. These help manage symptoms and reduce immune activity.
Are there any advanced treatment options available for autoimmune disorders?
Yes, advanced treatments include plasma exchange, IVIG, and stem cell transplantation. They can be effective for some conditions.
How can nutrition strategies help manage autoimmune conditions?
Eating an anti-inflammatory diet and avoiding trigger foods can help. Adding beneficial supplements also improves health.
What role does physical activity play in managing autoimmune disorders?
Low-impact exercise can reduce symptoms and improve function. It’s important to adjust workouts during flares.
How can stress management techniques help with autoimmune disorders?
Stress management like mindfulness, meditation, and good sleep can lessen stress’s impact on autoimmune conditions.
Can complementary and alternative approaches be used to treat autoimmune disorders?
Yes, methods like acupuncture, massage, and mind-body practices can help manage symptoms. They can be used with conventional treatments.
How can I manage flare-ups and daily life with an autoimmune disorder?
Identify triggers, create an emergency plan, and seek workplace help or disability benefits. These steps help manage daily life.
Are autoimmune disorders curable?
Some autoimmune disorders can be managed well, but a “cure” is not always possible. Yet, with the right treatment and lifestyle, many people live active, fulfilling lives.
How do I build a support system for living with an autoimmune disorder?
Work with healthcare providers, connect with others with similar conditions, and find resources and support groups.
What is the importance of working with specialists in treating autoimmune disorders?
Specialists offer targeted care, manage complex cases, and provide expertise in specific treatments and therapies.
How can I track my progress in managing an autoimmune disorder?
Regular check-ins with healthcare providers, monitoring symptoms, and adjusting treatment plans are key to tracking progress.
References
WebMD. Autoimmune diseases. https://www.webmd.com/a-to-z-guides/autoimmune-diseases
National Center for Biotechnology Information (NCBI). Treating Human Autoimmunity: Current Practice and Future Prospects. https://pmc.ncbi.nlm.nih.gov/articles/PMC4061980/
American Association of Immunologists. Treatments for Autoimmune Disorders. https://immunologyexplained.aai.org/topics/autoimmune-disorders/treatments-for-autoimmune-disorders
MedlinePlus. Autoimmune diseases. https://medlineplus.gov/autoimmunediseases.html