Targeted therapy for childhood leukemia uses drugs that target specific cancer cell growth pathways. This results in fewer side effects compared to traditional chemotherapy.

This method has changed how to treat childhood leukemia for the better. It offers precise, lower-toxicity treatments that reduce harmful side effects. These approaches have greatly improved patient outcomes. Now, when learning how to treat childhood leukemia, doctors can provide more tailored treatment plans thanks to the advancements in targeted therapy.
Key Takeaways
- Targeted therapy is a precise treatment approach for leukemia.
- It blocks specific molecular pathways critical for cancer cell growth.
- Fewer side effects occur compared to traditional chemotherapy.
- Patient outcomes have significantly improved with targeted therapy.
- A leukemia diagnosis now triggers a personalized treatment plan.
Understanding Childhood Leukemia
It’s important to know about childhood leukemia to find better treatments. This cancer affects the blood and bone marrow. It happens when abnormal white blood cells grow too much.
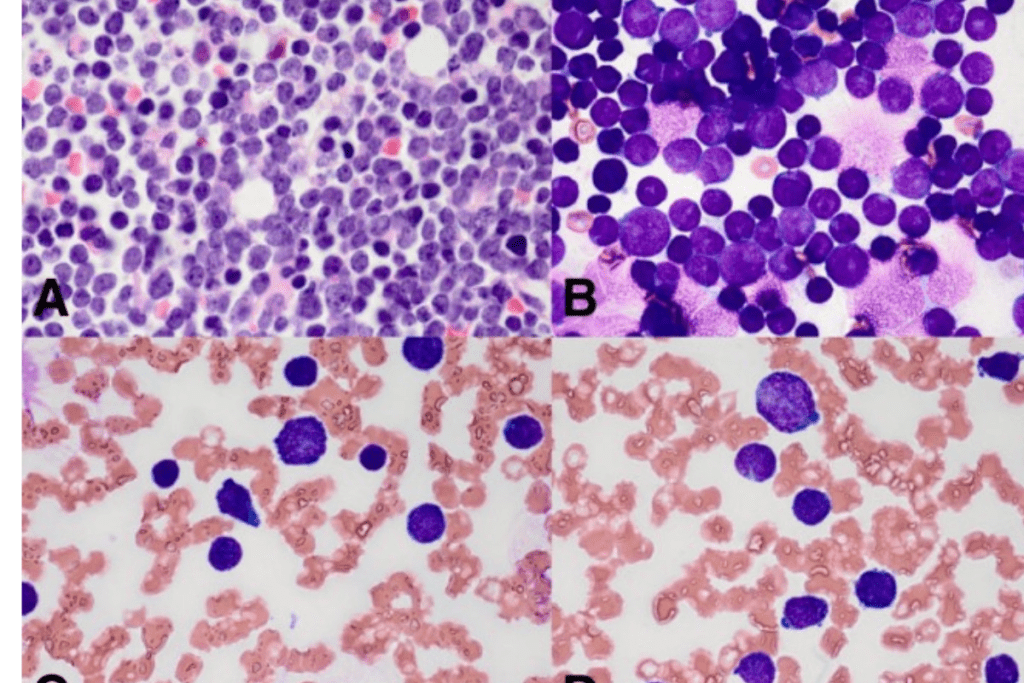
Types of Childhood Leukemia
Children can get different types of leukemia. The most common are Acute Lymphoblastic Leukemia (ALL) and Acute Myeloid Leukemia (AML). ALL is found in about 80% of cases, and AML in 15-20%. There are also rarer types like Chronic Myeloid Leukemia (CML) and Juvenile Myelomonocytic Leukemia (JMML).
- Acute Lymphoblastic Leukemia (ALL)
- Acute Myeloid Leukemia (AML)
- Chronic Myeloid Leukemia (CML)
- Juvenile Myelomonocytic Leukemia (JMML)
Global Prevalence and Statistics
Worldwide, leukemia is a big problem in kids. It makes up 33% of all new cancer cases in children. In fact, 31% of kids under 15 who die from cancer have leukemia.
The rates of leukemia vary around the world. They are higher in places like North America and Europe. Thanks to better treatments, more kids are surviving leukemia.
- Incidence rates are higher in North America and Europe.
- Mortality rates have decreased significantly due to advancements in treatment.
- Survival rates vary based on the type of leukemia and geographical location.
We need to keep working on treatments for childhood leukemia. Knowing how common it is helps doctors, researchers, and leaders plan better. This way, we can help more kids fight and win against leukemia.
