Choosing between ICSI and conventional IVF can be tough for couples. Both are well-known fertility treatments. But, recent studies show they work differently based on your situation. Comparing the fertilization and live birth rates of icsi vs conventional ivf.
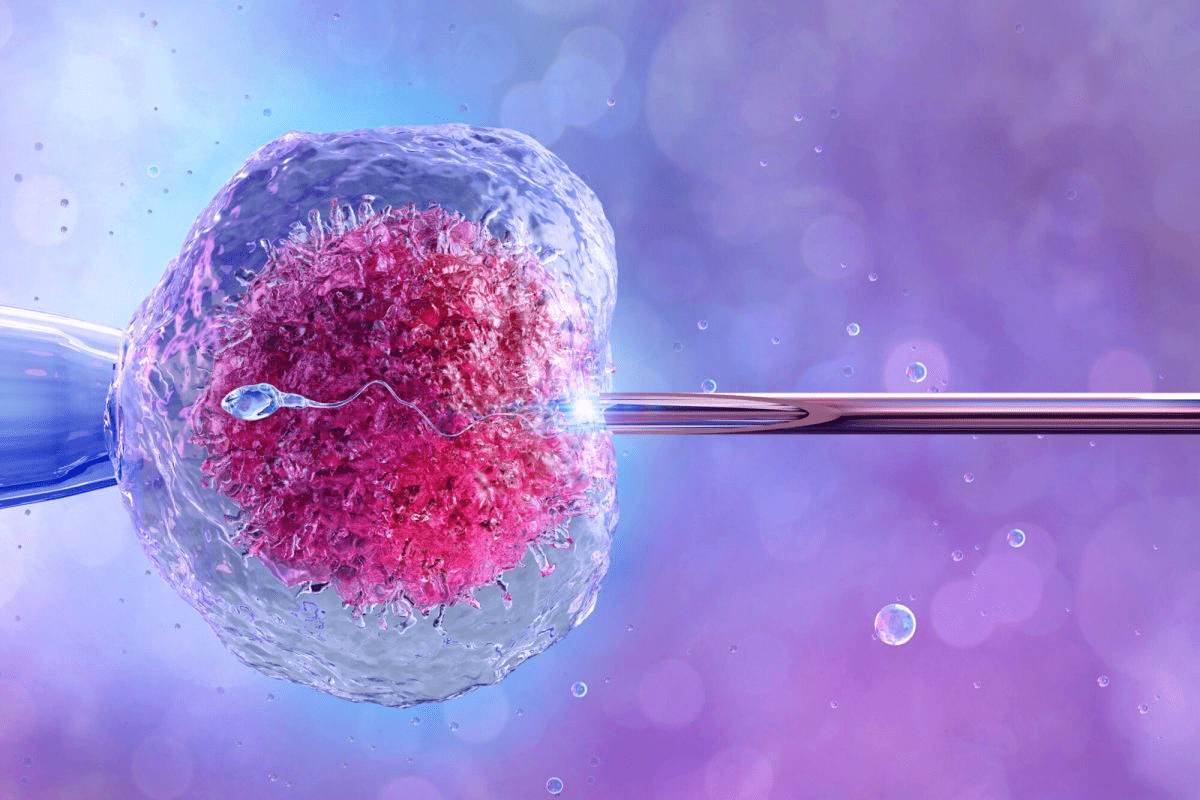
At Liv Hospital, we know it’s key to understand the differences. ICSI injects a single sperm into an egg, skipping natural barriers. Conventional IVF mixes eggs and sperm in a dish for natural fertilization.
ICSI helps couples with male fertility issues. Conventional IVF is better for female fertility problems.
Key Takeaways
- ICSI and conventional IVF are two distinct assisted reproductive technologies.
- The choice between ICSI and conventional IVF depends on individual circumstances.
- ICSI is beneficial for couples with male infertility issues.
- Conventional IVF is often used for female infertility factors.
- Understanding the differences between ICSI and conventional IVF is key for fertility treatment success.
The Fundamentals of Assisted Reproductive Technologies
Understanding assisted reproductive technologies is key for those exploring fertility treatments. These technologies have changed how we treat infertility, giving many options for conception.
ART has seen big improvements over the years. Success rates have gone up, and new treatments have been added. This shows how far fertility treatments have come.
The Evolution of Fertility Treatments
ART started many years ago with conventional IVF. It was one of the first and most well-known methods. Later, new techniques like ICSI (Intracytoplasmic Sperm Injection) were developed to tackle specific fertility issues.