Traditional Treatment Approaches
Childhood leukemia treatment has changed over time. These changes have made treatments better for kids. Now, we have a mix of therapies that fit each child’s needs.
Chemotherapy: The Foundation of Treatment
Chemotherapy is key in treating childhood leukemia. It uses drugs to kill cancer cells. The type of chemotherapy depends on the leukemia type and the child’s health.
- Chemotherapy targets fast-growing cells, like cancer cells.
- Doctors often use more than one drug to work better.
- Side effects can be big, so kids need extra care.
Radiation Therapy Applications
Radiation therapy is used in some cases of childhood leukemia. It uses high-energy rays to kill cancer cells.
Key applications include:
- It treats leukemia in the brain.
- It gets kids ready for stem cell transplants by removing cancer cells.
Even though it works, doctors use radiation therapy carefully because of possible long-term side effects.

Stem Cell Transplantation Procedures
Stem cell transplantation is a big help for some kids with leukemia. It’s for those with high-risk or relapsed disease. The goal is to replace the sick bone marrow with healthy stem cells.
“Stem cell transplantation offers a potentially curative approach for children with high-risk leukemia, providing a new immune system capable of fighting the disease.”
The process includes:
- Pre-transplant conditioning to get rid of the sick bone marrow
- Infusion of donor or autologous stem cells.
- Post-transplant care to manage complications and prevent relapse.
In conclusion, traditional treatments like chemotherapy, radiation therapy, and stem cell transplantation are very important for kids with leukemia. Knowing about these treatments helps doctors create better care plans.
The Evolution of How to Treat Childhood Leukemia
Medical science has made huge strides in treating childhood leukemia. This has brought new hope to patients and their families. The journey to treat this disease has seen many milestones, from the first treatments to today’s precision medicine.
Historical Treatment Protocols
In the mid-20th century, chemotherapy started being used to treat childhood leukemia. Early protocols were tough and had many side effects. But they were the start of something better.
Over time, these treatments got better. They became more focused on the disease and included more care for the patient.
The use of combination chemotherapy was a big step forward. It helped more kids survive and opened the door for more research.
Breakthrough Advancements
Childhood leukemia treatment has seen big changes thanks to breakthrough advancements. Targeted therapies are a big part of this. They aim to attack the disease directly, with less harm to healthy cells.
Immunotherapy has also made a big impact. Treatments like CAR T-cell therapy are showing great promise. They use the body’s immune system to fight cancer, which could lead to better treatments.
Shift Toward Precision Medicine
The move to precision medicine is a big step forward. It means treatments are tailored to each patient’s needs. This approach uses a deep understanding of the disease to find the best treatments.
Genomic profiling and other advanced tests have been key. They help doctors find the right treatments by looking at genetic and molecular details. This leads to better care for patients.
Fundamentals of Targeted Therapy
Targeted therapy has changed how we treat childhood leukemia. It focuses on the ways cancer cells grow.
Definition and Core Principles
Targeted therapy uses drugs that target specific molecules in cancer cells. It works by blocking the ways cancer cells grow and survive.
Precision medicine is key to targeted therapy. It means treatments are made just for each patient’s cancer. This makes treatments work better and have fewer side effects.
Molecular Basis of Targeted Approaches
Targeted therapy works by finding and targeting specific genetic changes or proteins in cancer. Knowing a patient’s molecular profile helps doctors choose the right treatment.
Comparison with Traditional Chemotherapy
Unlike traditional chemotherapy, targeted therapy only hits cancer cells. This means it’s safer for healthy cells and causes fewer side effects.
- Targeted therapy offers a more precise treatment approach.
- It reduces the harm to normal cells compared to traditional chemotherapy.
- The therapy is tailored to the molecular characteristics of the patient’s cancer.
Types of Targeted Therapies for Pediatric Leukemia
Targeted therapy is changing how we treat pediatric leukemia. It offers more precise and effective care. Unlike old chemotherapy, these therapies target cancer cells directly, harming fewer healthy cells.
Tyrosine Kinase Inhibitors
Tyrosine kinase inhibitors are showing great promise in treating pediatric leukemia. They block enzymes called tyrosine kinases that help cancer cells grow. Imatinib is a notable example, used to treat certain leukemias.
- Block tyrosine kinases, enzymes critical for cancer cell growth.
- Have shown effectiveness in treating specific leukemias.
- Can be combined with other therapies to boost results.