ICSI was a big step forward, helping those with male infertility. It involves directly injecting a sperm into an egg, overcoming natural barriers.
Current Landscape of Fertility Interventions
Now, there are many fertility treatments available. The choice between IVF and ICSI depends on the cause of infertility and past results.
| Treatment Aspect | Conventional IVF | ICSI |
|---|---|---|
| Fertilization Method | Natural fertilization in the lab | Direct sperm injection into the egg |
| Primary Indications | Female factor infertility, unexplained infertility | Male factor infertility, previous IVF failures |
| Success Rate Factors | Age, egg quality, sperm quality | Sperm quality, egg quality, embryologist expertise |
The Growing Importance of Success Rate Transparency
As treatments get better, sharing success rates is more important. Now, patients can find detailed info on treatment effectiveness. This helps them make better choices.
Clinics must now share more about their success rates. This includes fertilisation rate icsi and live birth rates. This openness helps patients understand their chances and pick the best treatment.
Conventional IVF: Process and Methodology
Conventional IVF is a detailed process. It starts with ovarian stimulation and ends with embryo transfer. It’s a proven method that has helped many people conceive.
How Traditional IVF Works
It starts with ovarian stimulation. This is when medications help the ovaries produce more eggs. Then, egg retrieval takes place, where the eggs are collected.
The eggs are then fertilized with sperm in a lab. This process is like natural fertilization.
Ovarian Stimulation: Medications are used to stimulate the ovaries. This increases the chances of successful fertilization and pregnancy.
The Natural-Style Fertilization Process
In conventional IVF, fertilization happens naturally in the lab. Eggs and sperm are mixed together. This closely mimics natural conception.
This natural-style fertilization process is great for those with female infertility issues.
Laboratory Protocols and Embryo Development
After fertilization, embryos are cultured in the lab for 3-5 days. Embryologists watch the embryos’ development. They check if they’re ready for transfer.
| Day | Embryo Development Stage |
|---|---|
| 1 | Fertilization |
| 3 | Cleavage stage |
| 5 | Blastocyst stage |
Ideal Candidates for Conventional IVF
Conventional IVF is best for those with female infertility issues. It’s also good for those who haven’t conceived after trying other treatments.
Knowing how conventional IVF works can help decide if it’s right for you. Comparing it to other treatments like ICSI can guide your choice.
Intracytoplasmic Sperm Injection (ICSI): Advanced Technique
ICSI has changed how we treat male infertility. It involves directly injecting sperm into eggs. This method has greatly improved fertilization rates for those facing fertility challenges.
The ICSI Procedure Explained
The ICSI process starts with egg retrieval from the female partner, similar to IVF. A semen sample is then prepared to pick out individual sperm. An embryologist chooses a sperm and injects it into an egg using a microscope and special tools.
Key steps in the ICSI process include:
- Egg retrieval
- Sperm selection
- Micro-injection of sperm into eggs
- Monitoring of fertilization and embryo development
Direct Sperm Injection Methodology
ICSI’s direct sperm injection method is great for male infertility. It injects a single sperm into an egg, even with low sperm count or motility. This leads to high ICSI fertilization rates.
The precision needed for ICSI is very high. It requires advanced lab tools and skilled embryologists.
Laboratory Requirements and Expertise
ICSI needs a specialized lab with top-notch equipment, like high-powered microscopes. The embryologists must be well-trained and experienced in handling gametes and performing the injection.
“The success of ICSI is heavily dependent on the skill of the embryologist and the quality of the laboratory equipment.” – Expert in Reproductive Medicine
Primary Indications for ICSI Treatment
ICSI is mainly for male factor infertility, like low sperm count or poor motility. It’s also suggested when IVF cycles fail or when sperm need to be surgically retrieved.
The intracytoplasmic sperm injection success rate depends on egg and sperm quality, the female partner’s age, and the lab team’s expertise.
ICSI vs Conventional IVF: Key Differences
ICSI and conventional IVF are two different ways to help with fertility issues. Each has its own benefits and when to use them. Knowing these differences helps patients and doctors make better choices.
Procedural and Technical Distinctions
The main difference is how they help eggs and sperm meet. Conventional IVF mixes eggs and sperm in a dish, letting nature take over. ICSI, on the other hand, injects a single sperm into an egg.
Key procedural differences include:
- The method of fertilization: conventional IVF uses natural fertilization, while ICSI involves manual sperm injection.
- Laboratory requirements: ICSI requires specialized equipment and expertise due to the delicate nature of the procedure.