Monoclonal Antibodies
Monoclonal antibodies are another targeted therapy for pediatric leukemia. These antibodies are made to target specific proteins on cancer cells. This marks them for destruction by the immune system. Rituximab is an example used in leukemia treatments.
- Target specific proteins on cancer cells.
- Mark cancer cells for destruction by the immune system.
- It can be used alone or with other treatments.
Proteasome Inhibitors
Proteasome inhibitors, like bortezomib, block the proteasome. This is a complex in cells that breaks down proteins. Blocking it leads to an accumulation of defective proteins, causing cell death, mainly in cancer cells.
- Inhibit the proteasome, causing an accumulation of defective proteins.
- It can induce cell death in cancer cells.
- Used in treating certain leukemias.
BCL-2 Inhibitors
BCL-2 inhibitors target the BCL-2 protein, which controls cell death. By inhibiting BCL-2, these therapies promote apoptosis in cancer cells. Venetoclax is a BCL-2 inhibitor used in treating certain leukemias.
- Target the BCL-2 protein to promote apoptosis.
- It can be effective in treating specific leukemias.
- Often used with other therapies.
In conclusion, various targeted therapies are being used to treat pediatric leukemia. Each has its own way of working and benefits. Understanding these therapies is key to creating effective treatment plans.
Immunotherapy as Targeted Treatment
Immunotherapy is a new way to fight childhood leukemia. It uses the body’s immune system to target cancer cells. This method is less harsh than traditional treatments.
CAR T-Cell Therapy
CAR T-Cell Therapy changes T-cells to attack cancer. It’s shown great promise in treating leukemia. Clinical trials have seen high success rates.
First, T-cells are taken from the patient. Then, they’re changed to find and kill leukemia cells. After that, these modified T-cells are put back into the patient.
Bispecific T-Cell Engagers
Bispecific T-Cell Engagers (BiTEs) are a new type of treatment. They connect T-cells to leukemia cells. This helps T-cells kill cancer cells better.
BiTEs have worked well in trials, even when other treatments failed. They’re a strong tool against leukemia.
Immune Checkpoint Inhibitors
Immune Checkpoint Inhibitors let the immune system fight cancer better. They’re being tested in childhood leukemia. So far, they show promise.
These inhibitors remove the brakes on the immune system. This lets the body fight cancer more effectively. More research is needed to see how safe and effective they are for kids with leukemia.
In summary, immunotherapy, including CAR T-Cell Therapy, bispecific T-cell engagers, and immune checkpoint inhibitors, is a big step forward in treating childhood leukemia. As research grows, these treatments could greatly improve outcomes for kids with leukemia.
Clinical Evidence and Treatment Outcomes
Clinical trials have shown that targeted therapies are effective for kids with leukemia. Studies have found a big drop in relapse risk when these therapies are used.
Recent Clinical Trial Results
Many trials have looked into the safety and success of targeted therapies in kids with leukemia. For example, one trial found a 61% reduction in relapse risk with a mix of targeted therapies and chemotherapy.
These trials show that targeted therapies can hit leukemia cells hard but spare healthy cells. This means fewer side effects for patients.
Long-Term Outcome Studies
Long-term studies have also backed up the good results of targeted therapies in treating leukemia in kids. These studies follow patients for years to see how well they do.
These studies show that kids treated with targeted therapies often live longer and face fewer long-term side effects.
Quality of Life Improvements
Targeted therapies have also made life better for kids with leukemia. They help reduce the need for harsh chemotherapy and lessen side effects. This means kids can enjoy life more during and after treatment.
Parents and doctors say kids on targeted therapy have fewer hospital stays. They can also do more normal kid stuff with less trouble.
Side Effects and Management
Targeted therapies are becoming more common in treating childhood leukemia. It’s important to know about their side effects for effective management. These therapies often have fewer side effects than traditional chemotherapy.
Common Side Effects of Targeted Therapies
Even though targeted therapies are more precise, they can cause side effects. Common issues include:
- Skin rashes and other skin problems
- Fatigue and feeling unwell
- Diarrhea or other stomach issues
- Potential liver enzyme elevations
These side effects are usually less severe than those from traditional chemotherapy. This helps patients maintain a better quality of life during treatment.
Comparison with Traditional Treatment Side Effects
Traditional chemotherapy has many side effects because it affects cells broadly. Targeted therapies, on the other hand, are more specific. This reduces harm to normal cells and side effects. For example:
- Targeted therapies often lead to less severe neutropenia (low white blood cell count) than chemotherapy.
- Patients on targeted therapies usually experience less alopecia (hair loss) and mucositis.
Supportive Care Strategies
Managing side effects is key to the success of targeted therapy. Supportive care strategies are essential. They include:
- Regular monitoring of patients for early signs of side effects
- Proactive management of side effects through medication and lifestyle adjustments
- Patient education on recognizing and reporting side effects
By using these strategies, healthcare providers can reduce the impact of side effects. This ensures patients can continue to benefit from targeted therapies without a big impact on their quality of life.
Global Access and Disparities
There’s a big problem with getting modern treatments for childhood leukemia around the world. The way treatments are spread out means different results in different places.
Regional Variations in Treatment Availability
Where you live affects how easy it is to get treatments for childhood leukemia. In rich countries, getting new treatments is easier than in poor ones. This is because of differences in healthcare, rules, and money.
In low-income countries, getting treatments is hard because they’re expensive and there’s not enough healthcare. But in high-income countries, better healthcare means more people can get these treatments.
Economic Barriers to Targeted Therapies
Money is a big problem in getting treatments for childhood leukemia. The cost of treatments is high, and it’s hard for families to pay.
The costs aren’t just for the medicine. There are also costs for diagnostic testing, hospital stays, and follow-up care. These costs can be too much for many families, making it hard in places with little financial help.
Initiatives to Improve Global Access
There are many efforts to make treatments for childhood leukemia more available worldwide. Groups like international health organizations, governments, and drug companies are working to make treatments cheaper and easier to get.
Some big steps include price cuts, donation programs, and helping healthcare in poor countries. These plans aim to close the gap in getting treatments and help more kids with leukemia get better care.
Conclusion
Targeted therapies and immunotherapies have changed how we treat childhood leukemia. They offer better results and fewer side effects. Targeted therapy is key, giving a precise way to fight the disease.
Breakthroughs in CAR T-cell therapy and other immunotherapies are showing great promise. They are making a big difference in clinical trials. This means we might see even better treatments in the future.
Work is being done to make sure everyone has access to these treatments. This is a big step forward. With continued research, we can make treatments even better and help more kids.
FAQ
What is targeted therapy for childhood leukemia?
Targeted therapy for childhood leukemia uses drugs that target specific cancer cell growth pathways. This approach has fewer side effects than traditional chemotherapy.
What are the types of childhood leukemia?
Childhood leukemia includes two main types: acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML).
How does targeted therapy differ from traditional chemotherapy?
Targeted therapy is more precise. It targets specific molecular pathways used by cancer cells. Traditional chemotherapy, on the other hand, affects both cancerous and healthy cells.
What are tyrosine kinase inhibitors used for in pediatric leukemia?
Tyrosine kinase inhibitors are used to treat certain pediatric leukemia types. They block specific enzymes that cancer cells need to grow.
What is CAR T-Cell Therapy?
CAR T-Cell Therapy is a form of immunotherapy. It modifies a patient’s T-cells to recognize and attack cancer cells.
How do targeted therapies impact the quality of life for patients with childhood leukemia?
Targeted therapies improve quality of life. They reduce side effects and enhance treatment outcomes.
Are there any disparities in access to targeted therapies for childhood leukemia globally?
Yes, there are disparities in access to modern treatments for childhood leukemia. These disparities are due to regional variations and economic barriers.
What are the common side effects of targeted therapies for childhood leukemia?
Targeted therapies generally have fewer side effects than traditional chemotherapy. Yet, they can cause side effects, which vary by treatment.
How have recent clinical trials impacted the treatment of childhood leukemia?
Recent clinical trials have shown significant improvements in treatment outcomes. They have reduced relapse risk when targeted therapies are used.
What initiatives are underway to improve global access to targeted therapies for childhood leukemia?
Various initiatives aim to improve global access. They focus on reducing economic barriers and increasing treatment availability in resource-limited regions.
References
- World Health Organization. (2024). Childhood cancers: key facts. https://www.who.int/news-room/fact-sheets/detail/childhood-cancers-key-facts
- Canadian Cancer Society. (2024). Targeted therapy for childhood leukemia. https://cancer.ca/en/cancer-information/cancer-types/leukemia-childhood/treatment/targeted-therapy
- Haladik, B., & Boztug, K. (2025). Better therapy selection for childhood leukemia using molecular and functional analyses. Center for Molecular Medicine. https://cemm.at/news/detail/better-therapy-selection-for-childhood-leukemia

