Bypassing Natural Fertilization Barriers
ICSI is great for couples facing male fertility issues. It helps by directly injecting sperm into the egg. This way, it overcomes problems like low sperm count or poor motility.
The ability to bypass these barriers makes ICSI a valuable option for patients who may not achieve successful fertilization through conventional IVF.
Cost Comparison Between Methods
ICSI and conventional IVF have different costs. ICSI is pricier because of the special tools and skills needed. But, the total cost also depends on the clinic, how many cycles you need, and any extra treatments.
| Treatment | Average Cost | Factors Influencing Cost |
|---|---|---|
| Conventional IVF | $12,000 – $17,000 per cycle | Clinic location, medication, additional treatments |
| ICSI | $13,000 – $20,000 per cycle | Specialized equipment, expertise, additional treatments |
Risk Profiles of Each Approach
Both ICSI and conventional IVF have risks. ICSI might have a higher chance of fertilization failure or egg damage. Conventional IVF risks include ovarian stimulation and multiple pregnancies.
Understanding these risks is essential for patients to make informed decisions about their fertility treatment.
Understanding Success Rate Metrics in Fertility Treatments
When looking into fertility treatments, it’s key to know the success metrics. Success rates in fertility treatments cover many areas. They give a full picture of how well treatments work.
Fertilization Rates vs. Pregnancy Rates
Fertilization rates show how many eggs are fertilized in IVF or ICSI cycles. But, a high fertilization rate doesn’t always mean a successful pregnancy. Pregnancy rates, on the other hand, show how many cycles lead to a clinical pregnancy.
Fertilization rates depend on egg and sperm quality, and the lab’s skill. Pregnancy rates, though, are also influenced by the uterus and embryo quality.
Live Birth Rate as the Ultimate Measure
The live birth rate is the best measure of success in fertility treatments. It shows the percentage of cycles that end in a living child. Live birth rates are the most reliable because they cover the whole treatment process.
Live birth rates give a clear view of the chances of success with fertility treatments. Clinics report live birth rates per cycle, egg retrieval, or embryo transfer. This helps patients understand their chances better.
How Clinics Calculate and Report Success
Fertility clinics report success rates in different ways, making comparisons hard. But, the Society for Assisted Reproductive Technology (SART) and others have set guidelines. These ensure clinics give accurate and comparable data.
- Clinics report success rates based on cycles started, egg retrievals, or embryo transfers.
- Success rates are often broken down by age, diagnosis, and treatment type.
- Some clinics report cumulative success rates, showing chances of a live birth over multiple cycles.
The Impact of Patient Demographics on Statistics
Patient demographics, like age and medical history, greatly affect success rates. Younger patients usually have better success rates with IVF and ICSI. Knowing how demographics affect success helps set realistic expectations.
Clinics often give success rate data by age and other demographic factors. This helps patients understand their chances better.
ICSI Success Rates Across Different Patient Populations
ICSI success rates change a lot depending on the patient. Things like age and why someone can’t get pregnant play big roles. Knowing this helps both patients and doctors make better choices about treatment.
Overall Fertilization Success
ICSI is very good at helping people get pregnant, with success rates over 70%. It’s a big help for men who have trouble getting their sperm to the egg. This method lets a single sperm get injected into the egg, skipping over usual barriers.
Fertilization rates are key to seeing if ICSI is working. But, high fertilization rates don’t always mean a baby will be born.
Live Birth Rates by Age Group
Age really matters when it comes to ICSI success. Live birth rates go down as women get older, after 35. Women under 35 do better with ICSI than older women.
| Age Group | Live Birth Rate (%) |
|---|---|
| <35 | 40-50 |
| 35-37 | 30-40 |
| 38-40 | 20-30 |
| >40 | 10-20 |
Outcomes for Male Factor Infertility Cases
ICSI was made to help men with fertility problems, and it works well. For men with severe fertility issues, ICSI gives them a better chance of getting pregnant than regular IVF.
ICSI helps men with low sperm count or poor sperm movement. This makes it a big success in treating male infertility.
Results for Non-Male Factor Indications
ICSI is not just for men with fertility problems. It’s also used for other reasons like unexplained infertility or failed IVF tries. Success rates can vary, and each case is looked at individually.
For reasons other than male infertility, ICSI’s benefits are not always clear. Egg quality and number are more important for success in these cases.
Conventional IVF Success Rates and Outcomes
Conventional IVF success depends on many things, like age and fertility issues. Knowing these factors helps us set realistic goals and choose the right fertility treatment.
Average Fertilization Rates
Fertilization rates show how well IVF works. Average rates are between 60% to 70%. But, they can change based on egg and sperm quality and lab methods.
Age-Stratified Live Birth Rates
Age greatly affects IVF success. Live birth rates drop a lot after 35. Women under 35 might see a 40-50% live birth rate per cycle. But, for women over 40, it’s around 10% or less.
Impact of Specific Fertility Diagnoses
The type of fertility issue also matters. Some issues, like tubal problems or unexplained infertility, have better success rates. But, severe male issues or low egg count can make it harder.
Multiple Cycle Cumulative Success Rates
Success rates over several cycles give a clearer view of IVF’s effectiveness. Studies show cumulative live birth rates can hit up to 80% or more after three to four cycles for some patients. This gives hope to those needing multiple treatments.
Understanding these factors helps us deal with the challenges of conventional IVF. It lets us make better choices about our fertility treatment.
When to Choose ICSI vs Conventional IVF
Choosing between ICSI and conventional IVF can be tough. It’s important to know when each is best. We’ll look at what makes the decision easier for patients and doctors.
Evidence-Based Indications for ICSI
ICSI is best for severe male infertility. This includes low sperm count or poor sperm movement. It’s also used when sperm are hard to get or when IVF hasn’t worked well before.
ICSI directly puts a sperm into an egg. This helps couples with certain fertility problems.
Scenarios Where Conventional IVF May Be Preferable
Conventional IVF is better for non-male infertility causes. This includes tubal damage or endometriosis. This method lets eggs naturally get fertilized by multiple sperm.
The Role of Previous Treatment History
What treatments you’ve had before affects your choice. If IVF didn’t work well before, ICSI might be suggested next. But, if conventional IVF worked, you might stick with it.
Physician and Patient Decision-Making Process
Doctors and patients decide together on ICSI or conventional IVF. They consider the infertility cause, the couple’s age, and past results. It’s key to talk openly about the risks and benefits of each option.
The right choice between ICSI and conventional IVF depends on your situation. Knowing the benefits and when to use each helps make a smart choice for your fertility treatment.
Conclusion: Navigating Your Fertility Treatment Options
Finding the right fertility treatment can be tough with so many options. Knowing the difference between ICSI and conventional IVF helps. This knowledge lets people make better choices for their health.
ICSI and conventional IVF are both good ways to help with fertility problems. ICSI is best for men with fertility issues. Conventional IVF works for more types of fertility problems. Knowing how well each works helps choose the right one.
This guide aims to clear up the confusion around these treatments. It helps people make smart decisions about their fertility. By understanding each treatment’s strengths, patients can work with doctors to find the best option for them.
FAQ
What is the difference between ICSI and conventional IVF?
ICSI directly injects sperm into eggs, skipping natural barriers. Conventional IVF mixes eggs and sperm in a dish, mimicking nature.
What are the success rates of ICSI compared to conventional IVF?
Success rates for ICSI and conventional IVF depend on age, sperm quality, and infertility causes. ICSI often has higher fertilization rates, helping with male infertility.
When is ICSI recommended over conventional IVF?
ICSI is suggested for male infertility, like low sperm count. It’s also used when conventional IVF fails.
What are the key factors influencing ICSI success rates?
Woman’s age, sperm quality, and infertility causes are key factors for ICSI success.
How do conventional IVF success rates compare across different age groups?
IVF success drops with age, more so after 35, due to egg quality and quantity decline.
What is the impact of specific fertility diagnoses on conventional IVF success rates?
Certain conditions like endometriosis or PCOS can impact IVF success, needing specific treatments.
How are success rates calculated and reported by fertility clinics?
Clinics use fertilization, pregnancy, and live birth rates to calculate success. These rates can vary based on patient and treatment details.
What is the role of previous treatment history in deciding between ICSI and conventional IVF?
Past treatment results, successes or failures, help choose between ICSI and conventional IVF, tailoring treatment to each person.
Are there any differences in the risk profiles of ICSI and conventional IVF?
Both ICSI and conventional IVF have similar risks, like multiple pregnancies and OHSS. Risks can vary based on individual cases.
How do ICSI fertilization rates compare to conventional IVF fertilization rates?
ICSI usually has better fertilization rates than conventional IVF, which is important for male infertility.
What is the significance of live birth rates in evaluating the success of fertility treatments?
Live birth rates are the best measure of fertility treatment success, showing the number of successful births.
References
National Center for Biotechnology Information. ICSI vs. Conventional IVF: Success Rate Considerations. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9650435/